Dement Neurocogn Disord.
2016 Dec;15(4):93-102. 10.12779/dnd.2016.15.4.93.
Primary Progressive Aphasia and the Left Hemisphere Language Network
- Affiliations
-
- 1Cognitive Neurology and Alzheimer's Disease Center, Northwestern University Feinberg School of Medicine Chicago, IL, USA. mmesulam@northwestern.edu
- KMID: 2442833
- DOI: http://doi.org/10.12779/dnd.2016.15.4.93
Abstract
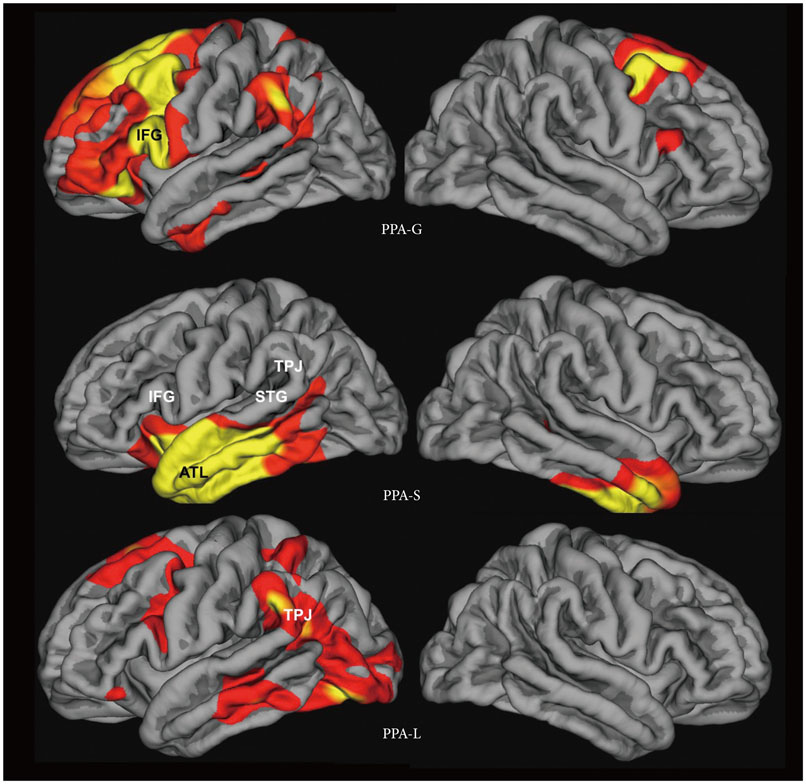
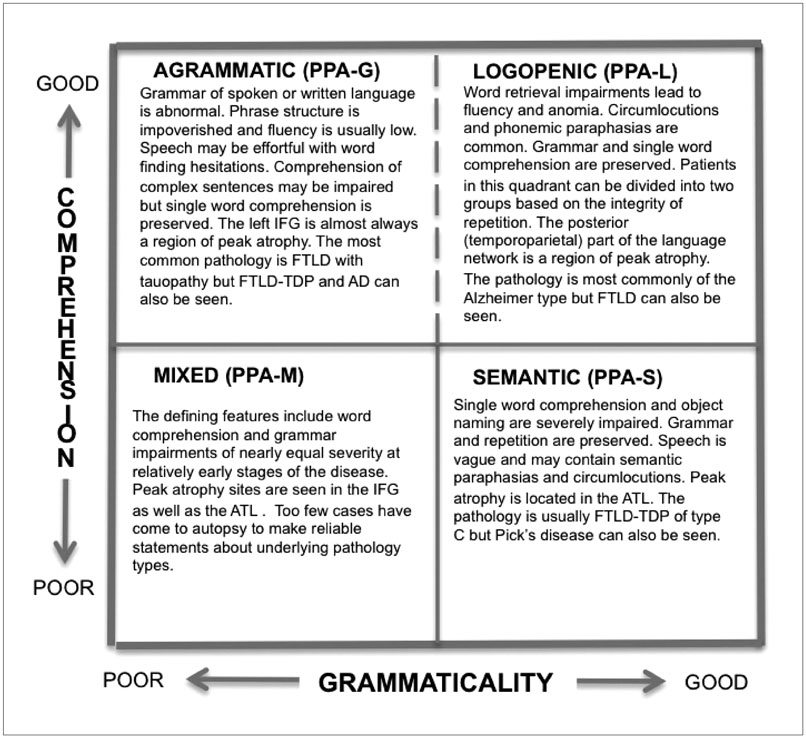
- Primary progressive aphasia (PPA) is a clinical syndrome diagnosed when three core criteria are met. First, there should be a language impairment (i.e., aphasia) that interferes with the usage or comprehension of words. Second, the neurological work-up should determine that the disease is neurodegenerative, and therefore progressive. Third, the aphasia should arise in relative isolation, without equivalent deficits of comportment or episodic memory. The language impairment can be fluent or non-fluent and may or may not interfere with word comprehension. Memory for recent events is preserved although memory scores obtained in verbally mediated tests may be abnormal. This distinctive clinical pattern is most conspicuous in the initial stages of the disease, and reflects a relatively selective atrophy of the language network, usually located in the left hemisphere. There are different clinical variants of PPA, each with a characteristic pattern of atrophy. Clinicoanatomical correlations in patient with these variants have led to new insights on the organization of the large-scale language network in the human brain. For example, the left anterior temporal lobe, which was not part of the classic language network, has been shown to play a critical role in word comprehension and object naming. Furthermore, patients with PPA have shown that fluency can be dissociated from grammaticality. The underlying neuropathological diseases are heterogeneous and can include Alzheimer's disease as well as frontotemporal lobar degeneration. The clinician's task is to recognize PPA and differentiate it from other neurodegenerative phenotypes, use biomarkers to surmise the nature of the underlying neuropathology, and institute the most fitting multimodal interventions.
Keyword
MeSH Terms
Figure
Reference
-
1. Mesulam M. Primary progressive aphasia–differentiation from Alzheimer’s disease. Annals of neurology. 1987; 22:533–534.
Article2. Gorno-Tempini ML, Hillis AE, Weintraub S, Kertesz A, Mendez M, Cappa SF, et al. Classification of primary progressive aphasia and its variants. Neurology. 2011; 76:1006–1014.
Article3. Murray LL, Paek EJ. Behavioral/nonpharmacological approaches to addressing cognitive-linguistic symptoms in individuals with dementia. Perspect ASHA Spec Interest Groups. 2016; 1:12–25.
Article4. Croot K, Nickels L, Laurence F, Manning M. Impairment–and activity/participation-directed interventions in progressive language impairment: clinical and theoretical issues. Aphasiology. 2009; 23:125–160.
Article5. Farrajota L, Maruta C, Maroco J, Martins IP, Guerreiro M, de Mendonça A. Speech therapy in primary progressive aphasia: a pilot study. Dement Geriatr Cogn Dis Extra. 2012; 2:321–331.
Article6. Mesulam MM, Weintraub S, Rogalski EJ, Wieneke C, Geula C, Bigio EH. Asymmetry and heterogeneity of Alzheimer’s and frontotemporal pathology in primary progressive aphasia. Brain. 2014; 137(Pt 4):1176–1192.
Article7. Rogalski E, Sridhar J, Rader B, Martersteck A, Chen K, Cobia D, et al. Aphasic variant of Alzheimer disease: clinical, anatomic, and genetic features. Neurology. 2016; 87:1337–1343.8. Mesulam M. Primary progressive aphasia. Ann Neurol. 2001; 49:425–432.
Article9. Wicklund AH, Johnson N, Weintraub S. Preservation of reasoning in primary progressive aphasia: further differentiation from Alzheimer’s disease and the behavioral presentation of frontotemporal dementia. J Clin Exp Neuropsychol. 2004; 26:347–355.
Article10. Weintraub S, Rogalski E, Shaw E, Sawlani S, Rademaker A, Wieneke C, et al. Verbal and nonverbal memory in primary progressive aphasia: the Three Words-Three Shapes Test. Behav Neurol. 2013; 26:67–76.
Article11. Weintraub S, Rubin NP, Mesulam MM. Primary progressive aphasia. Longitudinal course, neuropsychological profile, and language features. Arch Neurol. 1990; 47:1329–1335.
Article12. Josephs KA, Duffy JR, Strand EA, Machulda MM, Senjem ML, Master AV, et al. Characterizing a neurodegenerative syndrome: primary progressive apraxia of speech. Brain. 2012; 135(Pt 5):1522–1536.
Article13. Mesulam MM, Weintraub S. Primary progressive aphasia and kindred disorders. In : Duyckaerts C, Litvan I, editors. Handbook of Clinical Neurology. New York: Elsevier;2008. p. 573–587.14. Mesulam MM, Wieneke C, Thompson C, Rogalski E, Weintraub S. Quantitative classification of primary progressive aphasia at early and mild impairment stages. Brain. 2012; 135(Pt 5):1537–1553.
Article15. Mesulam M, Weintraub S, Parrish T, Gitelman D. Primary progressive aphasia: reversed asymmetry of atrophy and right hemisphere language dominance. Neurology. 2005; 64:556–557.
Article16. Demirtas-Tatlidede A, Gurvit H, Oktem-Tanor O, Emre M. Crossed aphasia in a dextral patient with logopenic/phonological variant of primary progressive aphasia. Alzheimer Dis Assoc Disord. 2012; 26:282–284.
Article17. Catani M, Piccirilli M, Cherubini A, Tarducci R, Sciarma T, Gobbi G, et al. Axonal injury within language network in primary progressive aphasia. Ann Neurol. 2003; 53:242–247.
Article18. Catani M, Mesulam MM, Jakobsen E, Malik F, Martersteck A, Wieneke C, et al. A novel frontal pathway underlies verbal fluency in primary progressive aphasia. Brain. 2013; 136(Pt 8):2619–2628.
Article19. D'Anna L, Mesulam MM, Thiebaut de Schotten M, Dell'Acqua F, Murphy D, Wieneke C, et al. Frontotemporal networks and behavioral symptoms in primary progressive aphasia. Neurology. 2016; 86:1393–1399.20. Dunn LA, Dunn LM. Peabody Picture Vocabulary Test-4. 4th ed. Minneapolis: Pearson;2006.21. Mesulam M, Rogalski E, Wieneke C, Cobia D, Rademaker A, Thompson C, et al. Neurology of anomia in the semantic variant of primary progressive aphasia. Brain. 2009; 132(Pt 9):2553–2565.
Article22. Kaplan E, Goodglass H, Weintraub S. Boston naming test. . Philadelphia: Lea & Febiger;1983.23. Howard D, Patterson K. Pyramids and palm trees: a test of semantic access from pictures and words. Bury St. Edmunds, Suffolk: Thames Valley Test Company;1992.24. Thompson CK. Northwestern Assessment of Verbs and Sentences (NAVS). cited 2016 May 3. Available from: http://flintbox.com/public/project/9299.25. Weintraub S, Mesulam MM, Wieneke C, Rademaker A, Rogalski EJ, Thompson CK. The northwestern anagram test: measuring sentence production in primary progressive aphasia. Am J Alzheimers Dis Other Demen. 2009; 24:408–416.
Article26. Thompson CK, Weintraub S, Mesulam MM. The Northwestern Anagram Test (NAT). cited 2016 May 3. Available from: http://flintbox.com/public/project/19927.27. Mesulam MM, Wieneke C, Hurley R, Rademaker A, Thompson CK, Weintraub S, et al. Words and objects at the tip of the left temporal lobe in primary progressive aphasia. Brain. 2013; 136(Pt 2):601–618.
Article28. Mesulam M, Wieneke C, Rogalski E, Cobia D, Thompson C, Weintraub S. Quantitative template for subtyping primary progressive aphasia. Arch Neurol. 2009; 66:1545–1551.
Article29. Mesulam MM, Weintraub S. Is it time to revisit the classification guidelines for primary progressive aphasia? Neurology. 2014; 82:1108–1109.
Article30. Geschwind N. Language and the brain. Sci Am. 1972; 226:76–83.
Article31. Sonty SP, Mesulam MM, Thompson CK, Johnson NA, Weintraub S, Parrish TB, et al. Primary progressive aphasia: PPA and the language network. Ann Neurol. 2003; 53:35–49.
Article32. Sonty SP, Mesulam MM, Weintraub S, Johnson NA, Parrish TB, Gitelman DR. Altered effective connectivity within the language network in primary progressive aphasia. J Neurosci. 2007; 27:1334–1345.
Article33. Mesulam MM, Rogalski EJ, Wieneke C, Hurley RS, Geula C, Bigio EH, et al. Primary progressive aphasia and the evolving neurology of the language network. Nat Rev Neurol. 2014; 10:554–569.
Article34. Vandenbulcke M, Peeters R, Van Hecke P, Vandenberghe R. Anterior temporal laterality in primary progressive aphasia shifts to the right. Ann Neurol. 2005; 58:362–370.
Article35. Mesulam MM, Thompson CK, Weintraub S, Rogalski EJ. The Wernicke conundrum and the anatomy of language comprehension in primary progressive aphasia. Brain. 2015; 138(Pt 8):2423–2437.
Article36. Seckin M, Mesulam MM, Voss JL, Huang W, Rogalski EJ, Hurley RS. Am I looking at a cat or a dog? Gaze in the semantic variant of primary progressive aphasia is subject to excessive taxonomic capture. J Neurolinguistics. 2016; 37:68–81.
Article37. Hurley RS, Paller KA, Rogalski EJ, Mesulam MM. Neural mechanisms of object naming and word comprehension in primary progressive aphasia. J Neurosci. 2012; 32:4848–4855.
Article38. Hurley RS, Wang X, Mesulam MM. Asymmetric physiology of the perisylvian language network: evidence from resting state fMRI. J Cogn Neurosci. 2013; 2013:194.39. Tyrrell PJ, Warrington EK, Frackowiak RS, Rossor MN. Progressive degeneration of the right temporal lobe studied with positron emission tomography. J Neurol Neurosurg Psychiatry. 1990; 53:1046–1050.
Article40. Neary D, Snowden JS, Gustafson L, Passant U, Stuss D, Black S, et al. Frontotemporal lobar degeneration: a consensus on clinical diagnostic criteria. Neurology. 1998; 51:1546–1554.
Article41. Gorno-Tempini ML, Brambati SM, Ginex V, Ogar J, Dronkers NF, Marcone A, et al. The logopenic/phonological variant of primary progressive aphasia. Neurology. 2008; 71:1227–1234.
Article42. Thompson CK, Cho S, Hsu CJ, Wieneke C, Rademaker A, Weitner BB, et al. Dissociations between fluency and agrammatism in primary progressive aphasia. Aphasiology. 2012; 26:20–43.
Article43. Rogalski E, Cobia D, Harrison TM, Wieneke C, Thompson CK, Weintraub S, et al. Anatomy of language impairments in primary progressive aphasia. J Neurosci. 2011; 31:3344–3350.
Article44. Mackenzie IR, Neumann M, Bigio EH, Cairns NJ, Alafuzoff I, Kril J, et al. Nomenclature and nosology for neuropathologic subtypes of frontotemporal lobar degeneration: an update. Acta Neuropathol. 2010; 119:1–4.
Article45. Gefen T, Gasho K, Rademaker A, Lalehzari M, Weintraub S, Rogalski E, et al. Clinically concordant variations of Alzheimer pathology in aphasic versus amnestic dementia. Brain. 2012; 135(Pt 5):1554–1565.
Article46. Harris JM, Gall C, Thompson JC, Richardson AM, Neary D, du Plessis D, et al. Classification and pathology of primary progressive aphasia. Neurology. 2013; 81:1832–1839.
Article47. Knibb JA, Xuereb JH, Patterson K, Hodges JR. Clinical and pathological characterization of progressive aphasia. Ann Neurol. 2006; 59:156–165.
Article48. Mesulam M, Wicklund A, Johnson N, Rogalski E, Léger GC, Rademaker A, et al. Alzheimer and frontotemporal pathology in subsets of primary progressive aphasia. Ann Neurol. 2008; 63:709–719.
Article49. Mandell AM, Alexander MP, Carpenter S. Creutzfeldt-Jakob disease presenting as isolated aphasia. Neurology. 1989; 39:55–58.
Article50. Rohrer JD, Geser F, Zhou J, Gennatas ED, Sidhu M, Trojanowski JQ, et al. TDP-43 subtypes are associated with distinct atrophy patterns in frontotemporal dementia. Neurology. 2010; 75:2204–2211.
Article51. Mackenzie IR, Neumann M, Baborie A, Sampathu DM, Du Plessis D, Jaros E, et al. A harmonized classification system for FTLD-TDP pathology. Acta Neuropathol. 2011; 122:111–113.
Article52. Dickerson BC, Bakkour A, Salat DH, Feczko E, Pacheco J, Greve DN, et al. The cortical signature of Alzheimer’s disease: regionally specific cortical thinning relates to symptom severity in very mild to mild AD dementia and is detectable in asymptomatic amyloid-positive individuals. Cereb Cortex. 2009; 19:497–510.
Article53. Rogalski E, Johnson N, Weintraub S, Mesulam M. Increased frequency of learning disability in patients with primary progressive aphasia and their first-degree relatives. Arch Neurol. 2008; 65:244–248.
Article54. Rogalski EJ, Rademaker A, Wieneke C, Bigio EH, Weintraub S, Mesulam MM. Association between the prevalence of learning disabilities and primary progressive aphasia. JAMA Neurol. 2014; 71:1576–1577.
Article55. Martersteck A, Murphy C, Rademaker A, Wieneke C, Weintraub S, Chen K, et al. Is in vivo amyloid distribution asymmetric in primary progressive aphasia? Ann Neurol. 2016; 79:496–501.
Article56. Bigio EH, Mishra M, Hatanpaa KJ, White CL 3rd, Johnson N, Rademaker A, et al. TDP-43 pathology in primary progressive aphasia and frontotemporal dementia with pathologic Alzheimer disease. Acta Neuropathol. 2010; 120:43–54.
Article57. Josephs KA, Whitwell JL, Tosakulwong N, Weigand SD, Murray ME, Liesinger AM, et al. TAR DNA-binding protein 43 and pathological subtype of Alzheimer’s disease impact clinical features. Ann Neurol. 2015; 78:697–709.
Article58. Dickerson BC. Quantitating severity and progression in primary progressive aphasia. J Mol Neurosci. 2011; 45:618–628.
Article59. Rogalski E, Cobia D, Harrison TM, Wieneke C, Weintraub S, Mesulam MM. Progression of language decline and cortical atrophy in subtypes of primary progressive aphasia. Neurology. 2011; 76:1804–1810.
Article60. Chawluk JB, Mesulam MM, Hurtig H, Kushner M, Weintraub S, Saykin A, et al. Slowly progressive aphasia without generalized dementia: studies with positron emission tomography. Ann Neurol. 1986; 19:68–74.
Article61. Trebbastoni A, Raccah R, de Lena C, Zangen A, Inghilleri M. Repetitive deep transcranial magnetic stimulation improves verbal fluency and written language in a patient with primary progressive aphasia-logopenic variant (LPPA). Brain Stimul. 2013; 6:545–553.
Article