J Cardiovasc Imaging.
2019 Apr;27(2):93-101. 10.4250/jcvi.2019.27.e16.
Patients with Isolated Focal Right Ventricular Dyskinetic Segments: Toward a Better Understanding of This Cohort
- Affiliations
-
- 1Division of Cardiology, Faculty of Medical Sciences, Lebanese University, Hadath, Lebanon.
- 2Division of Cardiovascular Medicine, Clemenceau Medical Center, Beirut, Lebanon. wjaroudi@hotmail.com
- 3Department of Radiology, Clemenceau Medical Center, Beirut, Lebanon.
- KMID: 2442742
- DOI: http://doi.org/10.4250/jcvi.2019.27.e16
Abstract
- BACKGROUND
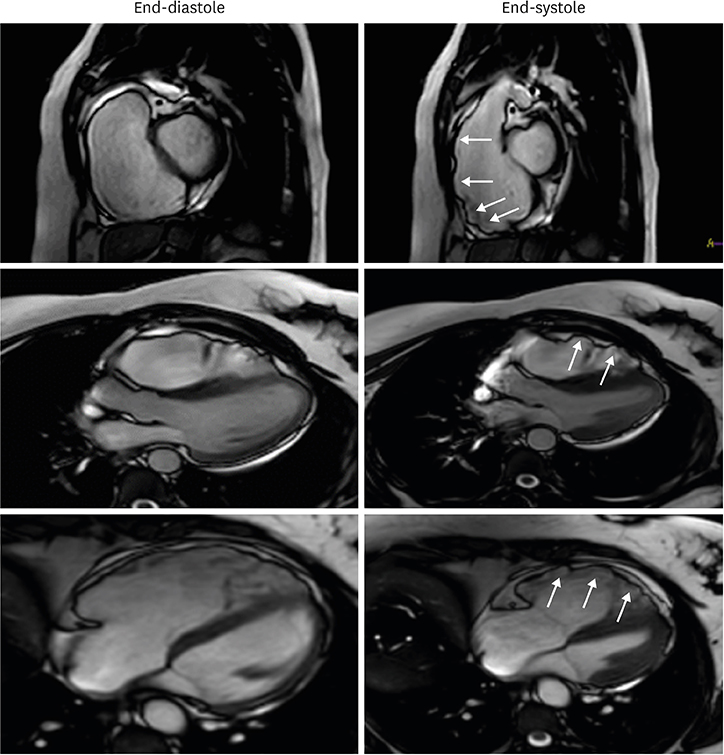
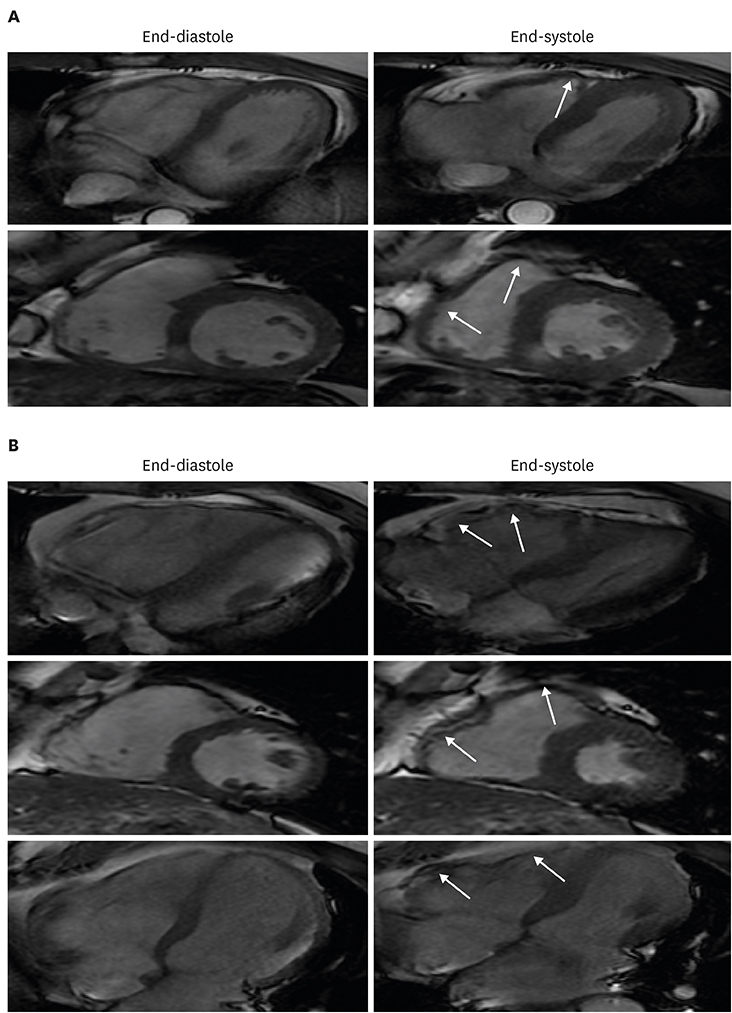
The 2010 revised Task Force criteria for the diagnosis of arrhythmogenic right ventricular cardiomyopathy (ARVC) provided guidance for the classification of patients as definitive, borderline or possible ARVC. However, many patients with clinical suspicion for ARVC have isolated RV dyskinetic segments only and partly meet cardiac magnetic resonance (CMR) imaging criteria. This subgroup of patients and the implication of this imaging finding remain not well defined.
METHODS
There were 65 consecutive patients with clinical suspicion for ARVC who were referred for CMR between 2015 and 2017. The presence of fatty infiltration and fibrosis were assessed using T2 imaging and myocardial delayed enhancement sequences, respectively. RV wall motions, volumes and ejection fraction (EF) of all patients were re-analysed and quantified. Available data on family history, Holter findings, and electrocardiograms were also reviewed.
RESULTS
There were 5 patients (7.7%) that fulfilled major CMR criteria for ARVC: 4 were classified as having definitive ARVC; and 1/5 as borderline. There were 33 patients with no RV dyskinetic segments: none were classified as having definitive or borderline ARVC; 4/33 were classified as possible ARVC, leaving 29/33 as normal or no ARVC. Finally, there were 27 remaining patients (41.5%) with isolated RV dyskinetic segments: 1/27 was classified as definitive ARVC; 4/27 as borderline; 8/27 as possible; leaving 15/27 as indeterminate. Compared to control, those with isolated RV dyskinesia (including the subgroup labelled as indeterminate 15/27) had more abnormal RVEF, larger RV end-diastolic volume index (82 ± 12 mL/m² vs. 72 ± 12 mL/m², p-value 0.0127), and a trend for higher odds of dilated RV (odds ratio 3.0 [0.81-11], p-value 0.09).
CONCLUSIONS
Among patients with a clinical suspicion for ARVC, almost 40% had isolated focal RV dyskinetic segments with the majority remaining unclassified. This cohort had more RV dilation and abnormal EF compared to control.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Comparison of CMR Findings according to the Presence or Absence of Isolated Focal Right Ventricular Dyskinetic Segments in Patients with Clinical Suspicion of ARVC
Sung Min Ko
J Cardiovasc Imaging. 2019;27(2):102-104. doi: 10.4250/jcvi.2019.27.e24.
Reference
-
1. Haugaa KH, Haland TF, Leren IS, Saberniak J, Edvardsen T. Arrhythmogenic right ventricular cardiomyopathy, clinical manifestations, and diagnosis. Europace. 2016; 18:965–972.
Article2. te Riele AS, Tandri H, Bluemke DA. Arrhythmogenic right ventricular cardiomyopathy (ARVC): cardiovascular magnetic resonance update. J Cardiovasc Magn Reson. 2014; 16:50.
Article3. Borgquist R, Haugaa KH, Gilljam T, et al. The diagnostic performance of imaging methods in ARVC using the 2010 Task Force criteria. Eur Heart J Cardiovasc Imaging. 2014; 15:1219–1225.
Article4. Marcus FI, McKenna WJ, Sherrill D, et al. Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia: proposed modification of the Task Force Criteria. Eur Heart J. 2010; 31:806–814.5. Perazzolo Marra M, Rizzo S, Bauce B, et al. Arrhythmogenic right ventricular cardiomyopathy. Contribution of cardiac magnetic resonance imaging to the diagnosis. Herz. 2015; 40:600–606.6. Femia G, Hsu C, Singarayar S, et al. Impact of new task force criteria in the diagnosis of arrhythmogenic right ventricular cardiomyopathy. Int J Cardiol. 2014; 171:179–183.
Article7. Rachoin R, Saleh BA, Mansour B, Rachwan RJ, AlJaroudi W. Arrhythmogenic ventricular cardiomyopathy and sudden cardiac death: Left or right? J Nucl Cardiol. 2017; 24:527–533.
Article8. Elmaghawry M, Alhashemi M, Zorzi A, Yacoub MH. A global perspective of arrhythmogenic right ventricular cardiomyopathy. Glob Cardiol Sci Pract. 2013; 2012:81–92.
Article9. Basso C, Corrado D, Marcus FI, Nava A, Thiene G. Arrhythmogenic right ventricular cardiomyopathy. Lancet. 2009; 373:1289–1300.
Article10. Sen-Chowdhry S, Morgan RD, Chambers JC, McKenna WJ. Arrhythmogenic cardiomyopathy: etiology, diagnosis, and treatment. Annu Rev Med. 2010; 61:233–253.
Article11. Rastegar N, Burt JR, Corona-Villalobos CP, et al. Cardiac MR findings and potential diagnostic pitfalls in patients evaluated for arrhythmogenic right ventricular cardiomyopathy. Radiographics. 2014; 34:1553–1570.
Article12. Bluemke DA, Krupinski EA, Ovitt T, et al. MR imaging of arrhythmogenic right ventricular cardiomyopathy: morphologic findings and interobserver reliability. Cardiology. 2003; 99:153–162.
Article13. Bomma C, Rutberg J, Tandri H, et al. Misdiagnosis of arrhythmogenic right ventricular dysplasia/cardiomyopathy. J Cardiovasc Electrophysiol. 2004; 15:300–306.
Article14. Quick S, Speiser U, Kury K, Schoen S, Ibrahim K, Strasser R. Evaluation and classification of right ventricular wall motion abnormalities in healthy subjects by 3-tesla cardiovascular magnetic resonance imaging. Neth Heart J. 2015; 23:64–69.
Article15. Sievers B, Addo M, Franken U, Trappe HJ. Right ventricular wall motion abnormalities found in healthy subjects by cardiovascular magnetic resonance imaging and characterized with a new segmental model. J Cardiovasc Magn Reson. 2004; 6:601–608.
Article16. Liu T, Pursnani A, Sharma UC, et al. Effect of the 2010 task force criteria on reclassification of cardiovascular magnetic resonance criteria for arrhythmogenic right ventricular cardiomyopathy. J Cardiovasc Magn Reson. 2014; 16:47.
Article17. Vermes E, Strohm O, Otmani A, Childs H, Duff H, Friedrich MG. Impact of the revision of arrhythmogenic right ventricular cardiomyopathy/dysplasia task force criteria on its prevalence by CMR criteria. JACC Cardiovasc Imaging. 2011; 4:282–287.
Article18. Cox MG, van der Smagt JJ, Noorman M, et al. Arrhythmogenic right ventricular dysplasia/cardiomyopathy diagnostic task force criteria: impact of new task force criteria. Circ Arrhythm Electrophysiol. 2010; 3:126–133.19. Femia G, Sy RW, Puranik R. Systematic review: Impact of the new task force criteria in the diagnosis of arrhythmogenic right ventricular cardiomyopathy. Int J Cardiol. 2017; 241:311–317.
Article20. Hamid MS, Norman M, Quraishi A, et al. Prospective evaluation of relatives for familial arrhythmogenic right ventricular cardiomyopathy/dysplasia reveals a need to broaden diagnostic criteria. J Am Coll Cardiol. 2002; 40:1445–1450.
Article21. Smiseth OA, Torp H, Opdahl A, Haugaa KH, Urheim S. Myocardial strain imaging: how useful is it in clinical decision making? Eur Heart J. 2016; 37:1196–1207.
Article22. Prati G, Vitrella G, Allocca G, et al. Right ventricular strain and dyssynchrony assessment in arrhythmogenic right ventricular cardiomyopathy: cardiac magnetic resonance feature-tracking study. Circ Cardiovasc Imaging. 2015; 8:e003647. discussion e003647.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of CMR Findings according to the Presence or Absence of Isolated Focal Right Ventricular Dyskinetic Segments in Patients with Clinical Suspicion of ARVC
- Echocardiographic Detection of Left Ventricular Asynergy by Apical Rotational Transducer Approach in Ischemic Heart Disease
- Isolated Noncompaction of Ventricular Myocardium: a Magnetic Resonance Imaging Study of 11 Patients
- Left Ventricular Imaging by Power Motion Imaging Technique
- Successful Catheter Ablation of Focal Automatic Left Ventricular Tachycardia Presented with Tachycardia-Mediated Cardiomyopathy