Infect Chemother.
2016 Dec;48(4):334-337. 10.3947/ic.2016.48.4.334.
A Case of Transverse Myelitis Caused by Varicella Zoster Virus in an Immunocompetent Older Patient
- Affiliations
-
- 1Deparment of Internal Medicine, Pusan National University School of Medicine, Medical Research Institute, Pusan National University Hospital, Busan, Korea. zzanmery@gmail.com
- KMID: 2441329
- DOI: http://doi.org/10.3947/ic.2016.48.4.334
Abstract
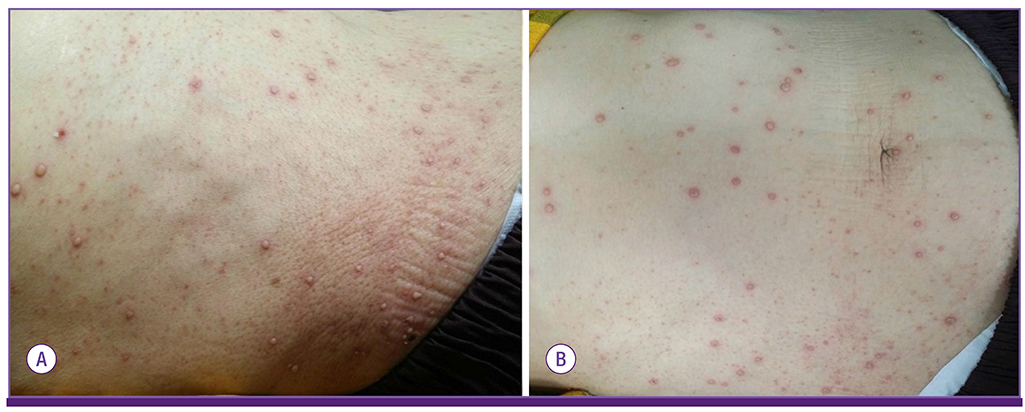
- Varicella zoster virus (VZV) is a human neurotropic alphaherpesvirus that causes chickenpox (varicella) in children. VZV reactivation may lead to neurological complications, including transverse myelitis. However, transverse myelitis caused by VZV reactivation is rare in immunocompetent patients. Herein, we report a case of transverse myelitis caused by VZV in an immunocompetent older patient, and confirmed this case by polymerase chain reaction. A 79-year-old woman visited our service with complaints of weakness in the right lower leg, generalized vesicular eruptions, and throbbing pain in the right flank for ten days. Spine MRI showed transverse myelitis in the thoracic spine at level T4-T11. The patient was treated with acyclovir and her neurological functions improved, except for sensory impairment below level T10. For older patients, early and aggressive antiviral treatment against VZV may be necessary even though these patients are immunocompetent.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Tuberculous Meningitis-Mimicking Varicella-Zoster Meningitis
Sun In Hong, Taeeun Kim, Jiwon Jung, Se Yoon Park, Yong Pil Chong, Sang-Oh Lee, Sang-Ho Choi, Yang Soo Kim, Jun Hee Woo, Sang-Ahm Lee, Sung-Han Kim
Infect Chemother. 2017;49(2):123-129. doi: 10.3947/ic.2017.49.2.123.
Reference
-
1. Gilden DH, Kleinschmidt-DeMasters BK, LaGuardia JJ, Mahalingam R, Cohrs RJ. Neurologic complications of the reactivation of varicella-zoster virus. N Engl J Med. 2000; 342:635–645.
Article2. Gilden D, Nagel MA, Cohrs RJ, Mahalingam R. The variegate neurological manifestations of varicella zoster virus infection. Curr Neurol Neurosci Rep. 2013; 13:374.
Article3. Amlie-Lefond C, Jubelt B. Neurologic manifestations of varicella zoster virus infections. Curr Neurol Neurosci Rep. 2009; 9:430–434.
Article4. Hung CH, Chang KH, Kuo HC, Huang CC, Liao MF, Tsai YT, Ro LS. Features of varicella zoster virus myelitis and dependence on immune status. J Neurol Sci. 2012; 318:19–24.
Article5. Baik JS, Kim WC, Heo JH, Zheng HY. Recurrent herpes zoster myelitis. J Korean Med Sci. 1997; 12:360–363.
Article6. Han MK, Lee SS, Han SH. Herper zoster myelitis confirmed by detection of varicell-zoster virus DNA using the polymerase chain reaction. J Korean Neurol Assoc. 1996; 14:1067–1071.7. Hwang YM, Lee BI, Chung JW, Ahn JH, Kim KW, Kim DI. A case of herpes zoster myelitis. J Korean Neurol Assoc. 1988; 6:272–277.8. Yang IS, Lim GD, Shin SS. A case of herpes zoster myelitis: a case report. J Korean Pain Soc. 1997; 10:266–269.9. Yi H, Lee Y, Shin HY, Kim SM. Varicella zoster viral myelitis in immunocompetent patient. J Korean Neurol Assoc. 2014; 32:339–341.10. Cohen JI. Clinical practice: Herpes zoster. N Engl J Med. 2013; 369:255–263.11. Takahashi T, Tamura M, Miki K, Yamaguchi M, Kanno A, Nunomura S, Ra C, Tamiya T, Kamei S, Takasu T. Varicella zoster virus myelitis in two elderly patients: diagnostic value of nested polymerase chain reaction assay and antibody index for cerebrospinal fluid specimens. Case Rep Neurol. 2013; 5:81–90.
Article12. Lee CC, Wu JC, Huang WC, Shih YH, Cheng H. Herpes zoster cervical myelitis in a young adult. J Chin Med Assoc. 2010; 73:605–610.
Article13. de Silva SM, Mark AS, Gilden DH, Mahalingam R, Balish M, Sandbrink F, Houff S. Zoster myelitis: improvement with antiviral therapy in two cases. Neurology. 1996; 47:929–931.
Article14. Ong OL, Churchyard AC, New PW. The importance of early diagnosis of herpes zoster myelitis. Med J Aust. 2010; 193:546–547.
Article15. Outteryck O, Deramecourt V, Bombois S, Mackowiak-Cordoliani MA, Pasquier F. VZV-related myelitis: a pathophysiological hypothesis. Rev Neurol (Paris). 2007; 163:89–92.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Acute Transverse Myelitis after Varicella-Zoster Virus Infection in an Immunocompetent Patient: A Case Report
- Varicella Zoster Viral Myelitis in Immunocompetent Patient
- Two cases of varicella zoster meningitis in immunocompetent children
- Two Cases of Herpes Zoster Following Varicella Vaccination in Immunocompetent Young Children: One Case Caused by Vaccine-Strain
- Dysphagia with Unilateral Vocal Cord Paralysis in Herpes Zoster: A Case Report