Korean J Radiol.
2019 Apr;20(4):671-682. 10.3348/kjr.2018.0400.
Distinguishing between Thymic Epithelial Tumors and Benign Cysts via Computed Tomography
- Affiliations
-
- 1Department of Radiology, Seoul National University College of Medicine, Seoul, Korea. yshoka@gmail.com
- 2Department of Radiology, Seoul National University Hospital, Seoul, Korea.
- 3Department of Radiology, Konkuk University School of Medicine, Seoul, Korea.
- 4Department of Radiology, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul, Korea.
- 5Department of Nuclear Medicine, Seoul National University College of Medicine, Seoul National University Hospital, Seoul, Korea.
- 6Institute of Radiation Medicine, Seoul National University Medical Research Center, Seoul, Korea.
- KMID: 2440490
- DOI: http://doi.org/10.3348/kjr.2018.0400
Abstract
OBJECTIVE
To investigate whether computed tomography (CT) and fluorine-18-labeled fluoro-2-deoxy-D-glucose (FDG) positron emission tomography (PET) may be applied to distinguish thymic epithelial tumors (TETs) from benign cysts in the anterior mediastinum.
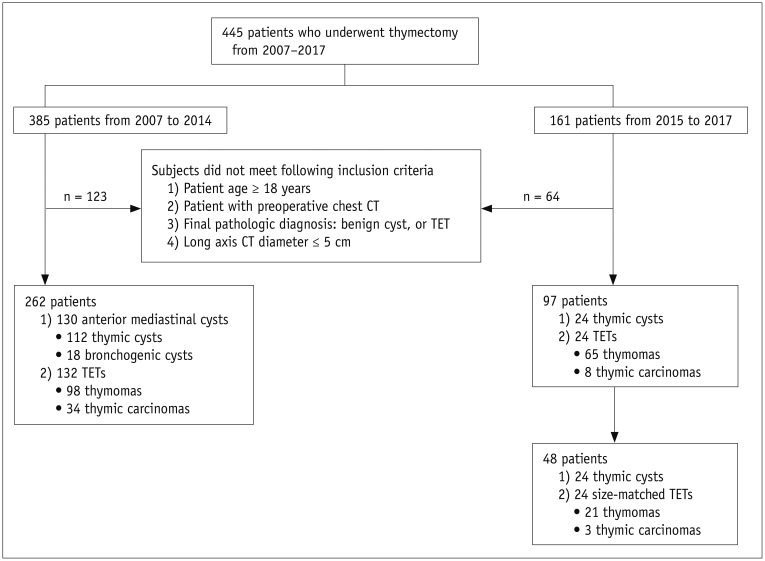
MATERIALS AND METHODS
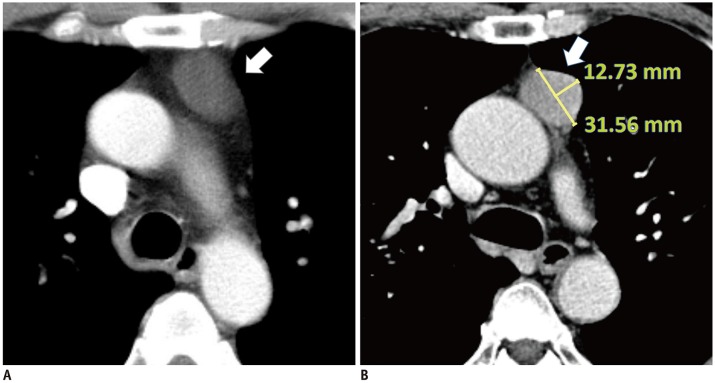
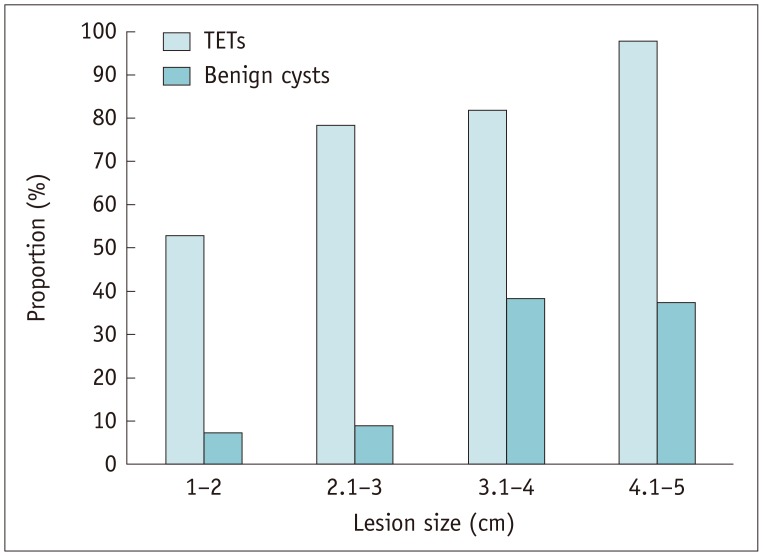
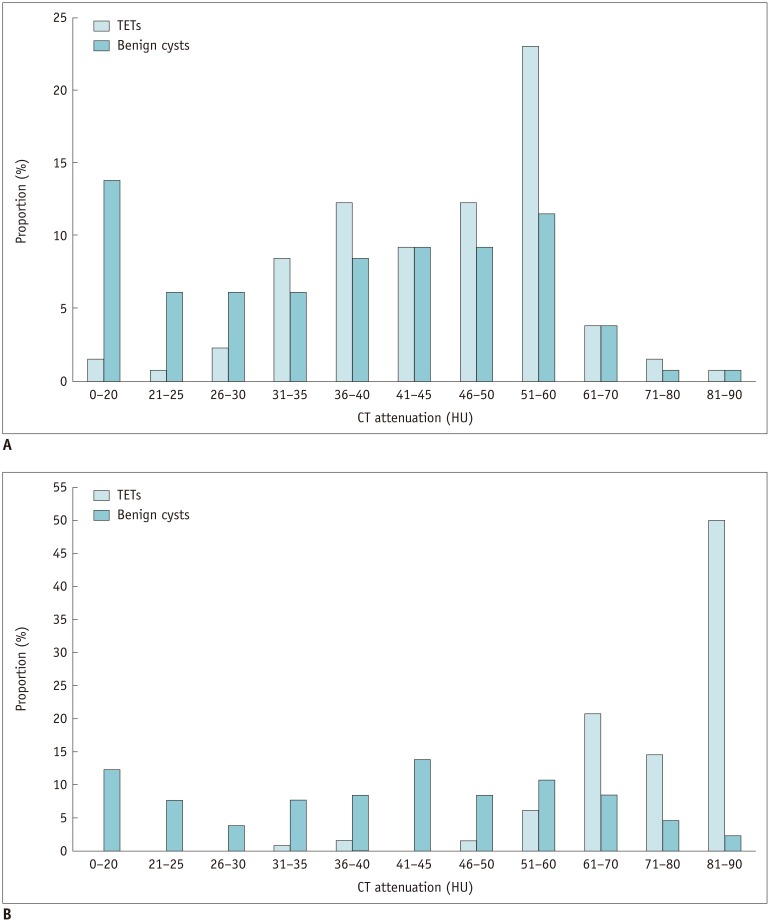
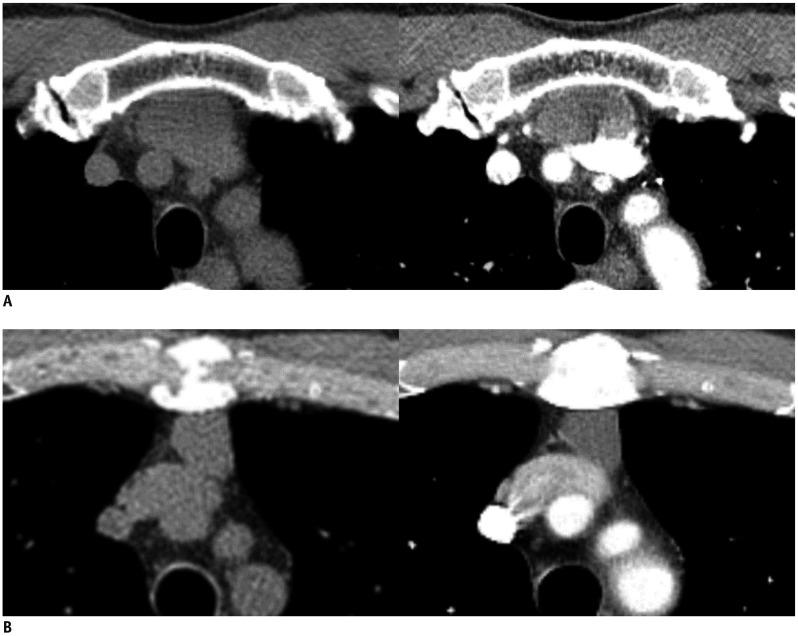
We included 262 consecutive patients with pathologically proven TETs and benign cysts 5 cm or smaller who underwent preoperative CT scans. In addition to conventional morphological and ancillary CT findings, the relationship between the lesion and the adjacent mediastinal pleura was evaluated qualitatively and quantitatively. Mean lesion attenuation was measured on CT images. The maximum standardized uptake value (SUVmax) was obtained with FDG-PET scans in 40 patients. CT predictors for TETs were identified with multivariate logistic regression analysis. For validation, we assessed the diagnostic accuracy and inter-observer agreement between four radiologists in a size-matched set of 24 cysts and 24 TETs using a receiver operating characteristic curve before and after being informed of the study findings.
RESULTS
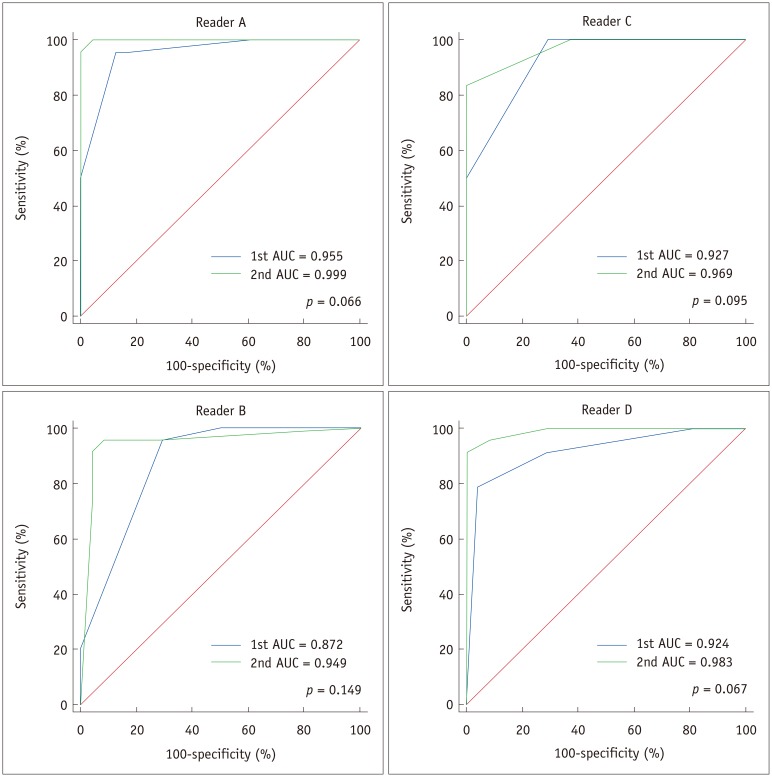
The multivariate analysis showed that post-contrast attenuation of 60 Hounsfield unit or higher (odds ratio [OR], 12.734; 95% confidence interval [CI], 2.506-64.705; p = 0.002) and the presence of protrusion from the mediastinal pleura (OR, 9.855; 95% CI, 1.749-55.535; p = 0.009) were the strongest CT predictors for TETs. SUVmax was significantly higher in TETs than in cysts (5.3 ± 2.4 vs. 1.1 ± 0.3; p < 0.001). After being informed of the study findings, the readers' area under the curve improved from 0.872-0.955 to 0.949-0.999 (p = 0.066-0.149). Inter-observer kappa values for protrusion were 0.630-0.941.
CONCLUSION
Post-contrast CT attenuation, protrusion from the mediastinal pleura, and SUVmax were useful imaging features for distinguishing TETs from cysts in the anterior mediastinum.
Keyword
MeSH Terms
Figure
Reference
-
1. Henschke CI, Lee IJ, Wu N, Farooqi A, Khan A, Yankelevitz D, et al. CT screening for lung cancer: prevalence and incidence of mediastinal masses. Radiology. 2006; 239:586–590. PMID: 16641357.2. Yoon SH, Choi SH, Kang CH, Goo JM. Incidental anterior mediastinal nodular lesions on chest CT in asymptomatic subjects. J Thorac Oncol. 2018; 13:359–366. PMID: 29233791.3. Jeung MY, Gasser B, Gangi A, Bogorin A, Charneau D, Wihlm JM, et al. Imaging of cystic masses of the mediastinum. Radiographics. 2002; 22 Spec No:S79–S93. PMID: 12376602.
Article4. Tomiyama N, Honda O, Tsubamoto M, Inoue A, Sumikawa H, Kuriyama K, et al. Anterior mediastinal tumors: diagnostic accuracy of CT and MRI. Eur J Radiol. 2009; 69:280–288. PMID: 18023547.
Article5. Araki T, Sholl LM, Gerbaudo VH, Hatabu H, Nishino M. Intrathymic cyst: clinical and radiological features in surgically resected cases. Clin Radiol. 2014; 69:732–738. PMID: 24824976.
Article6. Jurado J, Javidfar J, Newmark A, Lavelle M, Bacchetta M, Gorenstein L, et al. Minimally invasive thymectomy and open thymectomy: outcome analysis of 263 patients. Ann Thorac Surg. 2012; 94:974–981. discussion 981-982. PMID: 22748641.
Article7. Ackman JB, Verzosa S, Kovach AE, Louissaint A Jr, Lanuti M, Wright CD, et al. High rate of unnecessary thymectomy and its cause. Can computed tomography distinguish thymoma, lymphoma, thymic hyperplasia, and thymic cysts? Eur J Radiol. 2015; 84:524–553. PMID: 25575742.
Article8. Lococo F. The role of 18F-FDG PET/CT scan in predicting histological type of thymic epithelial tumors: indications and practical clinical considerations. Thorac Cardiovasc Surg. 2018; 66:350–351. PMID: 28728208.
Article9. Shinya T, Tanaka T, Soh J, Matsushita T, Sato S, Toyooka S, et al. Diagnostic value of dual-time-point F-18 FDG PET/CT and chest CT for the prediction of thymic epithelial neoplasms. Acta Med Okayama. 2017; 71:105–112. PMID: 28420891.10. Choi YW, McAdams HP, Jeon SC, Hong EK, Kim YH, Im JG, et al. Idiopathic multilocular thymic cyst: CT features with clinical and histopathologic correlation. AJR Am J Roentgenol. 2001; 177:881–885. PMID: 11566694.11. Maki DD, Birnbaum BA, Chakraborty DP, Jacobs JE, Carvalho BM, Herman GT. Renal cyst pseudoenhancement: beam-hardening effects on CT numbers. Radiology. 1999; 213:468–472. PMID: 10551228.
Article12. Mileto A, Nelson RC, Samei E, Jaffe TA, Paulson EK, Barina A, et al. Impact of dual-energy multi-detector row CT with virtual monochromatic imaging on renal cyst pseudoenhancement: in vitro and in vivo study. Radiology. 2014; 272:767–776. PMID: 24844472.
Article13. Chen G, Marx A, Chen WH, Yong J, Puppe B, Stroebel P, et al. New WHO histologic classification predicts prognosis of thymic epithelial tumors: a clinicopathologic study of 200 thymoma cases from China. Cancer. 2002; 95:420–429. PMID: 12124843.14. Nishino M, Ashiku SK, Kocher ON, Thurer RL, Boiselle PM, Hatabu H. The thymus: a comprehensive review. Radiographics. 2006; 26:335–348. PMID: 16549602.
Article15. Wang X, Chen K, Li X, Li Y, Yang F, Li J, et al. Clinical features, diagnosis and thoracoscopic surgical treatment of thymic cysts. J Thorac Dis. 2017; 9:5203–5211. PMID: 29312727.
Article16. Bae KT, Heiken JP, Siegel CL, Bennett HF. Renal cysts: is attenuation artifactually increased on contrast-enhanced CT images? Radiology. 2000; 216:792–796. PMID: 10966713.
Article17. Birnbaum BA, Hindman N, Lee J, Babb JS. Renal cyst pseudoenhancement: influence of multidetector CT reconstruction algorithm and scanner type in phantom model. Radiology. 2007; 244:767–775. PMID: 17709828.
Article18. Wang ZJ, Coakley FV, Fu Y, Joe BN, Prevrhal S, Landeras LA, et al. Renal cyst pseudoenhancement at multidetector CT: what are the effects of number of detectors and peak tube voltage? Radiology. 2008; 248:910–916. PMID: 18632527.
Article19. Araki T, Sholl LM, Gerbaudo VH, Hatabu H, Nishino M. Imaging characteristics of pathologically proven thymic hyperplasia: identifying features that can differentiate true from lymphoid hyperplasia. AJR Am J Roentgenol. 2014; 202:471–478. PMID: 24555583.
Article20. Levitt RG, Husband JE, Glazer HS. CT of primary germ-cell tumors of the mediastinum. AJR Am J Roentgenol. 1984; 142:73–78. PMID: 6318540.
Article21. Tateishi U, Muller NL, Johkoh T, Onishi Y, Arai Y, Satake M, et al. Primary mediastinal lymphoma: characteristic features of the various histological subtypes on CT. J Comput Assist Tomogr. 2004; 28:782–789. PMID: 15538151.22. McErlean A, Huang J, Zabor EC, Moskowitz CS, Ginsberg MS. Distinguishing benign thymic lesions from early-stage thymic malignancies on computed tomography. J Thorac Oncol. 2013; 8:967–973. PMID: 23608816.
Article23. Sung YM, Lee KS, Kim BT, Choi JY, Shim YM, Yi CA. 18F-FDG PET/CT of thymic epithelial tumors: usefulness for distinguishing and staging tumor subgroups. J Nucl Med. 2006; 47:1628–1634. PMID: 17015898.24. Tatci E, Ozmen O, Dadali Y, Biner IU, Gokcek A, Demirag F, et al. The role of FDG PET/CT in evaluation of mediastinal masses and neurogenic tumors of chest wall. Int J Clin Exp Med. 2015; 8:11146–11152. PMID: 26379916.25. Huang B, Law MW, Khong PL. Whole-body PET/CT scanning: estimation of radiation dose and cancer risk. Radiology. 2009; 251:166–174. PMID: 19251940.
Article26. Daye D, Ackman JB. Characterization of mediastinal masses by MRI: techniques and applications. Appl Radiol. 2017; 46:10–22.27. Zhang W, Zhou Y, Xu XQ, Kong LY, Xu H, Yu TF, et al. A whole-tumor histogram analysis of apparent diffusion coefficient maps for differentiating thymic carcinoma from lymphoma. Korean J Radiol. 2018; 19:358–365. PMID: 29520195.
Article28. Ackman JB, Wu CC. MRI of the thymus. AJR Am J Roentgenol. 2011; 197:W15–W20. PMID: 21700977.
Article29. Ruffini E, Van Raemdonck D, Detterbeck F, Rocco G, Thomas P, Venuta F. Management of thymic tumors: a survey of current practice among members of the European Society of Thoracic Surgeons. J Thorac Oncol. 2011; 6:614–623. PMID: 21266921.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Thymic Cysts: Two cases report
- The Immunoexpression of Ki-67, Bcl-2, p53, and Tyrosine Kinase Receptors in Thymic Epithelial Tumors; Their Correlation with the WHO Histologic Subtypes and the Prognostic Value
- CT Findings of Thymic Epidermoid Cyst in the Anterior Mediastinum: A Case Report and Literature Review
- (18)F-FDG PET/CT is Useful for Pretreatment Assessment of the Histopathologic Type of Thymic Epithelial Tumors
- Cystic Thymic Diseases: CT Manifestations