Korean J Radiol.
2019 Apr;20(4):641-648. 10.3348/kjr.2018.0632.
Coronal Three-Dimensional Magnetic Resonance Imaging for Improving Diagnostic Accuracy for Posterior Ligamentous Complex Disruption In a Goat Spine Injury Model
- Affiliations
-
- 1Department of Radiology, BenQ Medical Center, The Affiliated BenQ Hospital of Nanjing Medical University, Nanjing, China. fskwjc@126.com
- KMID: 2440487
- DOI: http://doi.org/10.3348/kjr.2018.0632
Abstract
OBJECTIVE
The purpose of this study was to investigate whether three-dimensional (3D) magnetic resonance imaging could improve diagnostic accuracy for suspected posterior ligamentous complex (PLC) disruption.
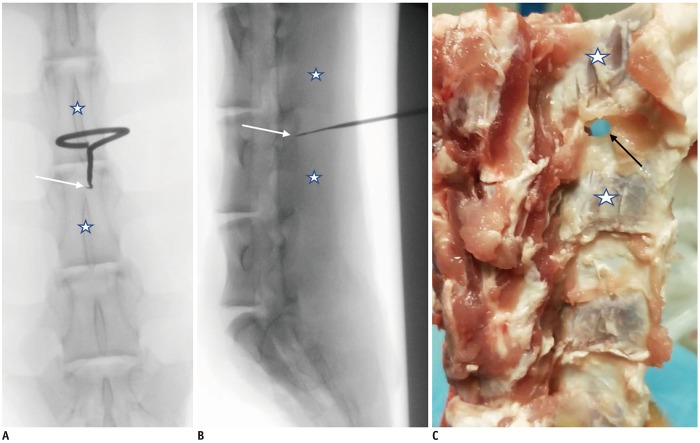
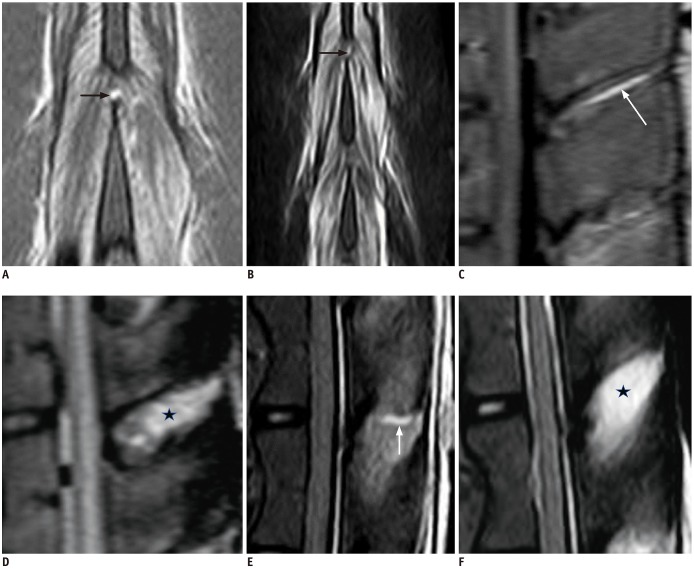
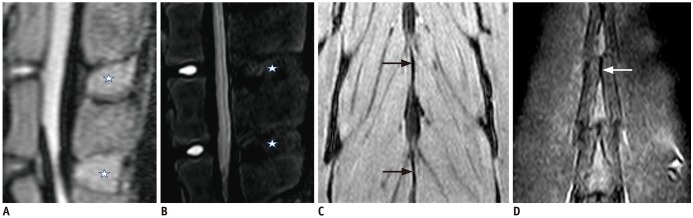
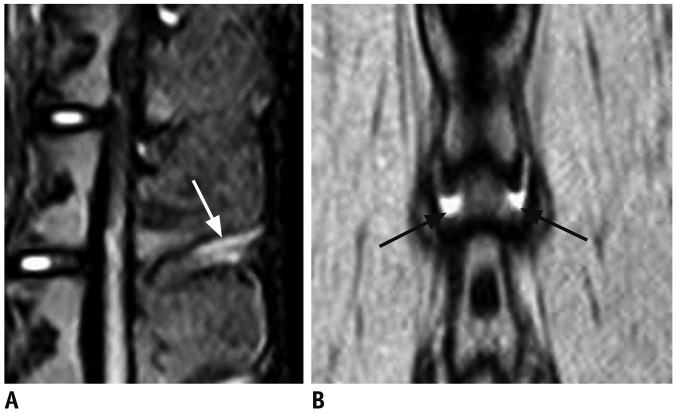
MATERIALS AND METHODS
We used 20 freshly harvested goat spine samples with 60 segments and intact surrounding soft tissue. The animals were aged 1-1.5 years and consisted of 8 males and 12 females, which were sexually mature but had not reached adult weights. We created a paraspinal contusion model by percutaneously injecting 10 mL saline into each side of the interspinous ligament (ISL). All segments underwent T2-weighted sagittal and coronal short inversion time inversion recovery (STIR) scans as well as coronal and sagittal 3D proton density-weighted spectrally selective inversion recovery (3D-PDW-SPIR) scans acquired at 1.5T. Following scanning, some ISLs were cut and then the segments were re-scanned using the same magnetic resonance (MR) techniques. Two radiologists independently assessed the MR images, and the reliability of ISL tear interpretation was assessed using the kappa coefficient. The chi-square test was used to compare the diagnostic accuracy of images obtained using the different MR techniques.
RESULTS
The interobserver reliability for detecting ISL disruption was high for all imaging techniques (0.776-0.949). The sensitivity, specificity, and diagnostic accuracy of the coronal 3D-PDW-SPIR technique for detecting ISL tears were 100, 96.9, and 97.9%, respectively, which were significantly higher than those of the sagittal STIR (p = 0.000), coronal STIR (p = 0.000), and sagittal 3D-PDW-SPIR (p = 0.001) techniques.
CONCLUSION
Compared to other MR methods, coronal 3D-PDW-SPIR provides a more accurate diagnosis of ISL disruption. Adding coronal 3D-PDW-SPIR to a routine MR protocol may help to identify PLC disruptions in cases with nearby contusion.
Keyword
MeSH Terms
Figure
Reference
-
1. Whang PG, Vaccaro AR, Poelstra KA, Patel AA, Anderson DG, Albert TJ, et al. The influence of fracture mechanism and morphology on the reliability and validity of two novel thoracolumbar injury classification systems. Spine (Phila Pa 1976). 2007; 32:791–779. PMID: 17414915.
Article2. Rihn JA, Yang N, Fisher C, Saravanja D, Smith H, Morrison WB, et al. Using magnetic resonance imaging to accurately assess injury to the posterior ligamentous complex of the spine: a prospective comparison of the surgeon and radiologist. J Neurosurg Spine. 2010; 12:391–396. PMID: 20367374.
Article3. James KS, Wenger KH, Schlegel JD, Dunn HK. Biomechanical evaluation of the stability of thoracolumbar burst fractures. Spine (Phila Pa 1976). 1994; 19:1731–1174. PMID: 7973968.
Article4. Oner FC, van Gils AP, Faber JA, Dhert WJ, Verbout AJ. Some complications of common treatment schemes of thoracolumbar spine fractures can be predicted with magnetic resonance imaging: prospective study of 53 patients with 71 fractures. Spine (Phila Pa 1976). 2002; 27:629–663. PMID: 11884911.5. Vaccaro AR, Lehman RA Jr, Hurlbert RJ, Anderson PA, Harris M, Hedlund R, et al. A new classification of thoracolumbar injuries: the importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine (Phila Pa 1976). 2005; 30:2325–2233. PMID: 16227897.6. Savage JW, Moore TA, Arnold PM, Thakur N, Hsu WK, Patel AA, et al. The reliability and validity of the thoracolumbar injury classification system in pediatric spine trauma. Spine. 2015; 40:E1014–E1018. PMID: 26426715.
Article7. Lee HM, Kim HS, Kim DJ, Suk KS, Park JO, Kim NH. Reliability of magnetic resonance imaging in detecting posterior ligament complex injury in thoracolumbar spinal fractures. Spine (Phila Pa 1976). 2000; 25:2079–2208. PMID: 10954639.
Article8. Pizones J, Zúñiga L, Sánchez-Mariscal F, Alvarez P, Gómez-Rice A, Izquierdo E. MRI study of post-traumatic incompetence of posterior ligamentous complex: importance of the supraspinous ligament. Prospective study of 74 traumatic fractures. Eur Spine J. 2012; 21:2222–2223. PMID: 22722921.
Article9. Pizones J, Sánchez-Mariscal F, Zúñiga L, Álvarez P, Izquierdo E. Prospective analysis of magnetic resonance imaging accuracy in diagnosing traumatic injuries of the posterior ligamentous complex of the thoracolumbar spine. Spine (Phila Pa 1976). 2013; 38:745–775. PMID: 23089929.
Article10. Dai LY, Ding WG, Wang XY, Jiang LS, Jiang SD, Xu HZ. Assessment of ligamentous injury in patients with thoracolumbar burst fractures using MRI. J Trauma. 2009; 66:1610–1615. PMID: 19509622.
Article11. Lee JY, Vaccaro AR, Schweitzer KM Jr, Lim MR, Baron EM, Rampersaud R, et al. Assessment of injury to the thoracolumbar posterior ligamentous complex in the setting of normal-appearing plain radiography. Spine J. 2007; 7:422–427. PMID: 17630140.
Article12. Haba H, Taneichi H, Kotani Y, Terae S, Abe S, Yoshikawa H, et al. Diagnostic accuracy of magnetic resonance imaging for detecting posterior ligamentous complex injury associated with thoracic and lumbar fractures. J Neurosurg. 2003; 99(1 Suppl):20–26. PMID: 12859054.
Article13. Crosby CG, Even JL, Song Y, Block JJ, Devin CJ. Diagnostic abilities of magnetic resonance imaging in traumatic injury to the posterior ligamentous complex: the effect of years in training. Spine J. 2011; 11:747–753. PMID: 21840264.
Article14. Van Middendorp JJ, Patel AA, Schuetz M, Joaquim AF. The precision, accuracy and validity of detecting posterior ligamentous complex injuries of the thoracic and lumbar spine: a critical appraisal of the literature. Eur Spine J. 2013; 22:461–474. PMID: 23208081.
Article15. Vaccaro AR, Rihn JA, Saravanja D, Anderson DG, Hilibrand AS, Albert TJ, et al. Injury of the posterior ligamentous complex of the thoracolumbar spine: a prospective evaluation of the diagnostic accuracy of magnetic resonance imaging. Spine (Phila Pa 1976). 2009; 34:E841–E847. PMID: 19927090.16. Pizones J, Izquierdo E, Sánchez-Mariscal F, Zúñiga L, Álvarez P, Gómez-Rice A. Sequential damage assessment of the different components of the posterior ligamentous complex after magnetic resonance imaging interpretation: prospective study 74 traumatic fractures. Spine (Phila Pa 1976). 2012; 37:E662–E667. PMID: 22146288.17. Rihn JA, Fisher C, Harrop J, Morrison W, Yang N, Vaccaro AR. Assessment of the posterior ligamentous complex following acute cervical spine trauma. J Bone Joint Surg Am. 2010; 92:583–589. PMID: 20194316.
Article18. Schweitzer KM, Vaccaro AR, Harrop JS, Hurlbert J, Carrino JA, Rechtine GR, et al. Interrater reliability of identifying indicators of posterior ligamentous complex disruption when plain films are indeterminate in thoracolumbar injuries. J Orthop Sci. 2007; 12:437–442. PMID: 17909928.
Article19. Vaccaro AR, Lee JY, Schweitzer KM Jr, Lim MR, Baron EM, Oner FC, et al. Assessment of injury to the posterior ligamentous complex in thoracolumbar spine trauma. Spine J. 2006; 6:524–528. PMID: 16934721.
Article20. Kim NR, Hong SH, Choi JY, Chang BS, Lee JW, Myung JS, et al. Spreading epidural hematoma and deep subcutaneous edema: indirect MRI signs of posterior ligamentous complex injury in thoracolumbar burst fractures. Skeletal Radiol. 2010; 39:767–772. PMID: 20140731.
Article21. Mi J, Sun XJ, Zhang K, Zhao CQ, Zhao J. Prediction of MRI findings including disc injury and posterior ligamentous complex injury in neurologically intact thoracolumbar burst fractures by the parameters of vertebral body damage on CT scan. Injury. 2018; 49:272–278. PMID: 29290375.
Article22. Rosenthal BD, Boody BS, Jenkins TJ, Hsu WK, Patel AA, Savage JW. Thoracolumbar burst fractures. Clin Spine Surg. 2018; 31:143–151. PMID: 29578877.
Article23. Dawkins RL, Miller JH, Ramadan OI, Lysek MC, Kuhn EN, Rocque BG, et al. Thoracolumbar injury classification and severity score in children: a reliability study. J Neurosurg Pediatr. 2018; 21:284–291. PMID: 29328004.
Article24. Lehman VT, Murthy NS, Diehn FE, Verdoorn JT, Maus TP. The posterior ligamentous complex inflammatory syndrome: spread of fluid and inflammation in the retrodural space of Okada. Clin Radiol. 2015; 70:528–535. PMID: 25577652.
Article25. Li Y, Shen Z, Huang M, Wang X. Stepwise resection of the posterior ligamentous complex for stability of a thoracolumbar compression fracture: an in vitro biomechanical investigation. Medicine (Baltimore). 2017; 96:e7873. PMID: 28858098.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- MRI Findings of Posterior Ligament Complex Injury in Thorcolumbar Bursting Fractures
- Injury of Posterior Ligament Complex with Cervical Spine Fracture
- Evaluation of Diagnostic Accuracy of Magnetic Resonance Imaging in Posterior Ligamentum Complex Injury of Thoracolumbar Spine
- Misdiagnosis of Thoracolumbar Posterior Ligamentous Complex Injuries and Use of Radiographic Parameter Correlations to Improve Detection Accuracy
- Injury of the ligaments of the knee: magnetic resonance evaluation