J Periodontal Implant Sci.
2012 Dec;42(6):256-260.
Differential diagnosis and treatment of periodontitis-mimicking actinomycosis
- Affiliations
-
- 1Department of Periodontics, Seoul St Mary's Hospital, The Catholic University of Korea College of Medicine, Seoul, Korea. ko_y@catholic.ac.kr
Abstract
- PURPOSE
Actinomycosis is an uncommon chronic granulomatous disease that presents as a slowly progressive, indolent, indurated infiltration with multiple abscesses, fistulas, and sinuses. The purpose of this article is to report on a case of actinomycosis with clinical findings similar to periodontitis.
METHODS
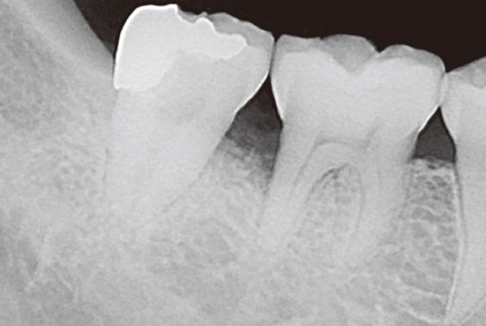
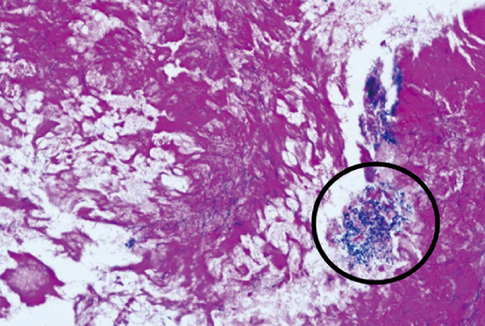
A 46-year-old female presented with recurrent throbbing pain on the right first and second molar of the mandible three weeks after root planing. Exploratory flap surgery was performed, and the bluish-gray tissue fragment found in the interproximal area between the two molars was sent for histopathology.
RESULTS
The diagnosis from the biopsy was actinomycosis. The clinical and radiographic manifestations of this case were clinically indistinguishable from periodontitis. The patient did not report any symptoms, and she is scheduled for a follow-up visit.
CONCLUSIONS
The present study has identified periodontitis-mimicking actinomycosis. Actinomycosis should be included in the differential diagnosis in cases with periodontal pain and inflammation that do not respond to nonsurgical treatment for periodontitis. More routine submissions of tissue removed from the oral cavity for biopsies may be beneficial for differential diagnosis.
Keyword
MeSH Terms
Figure
Reference
-
1. Hirshberg A, Tsesis I, Metzger Z, Kaplan I. Periapical actinomycosis: a clinicopathologic study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003. 95:614–620.
Article2. Nair PN. On the causes of persistent apical periodontitis: a review. Int Endod J. 2006. 39:249–281.
Article3. De D, Dogra S, Kanwar AJ, Saikia UN. Actinomycosis presenting as a destructive ulcerated plaque on the palate and gingiva. J Am Acad Dermatol. 2011. 65:1235–1236.
Article4. Kaplan I, Anavi K, Anavi Y, Calderon S, Schwartz-Arad D, Teicher S, et al. The clinical spectrum of Actinomyces-associated lesions of the oral mucosa and jawbones: correlations with histomorphometric analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009. 108:738–746.
Article5. Crossman T, Herold J. Actinomycosis of the maxilla: a case report of a rare oral infection presenting in general dental practice. Br Dent J. 2009. 206:201–202.
Article6. Sun CX, Henkin JM, Ririe C, Javadi E. Implant failure associated with actinomycosis in a medically compromised patient. J Oral Implantol. 2011. 07. 18. [Epub]. http://dx.doi.org/10.1563/AAID-JOI-D-11-00028.
Article7. Nagler RM, Ben-Arieh Y, Laufer D. Case report of regional alveolar bone actinomycosis: a juvenile periodontitis-like lesion. J Periodontol. 2000. 71:825–829.
Article8. Sakallioglu U, Acikgoz G, Kirtiloglu T, Karagoz F. Rare lesions of the oral cavity: case report of an actinomycotic lesion limited to the gingiva. J Oral Sci. 2003. 45:39–42.
Article9. Brook I. Actinomycosis: diagnosis and management. South Med J. 2008. 101:1019–1023.
Article10. Desai RS, Shetty SJ. The clinical spectrum of Actinomyces-associated lesions of the oral mucosa and jaw bones: a personal experience. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010. 109:657. author reply 657-8.
Article11. Won HR, Park JH, Kim KS. Simultaneous actinomycosis with aspergillosis in maxillary sinus. Br J Oral Maxillofac Surg. 2012. 03. 23. [Epub]. http://dx.doi.org/10.1016/j.bjoms.2012.03.003.
Article12. Choi J, Koh WJ, Kim TS, Lee KS, Han J, Kim H, et al. Optimal duration of IV and oral antibiotics in the treatment of thoracic actinomycosis. Chest. 2005. 128:2211–2217.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Actinomycosis of the right masseter following the extraction of lower third molar
- Abdominal Actinomycosis Mimicking Acute Appendicitis in Children: a Case Report
- Actinomycosis Presenting as a Nasopharyngeal Mass: A Case Report
- A Case of Actinomycosis of Maxillary Sinus
- A Case of Pelvic Actinomycosis Associated with Intrauterine Contraceptive Device