Pediatr Infect Vaccine.
2018 Dec;25(3):170-175. 10.14776/piv.2018.25.e14.
Abdominal Actinomycosis Mimicking Acute Appendicitis in Children: a Case Report
- Affiliations
-
- 1Department of Pediatrics, Hanil General Hospital, Seoul, the Republic of Korea. pedleejin@naver.com
- 2Department of Pathology, Hanil General Hospital, Seoul, the Republic of Korea.
- KMID: 2428255
- DOI: http://doi.org/10.14776/piv.2018.25.e14
Abstract
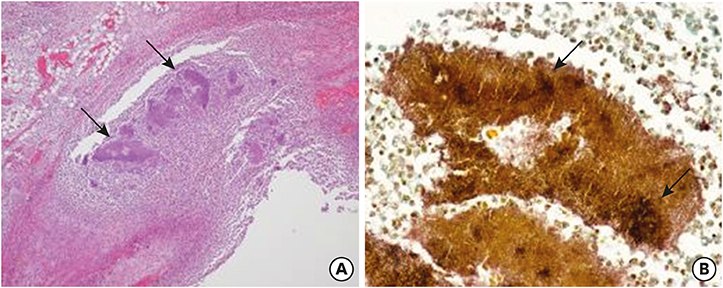
- Actinomyces are anaerobic, Gram-positive bacteria that are part of the endogenous flora of mucous membranes in humans. Infection caused by these bacteria is termed actinomycosis. The 3 most common types of actinomycosis are cervicofacial, abdominopelvic, and pulmonary. A previously healthy 6-year-old boy presented with the emergency room with fever, vomiting, and abdominal pain and initially diagnosed with acute appendicitis. Exploratory laparoscopy was done. Histologic finding demonstrated acute gangrenous appendicitis complicated by perforation and sulfur granules compatible with actinomycosis. Subsequently, he was diagnosed with abdominal actinomycosis and received long-term antibiotic therapy. Abdominal actinomycosis is uncommon in children and difficult to diagnose because of its nonspecific symptoms and of difficulties in growing Actinomyces in the clinical setting. It is necessary to include abdominal actinomycosis as a differential diagnosis of children presenting with abdominal pain.
Keyword
MeSH Terms
Figure
Reference
-
1. Wacharachaisurapol N, Bender JM, Wang L, Bliss D, Ponrartana S, Pannaraj PS. Abdominal actinomycosis in children: a case report and literature review. Pediatr Infect Dis J. 2017; 36:e76–9.2. Shah HR, Williamson MR, Boyd CM, Balachandran S, Angtuaco TL, McConnell JR. CT findings in abdominal actinomycosis. J Comput Assist Tomogr. 1987; 11:466–469.
Article3. Sung HY, Lee IS, Kim SI, Jung SE, Kim SW, Kim SY, et al. Clinical features of abdominal actinomycosis: a 15-year experience of a single institute. J Korean Med Sci. 2011; 26:932–937.
Article4. Davies M, Keddie NC. Abdominal actinomycosis. Br J Surg. 1973; 60:18–22.
Article5. Karateke F, Özyazıcı S, Menekşe E, Daş K, Ozdoğan M. Unusual presentations of actinomycosis; anterior abdominal wall and appendix: report of three cases. Balkan Med J. 2013; 30:315–317.
Article6. Sullivan DC, Chapman SW. Bacteria that masquerade as fungi: actinomycosis/nocardia. Proc Am Thorac Soc. 2010; 7:216–221.
Article7. American Academy of Pediatrics. Actinomycosis. Kimberlin DW, Brady MT, Jackson MA, Long SS, editors. Red book: 2018 report of the committee on infectious diseases. 31st ed. Itasca: American Academy of Pediatrics;2018. p. 205–206.8. Jacobs RF, Schutze GE. Actinomyces. In : Kliegman RM, Stanton BF, St. Geme JW, Schor NF, editors. Nelson textbook of pediatrics. 20th ed. Philadelphia: Elsevier;2016. p. 1352–1354.9. Acquaro P, Tagliabue F, Confalonieri G, Faccioli P, Costa M. Abdominal wall actinomycosis simulating a malignant neoplasm: case report and review of the literature. World J Gastrointest Surg. 2010; 2:247–250.
Article10. Benammar S, Hélardot PG, Sapin E, Adamsbaum C, Raymond J. Childhood actinomycosis: report of two cases. Eur J Pediatr Surg. 1995; 5:180–183.
Article11. Whitworth S, Pence MA, Jacobs RF. Actinomycosis. In : Cherry J, Harrison GJ, Kaplan SL, Steinbach WJ, Hotez PJ, editors. Feigin and Cherry's textbook of pediatric infectious diseases. 8th ed. Philadelphia: Elsevier;2013. p. 1312–1316.12. Miyamoto MI, Fang FC. Pyogenic liver abscess involving Actinomyces: case report and review. Clin Infect Dis. 1993; 16:303–309.13. Kwak JH, Won EJ, Choi EH, Jung SE, Kim HY. Periappendiceal actinomycosis presenting as acute appendicitis. J Korean Assoc Pediatr Surg. 2015; 21:7–10.
Article14. McGowan JE, Steinberg JP. Other gram-negative bacilli. In : Mandell GL, Bennett JE, Dolin R, editors. Mandell, Douglas and Bennett's principles and practices of infectious diseases. New York: Churchill Livingstone;1995. p. 2106–2107.15. Cato EP, Moore WEC, Nygaard G, Holdeman LV. Actinomyces meyeri sp. nov., specific epithet rev. Int J Syst Bacteriol. 1984; 34:487–489.16. Russo TA. Agents of actinomycosis. In : Bennett JE, Dolin R, Blaser MJ, editors. Mandell, Douglas, and Bennett's principles and practice of infectious diseases. 8th ed. Philadelphia: Elsevier;2015. p. 2864–2873.17. Huang CJ, Huang TJ, Hsieh JS. Pseudo-colonic carcinoma caused by abdominal actinomycosis: report of two cases. Int J Colorectal Dis. 2004; 19:283–286.
Article18. Abela J, Sciberras J, Meilak M, Felice AG, Degaetano J. Omental actinomycosis presenting with right lower quadrant abdominal pain. J Clin Pathol. 2004; 57:671.