Intest Res.
2019 Jan;17(1):17-23. 10.5217/ir.2018.00139.
Clinical aspects and treatments for pediatric inflammatory bowel diseases
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Children's Hospital, Seoul National University College of Medicine, Seoul, Korea. mjschj@snu.ac.kr
- KMID: 2438439
- DOI: http://doi.org/10.5217/ir.2018.00139
Abstract
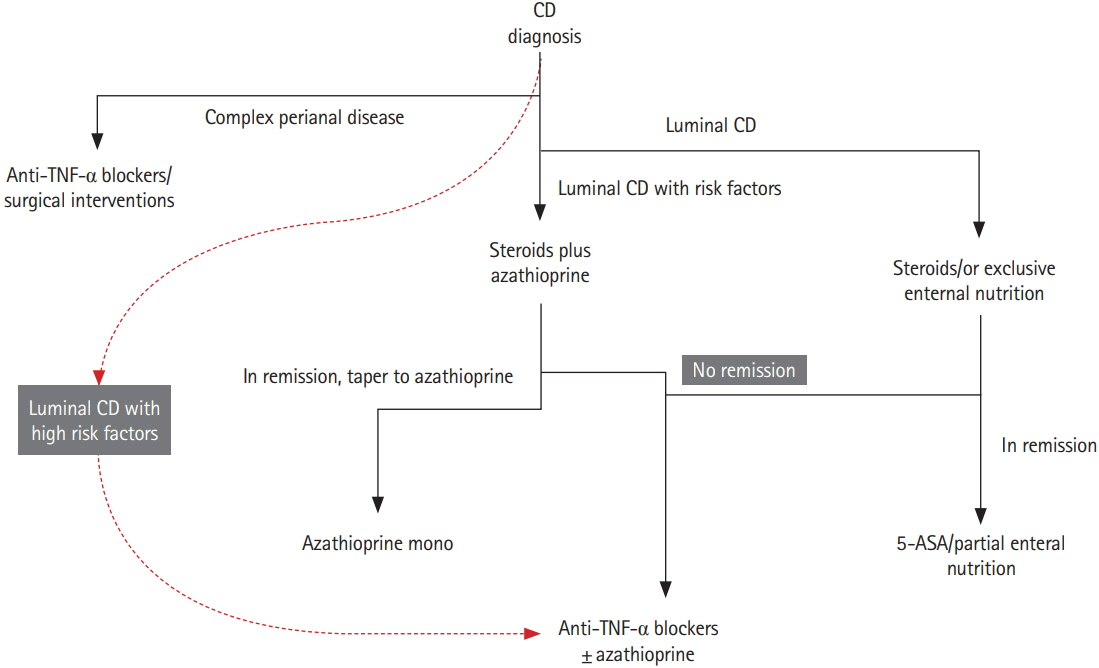
- The incidence of pediatric inflammatory bowel disease (IBD) is increasing worldwide, especially in the developing countries. It differs from adult disease in clinical manifestations, especially with regard to genetic predisposition in monogenic IBD. Pediatric disease also have a tendency to show more aggressive inflammation and greater extent of lesion. Newer drugs such as antitumor necrosis factor-α have been known to make a difference in treating pediatric IBD. Recent studies suggested that the patients with high risk factors might have some benefits from earlier use of biologics. To achieve treatment goals such as relieving symptoms, optimizing growth, and improving quality of life while minimizing drug toxicity, more research is needed to develop tools for risk stratification in the use of biologics for pediatric IBD.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Very early onset inflammatory bowel disease in a South Asian country where inflammatory bowel disease is emerging: a distinct clinical phenotype from later onset disease
Rupa Banerjee, Partha Pal, Zaheer Nabi, Upender Shava, Girish Ganesh, D. Nageshwar Reddy
Intest Res. 2021;19(4):398-407. doi: 10.5217/ir.2020.00107.
Reference
-
1. Kelsen J, Baldassano RN. Inflammatory bowel disease: the difference between children and adults. Inflamm Bowel Dis. 2008; 14 Suppl 2:S9–S11.
Article2. Benchimol EI, Fortinsky KJ, Gozdyra P, Van den Heuvel M, Van Limbergen J, Griffiths AM. Epidemiology of pediatric inflammatory bowel disease: a systematic review of international trends. Inflamm Bowel Dis. 2011; 17:423–439.
Article3. Ng SC, Tang W, Ching JY, et al. Incidence and phenotype of inflammatory bowel disease based on results from the Asia-Pacific Crohn’s and colitis epidemiology study. Gastroenterology. 2013; 145:158–165. e2.
Article4. Ong C, Aw MM, Liwanag MJ, Quak SH, Phua KB. Rapid rise in the incidence and clinical characteristics of pediatric inflammatory bowel disease in a South-East Asian cohort in Singapore, 1994-2015. J Dig Dis. 2018; 19:395–403.
Article5. Hong SJ, Cho SM, Choe BH, et al. Characteristics and incidence trends for pediatric inflammatory bowel disease in Daegu-Kyungpook Province in Korea: a multi-center study. J Korean Med Sci. 2018; 33:e132.
Article6. Van Limbergen J, Russell RK, Drummond HE, et al. Definition of phenotypic characteristics of childhood-onset inflammatory bowel disease. Gastroenterology. 2008; 135:1114–1122.
Article7. Sauer CG, Kugathasan S. Pediatric inflammatory bowel disease: highlighting pediatric differences in IBD. Gastroenterol Clin North Am. 2009; 38:611–628.
Article8. Rinawi F, Assa A, Hartman C, et al. Incidence of bowel surgery and associated risk factors in pediatric-onset Crohn’s disease. Inflamm Bowel Dis. 2016; 22:2917–2923.9. Ruemmele FM, Turner D. Differences in the management of pediatric and adult onset ulcerative colitis: lessons from the joint ECCO and ESPGHAN consensus guidelines for the management of pediatric ulcerative colitis. J Crohns Colitis. 2014; 8:1–4.
Article10. Charpentier C, Salleron J, Savoye G, et al. Natural history of elderly-onset inflammatory bowel disease: a population-based cohort study. Gut. 2014; 63:423–432.11. Jakobsen C, Bartek J Jr, Wewer V, et al. Differences in phenotype and disease course in adult and paediatric inflammatory bowel disease: a population-based study. Aliment Pharmacol Ther. 2011; 34:1217–1224.
Article12. Vernier-Massouille G, Balde M, Salleron J, et al. Natural history of pediatric Crohn’s disease: a population-based cohort study. Gastroenterology. 2008; 135:1106–1113.13. Heyman MB, Kirschner BS, Gold BD, et al. Children with early-onset inflammatory bowel disease (IBD): analysis of a pediatric IBD consortium registry. J Pediatr. 2005; 146:35–40.
Article14. Uhlig HH, Schwerd T, Koletzko S, et al. The diagnostic approach to monogenic very early onset inflammatory bowel disease. Gastroenterology. 2014; 147:990–1007. e3.15. Glocker EO, Kotlarz D, Boztug K, et al. Inflammatory bowel disease and mutations affecting the interleukin-10 receptor. N Engl J Med. 2009; 361:2033–2045.16. Shim JO, Hwang S, Yang HR, et al. Interleukin-10 receptor mutations in children with neonatal-onset Crohn’s disease and intractable ulcerating enterocolitis. Eur J Gastroenterol Hepatol. 2013; 25:1235–1240.
Article17. Shim JO, Seo JK. Very early-onset inflammatory bowel disease (IBD) in infancy is a different disease entity from adultonset IBD; one form of interleukin-10 receptor mutations. J Hum Genet. 2014; 59:337–341.
Article18. Engelhardt KR, Shah N, Faizura-Yeop I, et al. Clinical outcome in IL-10- and IL-10 receptor-deficient patients with or without hematopoietic stem cell transplantation. J Allergy Clin Immunol. 2013; 131:825–830.
Article19. Ko JS. Is infantile inflammatory bowel disease curable with hematopoietic stem cell transplantation? Korean J Gastroenterol. 2013; 62:313–314.
Article20. Snapper SB. Very-early-onset inflammatory bowel disease. Gastroenterol Hepatol (N Y). 2015; 11:554–556.21. Levine A, Griffiths A, Markowitz J, et al. Pediatric modification of the Montreal classification for inflammatory bowel disease: the Paris classification. Inflamm Bowel Dis. 2011; 17:1314–1321.
Article22. Kim KY, Lee EJ, Kim JW, et al. Higher morbidity of monogenic inflammatory bowel disease compared to the adolescent onset inflammatory bowel disease. Pediatr Gastroenterol Hepatol Nutr. 2018; 21:34–42.
Article23. Tsianos EV, Katsanos KH, Tsianos VE. Role of genetics in the diagnosis and prognosis of Crohn’s disease. World J Gastroenterol. 2012; 18:105–118.
Article24. Bianco AM, Girardelli M, Tommasini A. Genetics of inflammatory bowel disease from multifactorial to monogenic forms. World J Gastroenterol. 2015; 21:12296–12310.
Article25. Bouguen G, Levesque BG, Feagan BG, et al. Treat to target: a proposed new paradigm for the management of Crohn’s disease. Clin Gastroenterol Hepatol. 2015; 13:1042–1050. e2.
Article26. Kang B, Choe YH. Early biologic treatment in pediatric Crohn’s disease: catching the therapeutic window of opportunity in early disease by treat-to-target. Pediatr Gastroenterol Hepatol Nutr. 2018; 21:1–11.
Article27. Ruemmele FM, Veres G, Kolho KL, et al. Consensus guidelines of ECCO/ESPGHAN on the medical management of pediatric Crohn’s disease. J Crohns Colitis. 2014; 8:1179–1207.28. Hyams JS, Ferry GD, Mandel FS, et al. Development and validation of a pediatric Crohn’s disease activity Index. J Pediatr Gastroenterol Nutr. 1991; 12:439–447.
Article29. Turner D, Otley AR, Mack D, et al. Development, validation, and evaluation of a Pediatric Ulcerative Colitis Activity Index: a prospective multicenter study. Gastroenterolog. 2007; 133:423–432.
Article30. Danese S, Colombel JF, Reinisch W, Rutgeerts PJ. Review article: infliximab for Crohn’s disease treatment: shifting therapeutic strategies after 10 years of clinical experience. Aliment Pharmacol Ther. 2011; 33:857–869.
Article31. Noh SY, Oh SY, Kim SH, Kim HY, Jung SE, Park KW. Fifteenyear-old colon cancer patient with a 10-year history of ulcerative colitis. World J Gastroenterol. 2013; 19:2437–2440.
Article32. Philpott JR, Kurowski JA. Challenges in transitional care in inflammatory bowel disease: a review of the current literature in transition readiness and outcomes. Inflamm Bowel Dis. 2019; 25:45–55.
Article33. van Rheenen PF, Aloi M, Biron IA, et al. European Crohn’s and Colitis Organisation topical review on transitional care in inflammatory bowel disease. J Crohns Colitis. 2017; 11:1032–1038.
Article34. Brooks AJ, Smith PJ, Cohen R, et al. UK guideline on transition of adolescent and young persons with chronic digestive diseases from paediatric to adult care. Gut. 2017; 66:988–1000.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Pharmacotherapy of Inflammatory Bowel Disease in Child and Adolescence
- Clinical Aspects and Treatments for Pediatric Inflammatory Bowel Diseases
- Pediatric Inflammatory Bowel Disease (IBD): Phenotypic, Genetic and Therapeutic Differences between Early-Onset and Adult-Onset IBD
- Nutritional aspect of pediatric inflammatory bowel disease: its clinical importance
- Inflammatory Bowel Disease in Pediatric Age