J Korean Ophthalmol Soc.
2019 Feb;60(2):160-168. 10.3341/jkos.2019.60.2.160.
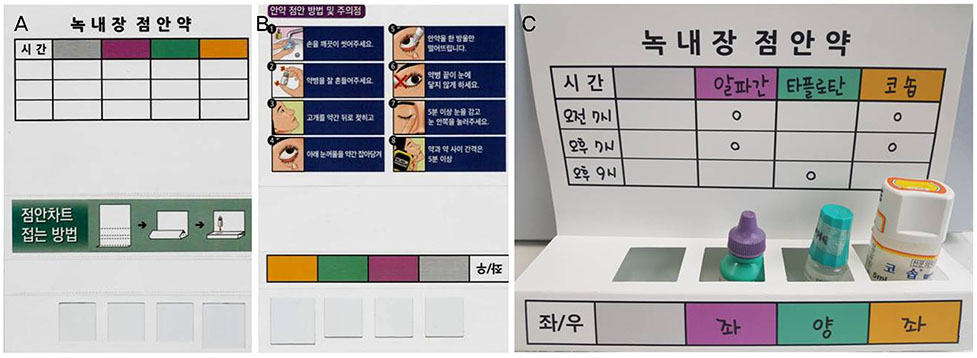
Eye Drop Chart for Improvement of Topical Eye Drops Administration and Adherence
- Affiliations
-
- 1Department of Ophthalmology, Keimyung University School of Medicine, Daegu, Korea. celee@dsmc.or.kr
- 2Cheil Eye Hospital, Daegu, Korea.
- KMID: 2438075
- DOI: http://doi.org/10.3341/jkos.2019.60.2.160
Abstract
- PURPOSE
To evaluate the efficacy of an eye drop chart and to determine the factors contributing to adherence enhancement using the eye drop chart.
METHODS
In this prospective study, enrolled glaucoma patients were educated on the administration of eye drops and use of the eye drop chart. They were required to complete a questionnaire on demographic characteristics and adherence. After 3 months, they completed a second questionnaire on adherence and satisfaction with the use of the eye drop chart. Changes in instillation behavior, relationships between performance scores and demographic characteristics, as well as factors contributing to the improvement of performance scores were analyzed.
RESULTS
Forty-seven patients were enrolled in this study. The performance scores were significantly better for those who administered the eye drops by themselves (p = 0.002), those with an annual income > 60 million won (p = 0.036), and patients with at least a college degree (p = 0.002). After using the eye drop chart for 3 months, the average intraocular pressure was significantly reduced (p = 0.041) and the performance score was improved (p = 0.019). The working area (p = 0.009) and eye drop applicator (p = 0.001) were correlated with performance score enhancement.
CONCLUSIONS
The eye drop chart was a cost-effective tool for improving the adherence and instillation practices of glaucoma patients. Adherence was improved among patients with more indoor activity, and those who practiced self-instillation. It is expected that the respective conditions of such patients would be more efficiently improved in a clinical setting.
Keyword
MeSH Terms
Figure
Reference
-
1. Tatham AJ, Sarodia U, Gatrad F, Awan A. Eye drop instillation technique in patients with glaucoma. Eye (Lond). 2013; 27:1293–1298.
Article2. Gaynes BI, Singa RM, Schaab G, Sorokin Y. Impact of administration angle on the cost of artificial tear solutions: does bottle positioning minimize wastage. J Ocul Pharmacol Ther. 2007; 23:196–201.
Article3. Ritch R, Jamal KN, Gürses-Ozden R, Liebmann JM. An improved technique of eye drop self-administration for patients with limited vision. Am J Ophthalmol. 2003; 135:530–533.
Article4. Kholdebarin R, Campbell RJ, Jin YP, Buys YM. Multicenter study of compliance and drop administration in glaucoma. Can J Ophthalmol. 2008; 43:454–461.
Article5. Taylor SA, Galbraith SM, Mills RP. Causes of non-compliance with drug regimens in glaucoma patients: a qualitative study. J Ocul Pharmacol Ther. 2002; 18:401–409.
Article6. Olthoff CM, Schouten JS, van de, Webers CA. Noncompliance with ocular hypotensive treatment in patients with glaucoma or ocular hypertension an evidence-based review. Ophthalmology. 2005; 112:953–961.7. Krilis M, Coroneo M. Digital eye drop instillation--a novel method. Aust Fam Physician. 2013; 42:201–202.8. Solomon A, Chowers I, Raiskup F, et al. Inadvertent conjunctival trauma related to contact with drug container tips: a masquerade syndrome. Ophthalmology. 2003; 110:796–800.9. Nelson JD. Corneal abrasion resulting from a unit dose artificial tear dispenser. Am J Ophthalmol. 1987; 103(3 Pt 1):333–334.
Article10. Aptel F, Masset H, Burillon C, et al. The influence of disease severity on quality of eye-drop administration in patients with glaucoma or ocular hypertension. Br J Ophthalmol. 2009; 93:700–701.
Article11. Norell SE. Improving medication compliance: a randomised clinical trial. Br Med J. 1979; 2:1031–1033.
Article12. Friedman DS, Hahn SR, Gelb L, et al. Doctor-patient communication, health-related beliefs, and adherence in glaucoma results from the Glaucoma Adherence and Persistency Study. Ophthalmology. 2008; 115:1320–1327.13. Cooper J. Improving compliance with glaucoma eye-drop treatment. Nurs Times. 1996; 92:36–37.14. Ashburn FS Jr, Goldberg I, Kass MA. Compliance with ocular therapy. Surv Ophthalmol. 1980; 24:237–248.
Article15. Newman-Casey PA, Robin AL, Blachley T, et al. The most common barriers to glaucoma medication adherence: a cross-sectional survey. Ophthalmology. 2015; 122:1308–1316.16. Mira JJ, Navarro I, Botella F, et al. A Spanish pillbox app for elderly patients taking multiple medications: randomized controlled trial. J Med Internet Res. 2014; 16:e99.
Article17. Ho LY, Camejo L, Kahook MY, Noecker R. Effect of audible and visual reminders on adherence in glaucoma patients using a commercially available dosing aid. Clin Ophthalmol. 2008; 2:769–772.
Article18. McVeigh KA, Vakros G. The eye drop chart: a pilot study for improving administration of and compliance with topical treatments in glaucoma patients. Clin Ophthalmol. 2015; 9:813–819.19. Feng A, O'Neill J, Holt M, et al. Success of patient training in improving proficiency of eyedrop administration among various ophthalmic patient populations. Clin Ophthalmol. 2016; 10:1505–1511.
Article20. Sleath BL, Krishnadas R, Cho M, et al. Patient-reported barriers to glaucoma medication access, use, and adherence in southern India. Indian J Ophthalmol. 2009; 57:63–68.
Article21. Kaona FA, Tuba M, Siziya S, Sikaona L. An assessment of factors contributing to treatment adherence and knowledge of TB transmission among patients on TB treatment. BMC Public Health. 2004; 4:68.
Article22. Brunner-Ziegler S, Rieder A, Stein KV, et al. Predictors of participation in preventive health examinations in Austria. BMC Public Health. 2013; 13:1138.
Article23. Dunlop S, Coyte PC, McIsaac W. Socio-economic status and the utilisation of physicians’ services: results from the Canadian National Population Health Survey. Soc Sci Med. 2000; 51:123–133.
Article24. Lee SH, Joh HK, Kim S, et al. Income disparities in the use of health screening services among university students in Korea: a cross-sectional study of 2479 participants in a university. Medicine (Baltimore). 2016; 95:e3681.25. Lee YY, Jun JK, Suh M, et al. Barriers to cancer screening among medical aid program recipients in the Republic of Korea: a qualitative study. Asian Pac J Cancer Prev. 2014; 15:589–594.
Article26. Robin A, Grover DS. Compliance and adherence in glaucoma management. Indian J Ophthalmol. 2011; 59:S93–S96.
Article27. Gupta R, Patil B, Shah BM, et al. Evaluating eye drop instillation technique in glaucoma patients. J Glaucoma. 2012; 21:189–192.
Article28. Tsai T, Robin AL, Smith JP 3rd. An evaluation of how glaucoma patients use topical medications: a pilot study. Trans Am Ophthalmol Soc. 2007; 105:29–33.29. Ahn DH, Lee YG, Hong YJ. Factors affecting compliance with prescribed eyedrops for glaucoma. J Korean Ophthalmol Soc. 1998; 39:2145–2151.30. Lee MA, Moon JI, Park MH. Analysis of eye drops applying behavior in glaucoma patients. J Korean Ophthalmol Soc. 2013; 54:1561–1566.
Article31. Shin HY, Kang HT, Lee JW, Lim HJ. The association between socioeconomic status and adherence to health checkup in Korean adults, based on the Korean National Health and Nutrition Examination Survey. Korean J Fam Med. 2018; 39:114–121.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Adherence Improvement in Glaucoma Patients: Effects of Educational Intervention Using an Eye Drop Chart
- Video-recording the Eyedrop Instillation Techniques of Glaucoma Patients
- Analysis of Eye Drops Applying Behavior in Glaucoma Patients
- The Study of Ocular Side Effects after the Use of Anti-Glaucoma Topical Medication
- The Effect of 5% Serum Albumin on Intractable Corneal Epithelial Keratitis: a Case Series and Literature Review