Neonatal Med.
2018 May;25(2):78-84. 10.5385/nm.2018.25.2.78.
Descending Aorta Blood Flow Characteristics before the Development of Necrotizing Enterocolitis in Preterm Neonates
- Affiliations
-
- 1Department of Pediatrics, Seoul St. Mary's Hospital, College of Medicine, the Catholic University of Korea, Seoul, Korea. jaeyounglee@catholic.ac.kr
- KMID: 2437902
- DOI: http://doi.org/10.5385/nm.2018.25.2.78
Abstract
- PURPOSE
To investigate the hemodynamic risk factors for necrotizing enterocolitis (NEC), we analyzed the characteristics of descending aorta (DA) blood flow in preterm neonates, who later developed NEC.
METHODS
This was an observational case-control study on 53 preterm neonates at a tertiary referral center. Clinical and echocardiographic data were collected from 23 preterm neonates with NEC (NEC group), and compared with those of 30 preterm neonates without NEC (control group). Echocardiography was done at a median (interquartile range) of 5 (3-9) days after birth and 2 (1-2.5) days before the diagnosis of NEC.
RESULTS
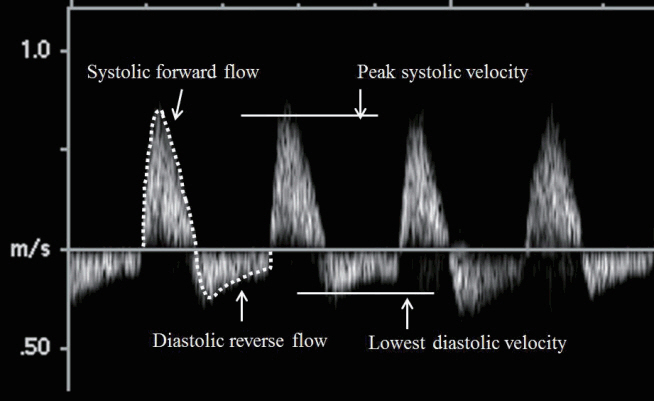
Basic clinical characteristics including gestational age, birth weight, Apgar score, breast feeding status, use of umbilical catheters, and mode of invasive ventilator care were similar between the groups. Compared with the control group, the lowest diastolic velocity of DA was significantly decreased, whereas the diastolic reverse flow and the ratio of diastolic reverse to systolic forward flows were significantly increased in the NEC group. In addition, the resistive index (RI) of DA was significantly increased in the NEC group and showed a positive association with the development of NEC. Multivariate logistic regression analysis showed that increasing RI of DA was an independent risk factor for the development of NEC (P=0.008).
CONCLUSION
Significant changes in DA flow characteristics including decreased diastolic velocity and increased diastolic reverse flow along with increased peripheral vascular resistance were observed before the development of NEC in preterm neonates. These findings may help clinicians stratify in advance neonates at a risk of developing NEC and may help improve outcomes in these neonates.
Keyword
MeSH Terms
-
Aorta, Thoracic*
Apgar Score
Birth Weight
Breast Feeding
Case-Control Studies
Catheters
Critical Care
Diagnosis
Echocardiography
Enterocolitis, Necrotizing*
Gestational Age
Hemodynamics
Humans
Infant, Newborn*
Logistic Models
Parturition
Risk Factors
Splanchnic Circulation
Tertiary Care Centers
Vascular Resistance
Ventilators, Mechanical
Figure
Reference
-
1. Mupsilonller MJ, Paul T, Seeliger S. Necrotizing enterocolitis in premature infants and newborns. J Neonatal Perinatal Med. 2016; 9:233–42.2. Lim JC, Golden JM, Ford HR. Pathogenesis of neonatal necrotizing enterocolitis. Pediatr Surg Int. 2015; 31:509–18.3. Schnabl KL, Van Aerde JE, Thomson AB, Clandinin MT. Necrotizing enterocolitis: a multifactorial disease with no cure. World J Gastroenterol. 2008; 14:2142–61.4. Nowicki PT. Ischemia and necrotizing enterocolitis: where, when, and how. Semin Pediatr Surg. 2005; 14:152–8.5. Chen Y, Chang KT, Lian DW, Lu H, Roy S, Laksmi NK, et al. The role of ischemia in necrotizing enterocolitis. J Pediatr Surg. 2016; 51:1255–61.6. Downard CD, Grant SN, Matheson PJ, Guillaume AW, Debski R, Fallat ME, et al. Altered intestinal microcirculation is the critical event in the development of necrotizing enterocolitis. J Pediatr Surg. 2011; 46:1023–8.7. Gay AN, Lazar DA, Stoll B, Naik-Mathuria B, Mushin OP, Rodriguez MA, et al. Near-infrared spectroscopy measurement of abdominal tissue oxygenation is a useful indicator of intestinal blood flow and necrotizing enterocolitis in premature piglets. J Pediatr Surg. 2011; 46:1034–40.8. Young CM, Kingma SD, Neu J. Ischemia-reperfusion and neonatal intestinal injury. J Pediatr. 2011; 158(2 Suppl):e25–8.9. Zhang HY, Wang F, Feng JX. Intestinal microcirculatory dysfunction and neonatal necrotizing enterocolitis. Chin Med J (Engl). 2013; 126:1771–8.10. Hashem RH, Mansi YA, Almasah NS, Abdelghaffar S. Doppler ultrasound assessment of the splanchnic circulation in preterms with neonatal sepsis at risk for necrotizing enterocolitis. J Ultrasound. 2017; 20:59–67.11. Murdoch EM, Sinha AK, Shanmugalingam ST, Smith GC, Kempley ST. Doppler flow velocimetry in the superior mesenteric artery on the first day of life in preterm infants and the risk of neonatal necrotizing enterocolitis. Pediatrics. 2006; 118:1999–2003.12. Urboniene A, Palepsaitis A, Uktveris R, Barauskas V. Doppler flowmetry of the superior mesenteric artery and portal vein: impact for the early prediction of necrotizing enterocolitis in neonates. Pediatr Surg Int. 2015; 31:1061–6.13. Fang S, Kempley ST, Gamsu HR. Prediction of early tolerance to enteral feeding in preterm infants by measurement of superior mesenteric artery blood flow velocity. Arch Dis Child Fetal Neonatal Ed. 2001; 85:F42–5.14. Miller TA, Minich LL, Lambert LM, Joss-Moore L, Puchalski MD. Abnormal abdominal aorta hemodynamics are associated with necrotizing enterocolitis in infants with hypoplastic left heart syndrome. Pediatr Cardiol. 2014; 35:616–21.15. Carlo WF, Kimball TR, Michelfelder EC, Border WL. Persistent diastolic flow reversal in abdominal aortic Doppler-flow profiles is associated with an increased risk of necrotizing enterocolitis in term infants with congenital heart disease. Pediatrics. 2007; 119:330–5.16. Walsh MC, Kliegman RM. Necrotizing enterocolitis: treatment based on staging criteria. Pediatr Clin North Am. 1986; 33:179–201.17. Yoon JH, Lee EJ, Yum SK, Moon CJ, Youn YA, Kwun YJ, et al. Impacts of therapeutic hypothermia on cardiovascular hemodynamics in newborns with hypoxic-ischemic encephalopathy: a case control study using echocardiography. J Matern Fetal Neonatal Med. 2017; Jul. 7. [Epub]. https://doi.org/10.1080/14767058.2017.1338256.18. Hochwald O, Jabr M, Osiovich H, Miller SP, McNamara PJ, Lavoie PM. Preferential cephalic redistribution of left ventricular cardiac output during therapeutic hypothermia for perinatal hypoxic-ischemic encephalopathy. J Pediatr. 2014; 164:999–1004. e1.19. Kessler U, Schulte F, Cholewa D, Nelle M, Schaefer SC, Klimek PM, et al. Outcome in neonates with necrotizing enterocolitis and patent ductus arteriosus. World J Pediatr. 2016; 12:55–9.20. Groves AM, Kuschel CA, Knight DB, Skinner JR. Does retrograde diastolic flow in the descending aorta signify impaired systemic perfusion in preterm infants? Pediatr Res. 2008; 63:89–94.21. Bude RO, Rubin JM. Relationship between the resistive index and vascular compliance and resistance. Radiology. 1999; 211:411–7.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Serious Necrotizing Enterocolitis in a Neonate Treated with Octreotide for Congenital Chylothorax
- The relation between serum levels of epidermal growth factor and necrotizing enterocolitis in preterm neonates
- Necrotizing Enterocolitis Associated with Norovirus Infection in a Preterm Infant
- Two Cases of Hemorrhagic Necrotizing Enterocolitis as a Presenting Complaint of Hirschsprung's Disease
- Double Intussusceptions with Necrotizing Enterocolitis Diagnosed in a Premature Infant