Neonatal Med.
2018 Nov;25(4):170-177. 10.5385/nm.2018.25.4.170.
Comparison of Hemoglobin Correction Effects According to Storage Period and Other Factors in the Transfusion of Packed Red Blood Cells in Neonatal Intensive Care Unit Patients
- Affiliations
-
- 1Department of Pediatrics, Kosin University College of Medicine, Busan, Korea. pondhong@gmail.com
- KMID: 2436135
- DOI: http://doi.org/10.5385/nm.2018.25.4.170
Abstract
- PURPOSE
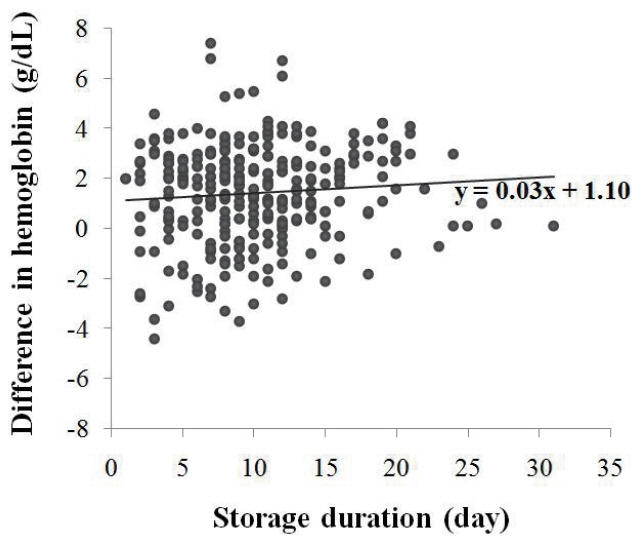
Preterm infants frequently require red blood cell (RBC) transfusions in neonatal intensive care units (NICU). Storage RBCs undergo many changes during storage periods. We aimed to compare the hemoglobin (Hb) correction effect according to the period of RBC storage and investigate the factors influencing Hb correction.
METHODS
This retrospective study reviewed the medical records of 289 patients who received RBC transfusion more than once in the NICU of Kosin University Gospel Hospital between February 2006 and March 2016. The subjects were classified into two storage groups: short-term (≤7 days, n=88) and long-term (>7 days, n=201), according to the period of RBC storage. We checked Hb levels by complete blood cell count tests conducted within 2 days before and 5 to 9 days after the first transfusion. We compared the Hb difference between the two groups and analyzed the factors influencing Hb correction.
RESULTS
Excluding the use of an invasive ventilator, there was no significant difference between the two groups in terms of clinical characteristics. There was no significant difference in the Hb correction effect between the two groups (P=0.537). Birth weight greater than 1,500 g, higher weight at transfusion, and larger volume of transfusion were significant prognostic factors affecting greater changes in Hb. In addition, surgery experience, higher Hb level at transfusion, and additional blood tests were found to be significantly associated with less changes in Hb.
CONCLUSION
The RBC storage period did not affect the Hb correction effect. The Hb correction effect may be diminished in infants with lower birth weight and lower weight at transfusion under unstable clinical conditions.
MeSH Terms
Figure
Reference
-
1. Quinn K, Quinn M, Moreno C, Soundar E, Teruya J, Hui SK. Neonatal transfusion models to determine the impact of using fresh red blood cells on inventory and exposure. Blood Transfus. 2015; 13:595–9.2. Lee SH, Yoon J, Park Y, Lee SK, Kim HC, Shim WS. The use of quadruple blood bags transfusion of low birth weight neonates. J Korean Pediatr Soc. 1999; 42:1122–9.3. Bell EF, Strauss RG, Widness JA, Mahoney LT, Mock DM, Seward VJ, et al. Randomized trial of liberal versus restrictive guidelines for red blood cell transfusion in preterm infants. Pediatrics. 2005; 115:1685–91.4. Kim HM. Advances in neonatal care and outcome of low birth weight infants. J Korean Pediatr Soc. 1996; 39:762–72.5. Kim SS. Optimal hemoglobin level in preterm infants. Neonatal Med. 2014; 21:92–8.6. Fernandes da Cunha DH, Nunes Dos Santos AM, Kopelman BI, Areco KN, Guinsburg R, de Araujo Peres C, et al. Transfusions of CPDA-1 red blood cells stored for up to 28 days decrease donor exposures in very low-birth-weight premature infants. Transfus Med. 2005; 15:467–73.7. Kasat K, Hendricks-Munoz KD, Mally PV. Neonatal red blood cell transfusions: searching for better guidelines. Blood Transfus. 2011; 9:86–94.8. Whyte RK, Jefferies AL; Canadian Paediatric Society, Fetus and Newborn Committee. Red blood cell transfusion in newborn infants. Paediatr Child Health. 2014; 19:213–22.9. Tinmouth A, Fergusson D, Yee IC, Hebert PC; ABLE Investigators; Canadian Critical Care Trials Group. Clinical consequences of red cell storage in the critically ill. Transfusion. 2006; 46:2014–27.10. Hogman CF, Meryman HT. Storage parameters affecting red blood cell survival and function after transfusion. Transfus Med Rev. 1999; 13:275–96.11. Hess JR. Red cell storage. J Proteomics. 2010; 73:368–73.12. Lion N, Crettaz D, Rubin O, Tissot JD. Stored red blood cells: a changing universe waiting for its map(s). J Proteomics. 2010; 73:374–85.13. Mangel J, Goldman M, Garcia C, Spurll G. Reduction of donor exposures in premature infants by the use of designated adenine-saline preserved split red blood cell packs. J Perinatol. 2001; 21:363–7.14. Fergusson DA, Hebert P, Hogan DL, LeBel L, Rouvinez-Bouali N, Smyth JA, et al. Effect of fresh red blood cell transfusions on clinical outcomes in premature, very low-birth-weight infants: the ARIPI randomized trial. JAMA. 2012; 308:1443–51.15. Lee DA, Slagle TA, Jackson TM, Evans CS. Reducing blood donor exposures in low birth weight infants by the use of older, unwashed packed red blood cells. J Pediatr. 1995; 126:280–6.16. BISS. Blood Information Sharing System [Internet]. Wonju: KOREAN Redcross Blood Services;2018. [cited 2018 Nov 21]. Available from: http://biss.bloodinfo.net.17. The Korean Society of Neonatology. Indications of transfusion in manual of neonatal care. 3rd ed. Seoul: The Korean Society of Neonatology;2014.18. Nortfolk D. Neonatal transfusion. In : Nortfolk D, editor. Handbook for transfusion medicine. 5th ed. Norwich: Joint United Kingdom (UK) Blood Transfusion and Tissue Transplantation Services Professional Advisory Committee;2013. [cited 2018 Nov 21]. Available from: https://www.transfusionguidelines.org/transfusion-handbook/10-effective-transfusion-in-paediatric-practice/10-2-neonatal-transfusion.19. Shanmugha Priya RA, Krishnamoorthy R, Panicker VK, Ninan B. Transfusion support in preterm neonates <1500 g and/or <32 weeks in a tertiary care center: a descriptive study. Asian J Transfus Sci. 2018; 12:34–41.20. Fasano RM, Luban N. Blood component therapy for the neonate. In : Martin RJ, Fanaroff AA, Walsh MC, editors. Fanaroff and Martin’s neonatal-perinatal medicine. 10th ed. Cleveland: Elsevier;2015. p. 1344–61.21. New York State Department of Health. Guidelines for transfusion therapy of infants from birth to four months of age. 2nd ed. New York: New York State Council on Human Blood and Transfusion services;2004.22. Said Conti V, Azzopardi E, Parascandalo R, Soler P, Attard Montalto S. Overview of the blood transfusion policy in preterms on the neonatal intensive care unit. Malta Med J. 2013; 25:46–50.23. Jeon GW, Sin JB. Risk factors of transfusion in anemia of very low birth weight infants. Yonsei Med J. 2013; 54:366–73.24. Alan S, Arsan S. Prevention of the anaemia of prematurity. Int J Pediatr Adolesc Med. 2015; 2:99–106.25. Freitas BA, Franceschini Sdo C. Factors associated with packed red blood cell transfusions in premature infants in an intensive care unit. Rev Bras Ter Intensiva. 2012; 24:224–9.26. Liu EA, Mannino FL, Lane TA. Prospective, randomized trial of the safety and efficacy of a limited donor exposure transfusion program for premature neonates. J Pediatr. 1994; 125:92–6.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Factors Affecting the Freshness of Transfused Packed Red Blood Cells
- Transfusion-Related Acute Lung Injury after Stored Packed Red Blood Cell Transfusion: A Case Report
- Adequate Change Interval of Transfusion Kits during Rapid Transfusion
- The Change of White Blood Cell Count Following Transfusion in Preterm Neonates
- Packed Red Cell Transfusion in Neonate: Effects of Age of Red Cells on Serum Laboratory Values and Readjustment of Hematocrit Values after Transfusion