Yeungnam Univ J Med.
2019 Jan;36(1):43-49. 10.12701/yujm.2019.00094.
Comparison of the removal torque and a histomorphometric evaluation of the RBM treated implants with the RBM followed by laser treated implants: an experimental study in rabbits
- Affiliations
-
- 1Department of Dentistry, Yeungnam University College of Medicine, Daegu, Korea.
- 2Department of Dentistry, Kyungpook National University Medical Center, Daegu, Korea.
- 3Department of Dental Hygiene, College of Science & Technology, Kyungpook National University, Sangju, Korea. jinha01@naver.com
- KMID: 2434098
- DOI: http://doi.org/10.12701/yujm.2019.00094
Abstract
- BACKGROUND
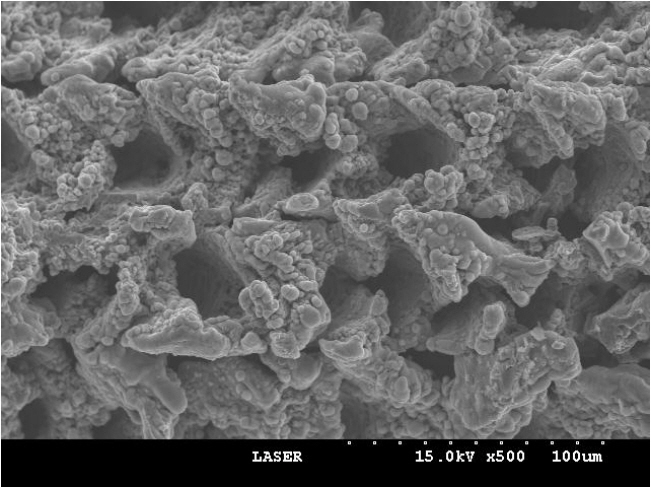
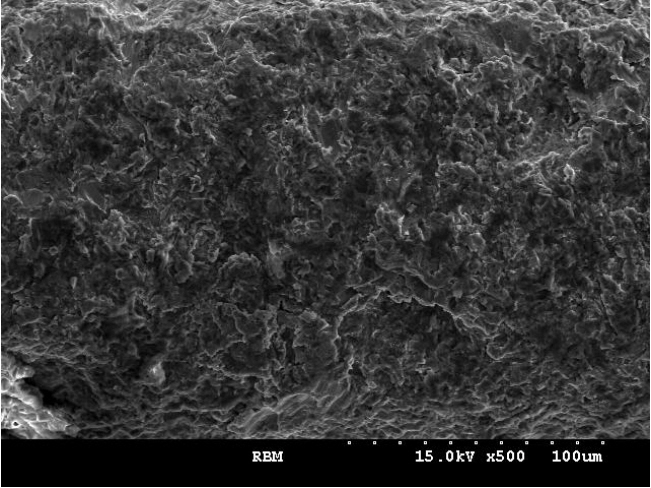
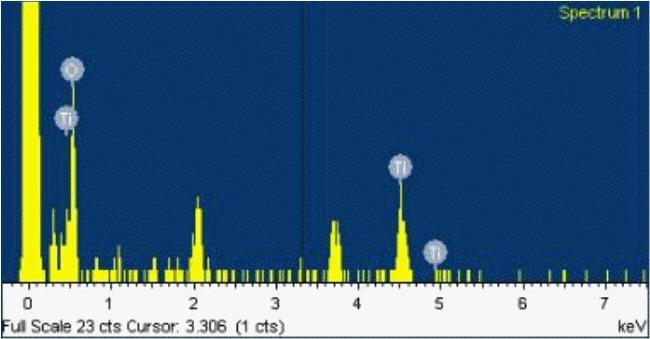
In the osseointegration of dental implants, the implant surface properties have been reported to be some of the most important critical factors. The effect of implant's surfaces created by resorbable blast media (RBM) followed by laser ablation on bone tissue reactions was examined using the removal torque test and histomorphometric analysis.
METHODS
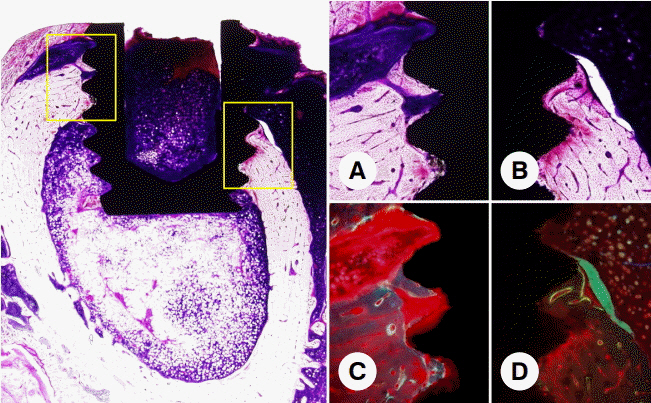
Two types of dental implants, RBM-laser implants (experimental group) and RBM implants (control group) (CSM implant system, Daegu, Korea; L=6 mm, diameter=3.75 mm) were placed into the right and left distal femoral metaphysis of 17 adult rabbits. Six weeks after placement, removal torque was measured and histomorphometric analysis was performed.
RESULTS
The mean removal torque was 24.0±10.2 Ncm and 46.6±16.4 Ncm for the control and test specimens, respectively. The experimental RBM-laser implants had significantly higher removal torque values than the control RBM implants (p=0.013). The mean values of total and cortical bone to implant contact (BIC) were respectively 46.3±10.8% and 65.3±12.5% for the experimental group, and 41.9±18.5% and 57.6±10.6% for the control group. The experimental RBM-laser implants showed a higher degree of total and cortical BIC compared with RBM implants, but there was no statistical significance (p=0.482, 0.225).
CONCLUSION
The removal torque and BIC of the test group were higher than those of the control group. In this study, the surface treatment created by RBM treatment followed by laser ablation appears to have a potential in improving bone tissue reactions of dental implants.
MeSH Terms
Figure
Reference
-
References
1. Levine RA, Clem DS 3rd, Wilson TG Jr, Higginbottom F, Solnit G. Multicenter retrospective analysis of the ITI implant system used for single-tooth replacements: results of loading for 2 or more years. Int J Oral Maxillofac Implants. 1999; 14:516–20.2. Park YJ, Cho SA. Retrospective chart analysis on survival rate of fixtures installed at the tuberosity bone for cases with missing unilateral upper molars: a study of 7 cases. J Oral Maxillofac Surg. 2010; 68:1338–44.
Article3. Lekholm U, van Steenberghe D, Herrmann I, Bolender C, Folmer T, Gunne J, et al. Osseointegrated implants in the treatment of partially edentulous jaws: a prospective 5-year multicenter study. Int J Oral Maxillofac Implants. 1994; 9:627–35.4. Adell R, Eriksson B, Lekholm U, Brånemark PI, Jemt T. Long-term follow-up study of osseointegrated implants in the treatment of totally edentulous jaws. Int J Oral Maxillofac Implants. 1990; 5:347–59.5. Albrektsson T, Brånemark PI, Hansson HA, Lindström J. Osseointegrated titanium implants. Requirements for ensuring a long-lasting, direct bone-to-implant anchorage in man. Acta Orthop Scand. 1981; 52:155–70.6. Wennerberg A, Albrektsson T, Lausmaa J. Torque and histomorphometric evaluation of c.p. titanium screws blasted with 25- and 75-microns-sized particles of Al2O3. J Biomed Mater Res. 1996; 30:251–60.7. Gonshor A, Goveia G, Sotirakis E. A prospective, multicenter, 4-year study of the ACE Surgical resorbable blast media implant. J Oral Implantol. 2003; 29:174–80.
Article8. Piattelli M, Scarano A, Paolantonio M, Iezzi G, Petrone G, Piattelli A. Bone response to machined and resorbable blast material titanium implants: an experimental study in rabbits. J Oral Implantol. 2002; 28:2–8.
Article9. Yoo IS, Yim SB, Chung CH, Hong KS. A compare research of machined implant and RBM surface implant. J Korean Acad Periodontol. 2008; 38:467–74.
Article10. Gaggl A, Schultes G, Müller WD, Kärcher H. Scanning electron microscopical analysis of laser-treated titanium implant surfaces--a comparative study. Biomaterials. 2000; 21:1067–73.
Article11. Johansson C, Albrektsson T. Integration of screw implants in the rabbit: a 1-year follow-up of removal torque of titanium implants. Int J Oral Maxillofac Implants. 1987; 2:69–75.12. Cho SA, Park KT. The removal torque of titanium screw inserted in rabbit tibia treated by dual acid etching. Biomaterials. 2003; 24:3611–7.
Article13. Kim KS, Suh KW, Leesungbok R, Ryu JJ. Removal torque of bicortically stabilized RBM (resorbable blast media) pin implants in rabbit tibia. J Korean Acad Prosthodont. 2006; 44:722–33.14. Han CH, Johansson CB, Wennerberg A, Albrektsson T. Quantitative and qualitative investigations of surface enlarged titanium and titanium alloy implants. Clin Oral Implants Res. 1998; 9:1–10.
Article15. Faeda RS, Tavares HS, Sartori R, Guastaldi AC, Marcantonio E Jr. Biological performance of chemical hydroxyapatite coating associated with implant surface modification by laser beam: biomechanical study in rabbit tibias. J Oral Maxillofac Surg. 2009; 67:1706–15.
Article16. Wennerberg A, Albrektsson T, Andersson B, Krol JJ. A histomorphometric and removal torque study of screw-shaped titanium implants with three different surface topographies. Clin Oral Implants Res. 1995; 6:24–30.
Article17. Rønold HJ, Lyngstadaas SP, Ellingsen JE. Analysing the optimal value for titanium implant roughness in bone attachment using a tensile test. Biomaterials. 2003; 24:4559–64.
Article18. Rong M, Zhou L, Gou Z, Zhu A, Zhou D. The early osseointegration of the laser-treated and acid-etched dental implants surface: an experimental study in rabbits. J Mater Sci Mater Med. 2009; 20:1721–8.
Article19. Sul YT, Johansson C, Wennerberg A, Cho LR, Chang BS, Albrektsson T. Optimum surface properties of oxidized implants for reinforcement of osseointegration: surface chemistry, oxide thickness, porosity, roughness, and crystal structure. Int J Oral Maxillofac Implants. 2005; 20:349–59.20. Albrektsson T, Wennerberg A. Oral implant surfaces: part 1--review focusing on topographic and chemical properties of different surfaces and in vivo responses to them. Int J Prosthodont. 2004; 17:536–43.21. Albrektsson T, Wennerberg A. Oral implant surfaces: part 2--review focusing on clinical knowledge of different surfaces. Int J Prosthodont. 2004; 17:544–64.22. Wennerberg A, Hallgren C, Johansson C, Danelli S. A histomorphometric evaluation of screw-shaped implants each prepared with two surface roughnesses. Clin Oral Implants Res. 1998; 9:11–9.
Article23. Jartoft P, Krantz M. Kinoform guided laser microfabrication of titanium implant surfaces [dissertation]. Göteborg: Chalmers University of Technology;1997.24. Guo Z, Zhou L, Rong M, Zhu A, Geng H. Bone response to a pure titanium implant surface modified by laser etching and microarc oxidation. Int J Oral Maxillofac Implants. 2010; 25:130–6.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of removal torque of saline-soaking RBM implants and RBM implants in rabbit tibias
- On the effect of saline immersion to the removal torque for resorbable blasting media and acid treated implants
- Histologic evaluation and removal torque analysis of nano- and microtreated titanium implants in the dogs
- The effect of different surface treatment on the osseointegration and stability of implants
- Removal torque of bicortically stabilized RBM(resorbable blast media) pin implants in rabbit tibia