Ann Rehabil Med.
2018 Oct;42(5):652-659. 10.5535/arm.2018.42.5.652.
Comparison Between Neuromuscular Electrical Stimulation to Abdominal and Back Muscles on Postural Balance in Post-stroke Hemiplegic Patients
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Soonchunhyang University Bucheon Hospital, Soonchunhyang University College of Medicine, Bucheon, Korea. shouletz@gmail.com
- KMID: 2429194
- DOI: http://doi.org/10.5535/arm.2018.42.5.652
Abstract
OBJECTIVE
To compare the effects of neuromuscular electrical stimulation (NMES) to abdominal muscles and back muscles on postural balance in post-stroke hemiplegic patients.
METHODS
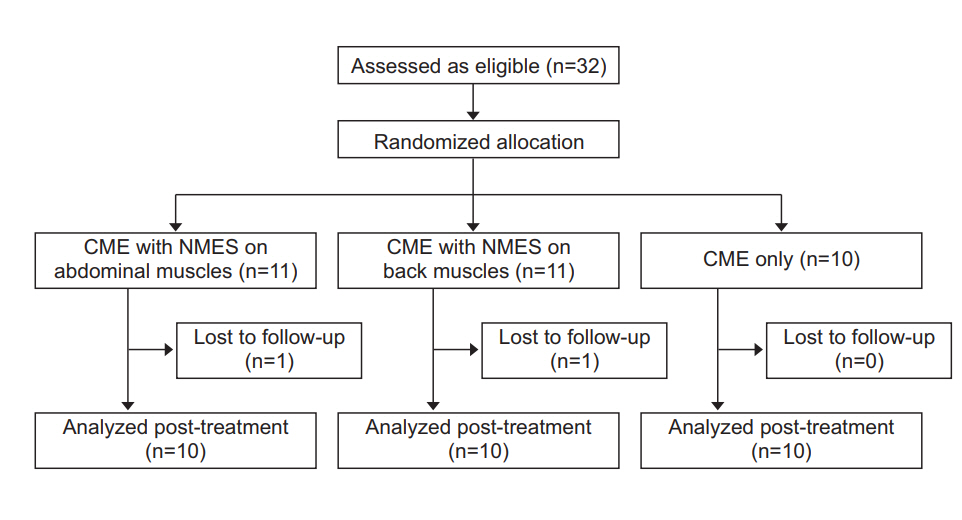
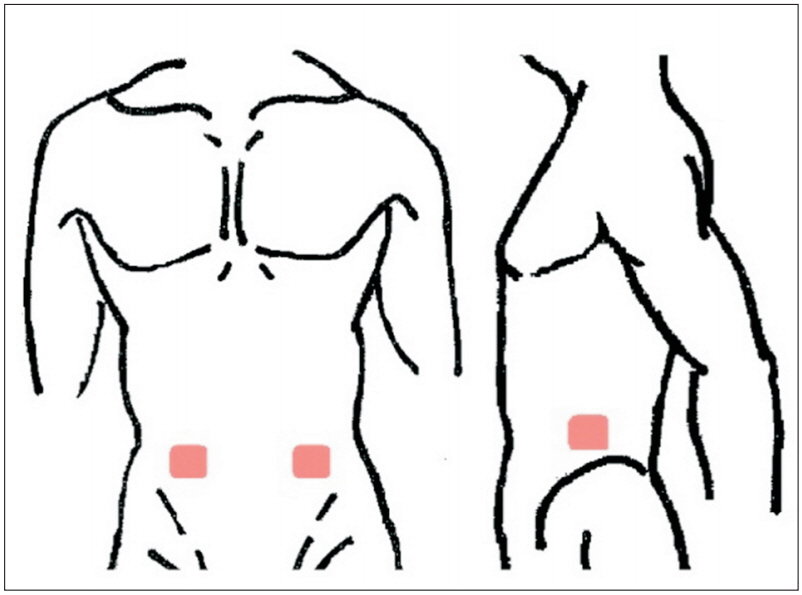
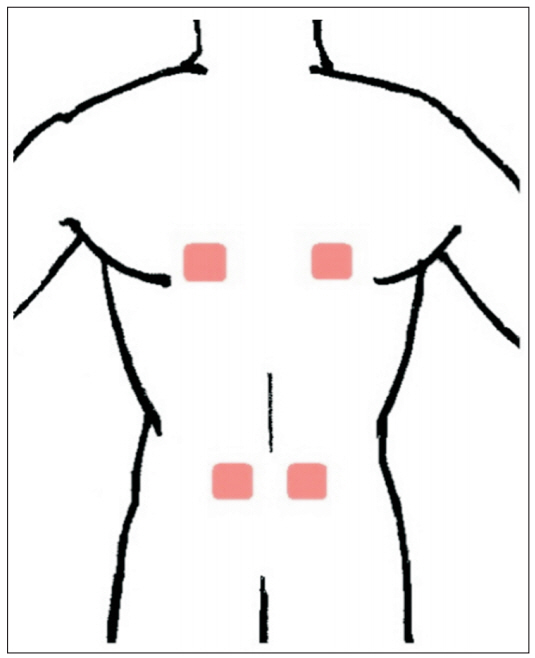
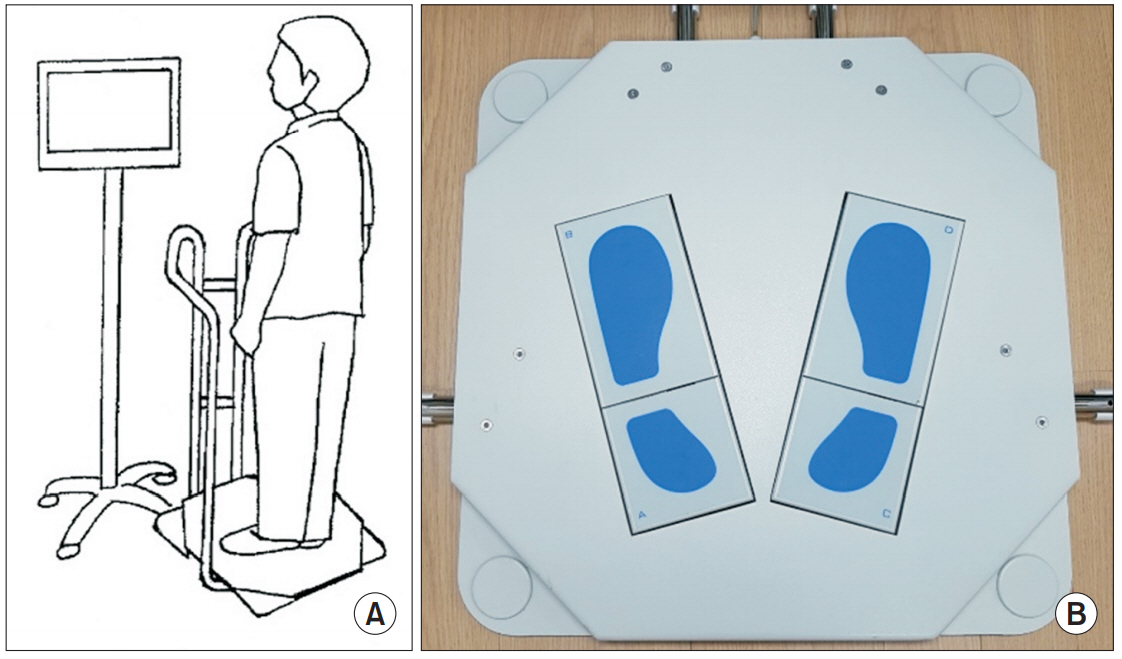
Thirty post-stroke hemiplegic patients were prospectively enrolled and randomly assigned to one of the three groups: core muscle-strengthening exercise (CME) with NMES to abdominal muscles (group A), CME with NMES to back muscles (group B), and CME alone (group C). All subjects underwent their targeted interventions for 30 minutes each day, 5 days per week for 3 weeks under a conventional stroke rehabilitation program. Subjects were evaluated using Korean version of Berg Balance Scale (K-BBS), Trunk Impairment Scale (TIS), Korean version of Modified Barthel Index (K-MBI), Weight Distribution Index (WDI), and Stability Index (SI) just before and 3 weeks after intervention.
RESULTS
Changes in K-BBS (p < 0.05) and TIS (p < 0.05) were significantly higher in group A (18.5±8.10, 6.6±1.90) and group B (19.9±5.44, 7.0±2.26) than in group C (8.4±4.14, 3.1±0.99). However, K-MBI, WDI, and SI failed to show any significant difference. No significant difference in all outcomes was observed between groups A and B.
CONCLUSION
The effect of NMES to the abdominal muscles was similar to the effect on back muscles in terms of postural balance. This finding indicated that the NMES to the abdominal muscles may be an alternative for post-stroke hemiplegic patients contraindicated for NMES to the back muscles. Additional studies investigating the effects of NMES on abdominal and back muscles are needed.
MeSH Terms
Figure
Reference
-
1. Kibler WB, Press J, Sciascia A. The role of core stability in athletic function. Sports Med. 2006; 36:189–98.
Article2. Chuter VH, Janse de Jonge XA. Proximal and distal contributions to lower extremity injury: a review of the literature. Gait Posture. 2012; 36:7–15.
Article3. Hodges PW. Core stability exercise in chronic low back pain. Orthop Clin North Am. 2003; 34:245–54.
Article4. Karatas M, Cetin N, Bayramoglu M, Dilek A. Trunk muscle strength in relation to balance and functional disability in unihemispheric stroke patients. Am J Phys Med Rehabil. 2004; 83:81–7.
Article5. Merkert J, Butz S, Nieczaj R, Steinhagen-Thiessen E, Eckardt R. Combined whole body vibration and balance training using Vibrosphere: improvement of trunk stability, muscle tone, and postural control in stroke patients during early geriatric rehabilitation. Z Gerontol Geriatr. 2011; 44:256–61.6. Ko EJ, Chun MH, Kim DY, Yi JH, Kim W, Hong J. The additive effects of core muscle strengthening and trunk NMES on trunk balance in stroke patients. Ann Rehabil Med. 2016; 40:142–51.
Article7. Yoo SD, Jeong YS, Kim DH, Lee M, Noh SG, Shin YW, et al. The efficacy of core strengthening on the trunk balance in patients with subacute stroke. J Korean Acad Rehabil Med. 2010; 34:677–82.8. Yu SH, Park SD. The effects of core stability strength exercise on muscle activity and trunk impairment scale in stroke patients. J Exerc Rehabil. 2013; 9:362–7.
Article9. Fujita T, Sato A, Togashi Y, Kasahara R, Ohashi T, Yamamoto Y. Contribution of abdominal muscle strength to various activities of daily living of stroke patients with mild paralysis. J Phys Ther Sci. 2015; 27:815–8.
Article10. Kim YM, Chun MH, Kang SH, Ahn WH. The effect of neuromuscular electrical stimulation on trunk control in hemiparetic stroke patients. J Korean Acad Rehabil Med. 2009; 33:265–70.11. Baek SO, Cho HK, Jung GS, Son SM, Cho YW, Ahn SH. Verification of an optimized stimulation point on the abdominal wall for transcutaneous neuromuscular electrical stimulation for activation of deep lumbar stabilizing muscles. Spine J. 2014; 14:2178–83.
Article12. Smith MC, Byblow WD, Barber PA, Stinear CM. Proportional recovery from lower limb motor impairment after stroke. Stroke. 2017; 48:1400–3.
Article13. Stinear CM, Byblow WD, Ackerley SJ, Barber PA, Smith MC. Predicting recovery potential for individual stroke patients increases rehabilitation efficiency. Stroke. 2017; 48:1011–9.
Article14. Cortes JC, Goldsmith J, Harran MD, Xu J, Kim N, Schambra HM, et al. A short and distinct time window for recovery of arm motor control early after stroke revealed with a global measure of trajectory kinematics. Neurorehabil Neural Repair. 2017; 31:552–60.
Article15. Bohannon RW. Lateral trunk flexion strength: impairment, measurement reliability and implications following unilateral brain lesion. Int J Rehabil Res. 1992; 15:249–51.16. Tanaka S, Hachisuka K, Ogata H. Muscle strength of trunk flexion-extension in post-stroke hemiplegic patients. Am J Phys Med Rehabil. 1998; 77:288–90.17. Vieira S, Dibai-Filho AV, Brandino HE, Ferreira VT, Scheicher ME. Abdominal muscle strength is related to the quality of life among older adults with lumbar osteoarthritis. J Bodyw Mov Ther. 2015; 19:273–7.
Article18. Gibson JN, Smith K, Rennie MJ. Prevention of disuse muscle atrophy by means of electrical stimulation: maintenance of protein synthesis. Lancet. 1988; 2:767–70.
Article19. Maffiuletti NA, Roig M, Karatzanos E, Nanas S. Neuromuscular electrical stimulation for preventing skeletal-muscle weakness and wasting in critically ill patients: a systematic review. BMC Med. 2013; 11:137.
Article20. Qi YC, Niu XL, Gao YR, Wang HB, Hu M, Dong LP, et al. Therapeutic effect evaluation of neuromuscular electrical stimulation with or without strengthening exercise on spastic cerebral palsy. Clin Pediatr (Phila). 2018; 57:580–3.
Article21. Alon G, McCombe SA, Koutsantonis S, Stumphauzer LJ, Burgwin KC, Parent MM, et al. Comparison of the effects of electrical stimulation and exercise on abdominal musculature. J Orthop Sports Phys Ther. 1987; 8:567–73.
Article22. Frontera WR, DeLisa JA. DeLisa’s physical medicine and rehabilitation. 5th ed. Philadelphia: Lippincott Williams and Wilkins;2010. p. 1393–409.23. Kang JI, Kim BR, Park SK, Yang DJ, Jeong DK, Kim JH. Effects of deep abdominal muscle strengthening exercises on pulmonary function and the ability to balance in stroke patients. J Korea Phys Ther. 2015; 27:258–63.
Article24. Coghlan S, Crowe L, McCarthypersson U, Minogue C, Caulfield B. Neuromuscular electrical stimulation training results in enhanced activation of spinal stabilizing muscles during spinal loading and improvements in pain ratings. Conf Proc IEEE Eng Med Biol Soc. 2011; 2011:7622–5.
Article25. Akkaya N, Doganlar N, Celik E, Aysse SE, Akkaya S, Gungor HR, et al. Test-retest reliability of Tetrax static posturography system in young adults with low physical activity level. Int J Sports Phys Ther. 2015; 10:893–900.26. Quatman-Yates CC, Lee A, Hugentobler JA, Kurowski BG, Myer GD, Riley MA. Test-retest consistency of a postural sway assessment protocol for adolescent athletes measured with a force plate. Int J Sports Phys Ther. 2013; 8:741–8.27. Kohen-Raz R. Application of tetra-ataxiametric posturography in clinical and developmental diagnosis. Percept Mot Skills. 1991; 73:635–56.
Article28. Klavora P, Warren M. Rehabilitation of visuomotor skills in poststroke patients using the Dynavision apparatus. Percept Mot Skills. 1998; 86:23–30.
Article29. Lee NH, Lee J, Lee KN. The effects of treatment with a TETRAX on balance and mobility in acute stroke patients. Phys Ther Korea. 2010; 17:11–9.30. Ma J, Yao YJ, Ma RM, Li JQ, Wang T, Li XJ, et al. Effects of sleep deprivation on human postural control, subjective fatigue assessment and psychomotor performance. J Int Med Res. 2009; 37:1311–20.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Electrical Stimulation on Spasticity in Hemiplegic Patients
- The Effect of an Abdominal Drawing-In Maneuver Combined with Low·High Frequency Neuromuscular Electrical Stimulation on Trunk Muscle Activity, Muscle Fatigue, and Balance in Stroke Patients
- Effect of Transcranial Direct Current Stimulation on Postural Stability and Lower Extremity Strength in Hemiplegic Stroke Patients
- The Effect of Neuromuscular Electrical Stimulation on Trunk Control in Hemiparetic Stroke Patients
- The Effects of Balance Training Using Balance System in the Hemiplegic Patients