J Korean Acad Nurs.
2018 Jun;48(3):266-278. 10.4040/jkan.2018.48.3.266.
Self-Management Experiences of the Adolescents with Chronic Kidney Disease
- Affiliations
-
- 1Hanil University & Presbyterian Theological Seminary, Wanju, Korea.
- 2College of Nursing, Dankook University, Cheonan, Korea. sw724@dankook.ac.kr
- KMID: 2429103
- DOI: http://doi.org/10.4040/jkan.2018.48.3.266
Abstract
- PURPOSE
The aim of this study was to develop a substantive theory on self-management conducted by the adolescents with chronic kidney disease from their lived experience.
METHODS
Data was collected through in-depth interviews from May to December in 2015 with thirteen adolescents with chronic kidney disease. The data collected were analyzed on the basis of Strauss and Corbin's grounded theory.
RESULTS
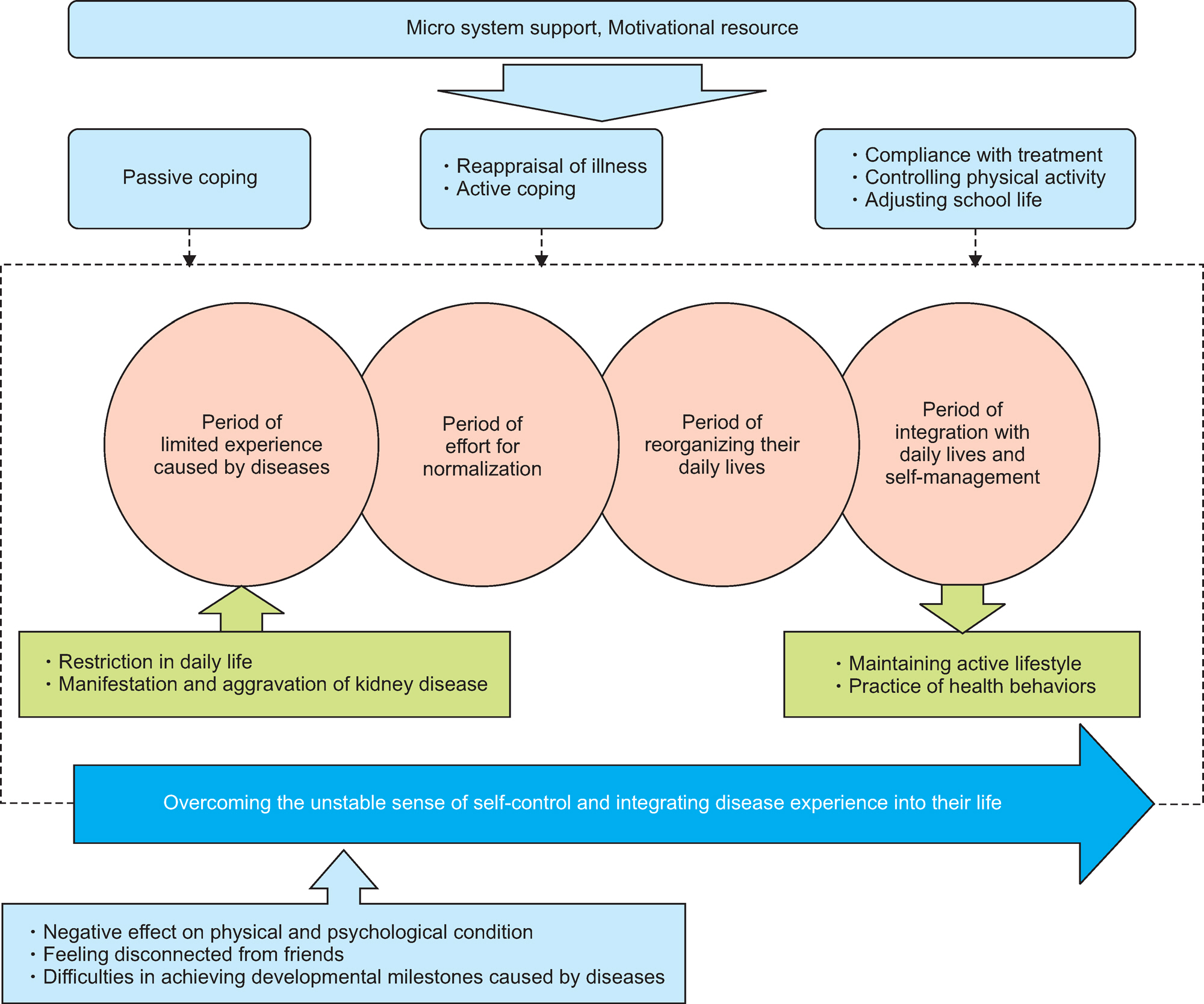
The core of the category found in this study was "overcoming the unstable sense of self-control and integrating disease experience into their life". The causal conditions triggering the central phenomenon were "restriction in daily life" and "manifestation and aggravation of symptom". The central phenomenon in the experience of self-management within the adolescents with chronic kidney disease was "unstable sense of self control". The intervening condition for unstable self control were "micro system support" and "motivational resources". This study found that the adolescents with chronic kidney disease followed a series of strategies when they faced the central phenomenon, including; passive coping, reappraisal of illness, active coping, compliance with treatment, controlling physical activity, and adjusting school life. With these strategic approaches, the adolescents with chronic kidney disease could maintain their active lifestyles and achieve their health behaviors. The process of self-management by these adolescents passed through four phases; limited experience caused by diseases, effort for normalization, reorganizing their daily lives, and integration with daily lives and self-management.
CONCLUSION
This Study explored the process and experience of self-management of adolescents with chronic kidney disease. These findings can be used for basis for developing substantive theory and nursing intervention strategy for adolescents with chronic kidney diseases.
Keyword
MeSH Terms
Figure
Reference
-
References
1. National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: Evaluation, classification, and stratification. American Journal of Kidney Diseases. 2002; 39(2 Suppl l):S1–S266.2. Kang HK, Lee JY, Shin JI, Cheo MH, Park SK, Oh GH, et al. Current status of Korean children and adolescents with chronic kidney disease patients by type: Survival and renal function retention 10 years follow-up study pediatric cohort. The 32nd Annual Spring Meeting of the Korean Society of Nephrology. 2012; 2012(1):75.3. Shin YM, Cho SM. Emotional and behavioral problems in children with chronic physical illness. Annals of Pediatric Endocrinology & Metabolism. 2012; 17(1):1–9. https://doi.org/10.6065/apem.2012.17.1.1.
Article4. Lim MH, Park YS. A study of happiness among Korean adolescents: With specific focusing on elementary and middle school students. Journal of Education & Culture. 2006; 12:159–179.5. Ferro MA. Adolescents and young adults with physical illness: A comparative study of psychological distress. Acta Paediatri-ca. 2014; 103(1):e32–e37. https://doi.org/10.1111/apa.12429.
Article6. Kelly MM. Children and adolescents with chronic kidney disease: A population at risk for more than just kidney disease. Nephrology Nursing Journal. 2016; 43(1):67–70. quiz 71.7. Tong A, Wong G, McTaggart S, Henning P, Mackie F, Carroll RP, et al. Quality of life of young adults and adolescents with chronic kidney disease. The Journal of Pediatrics. 2013; 163(4):1179–1185.e5. https://doi.org/10.1016/j.jpeds.2013.04.066.
Article8. Korean Academy of Nursing. The great encyclopedia of nursing science. Seoul: Korean Dictionary Research Publishing;1996. p. 176.9. Park YS, Jeong EN, Yang JH. Lived experiences of life world for adolescents with epilepsy. Journal of Korean Academy of Fundamentals Nursing. 2011; 18(1):6–18.10. Kim SM. A narrative inquiry exploring disease experience of adolescent renal transplant recipients [dissertation]. Seoul: Seoul National University;2016. p. 1–195.11. Graves MM, Roberts MC, Rapoff M, Boyer A. The efficacy of adherence interventions of chronically ill children: A meta-analytic review. Journal of Pediatric Psychology. 2010; 35(4):368–382. https://doi.org/10.1093/jpepsy/jsp072.12. Kirk S, Beatty S, Callery P, Gellatly J, Milnes L, Pryjmachuk S. The effectiveness of self-care support interventions for children and young people with long-term conditions: A systematic review. Child: Care, Health and Development. 2013; 39(3):305–324. https://doi.org/10.1111/j.1365-2214.2012.01395.x.
Article13. Kim DH, Im YJ. Validity and reliability of Korean version of the family management measure (Korean FaMM) for families with children having chronic illness. Journal of Korean Academy of Nursing. 2013; 43(1):123–132. https://doi.org/10.4040/jkan.2013.43.1.123.
Article14. Lee BR, Park HJ, Lee KY. Korean adolescents’ physical health and peer relationships: The mediating effects of self-perceived health status and resilience. Korean Journal of Child Studies. 2013; 34(5):127–144. https://doi.org/10.5723/KJCS.2013.34.5.127.15. Jung SY. A study on psychosocial factors associated with self-care in adolescents with type 1 diabetes mellitus [master’s thesis]. Seoul: Hanyang University;2008. p. 1–58.16. Yoo H, Kim HS. Development and evaluation of the Empowering A Self-Efficacy (EASE) program for children with epilepsy. Journal of Korean Academy of Nursing. 2015; 45(1):54–63. https://doi.org/10.4040/jkan.2015.45.1.54.
Article17. Kim SS, Kwon IS. Knowledge and practice in self-management on asthma of school-aged children with asthma. Child Health Nursing Research. 2016; 22(2):87–96. https://doi.org/10.4094/chnr.2016.22.2.87.
Article18. Eiser C. Psychological effects of chronic disease. Journal of Child Psychology and Psychiatry. 1990; 31(1):85–98. https://doi.org/10.1111/j.1469-7610.1990.tb02274.x.
Article19. Corbin J, Strauss AL. Basics of qualitative research: Techniques and procedures for developing grounded theory. 3rd ed. Thousand Oaks (CA): Sage;2008. p. 1–130.20. Guba EG, Lincoln YS. Effective evaluation. San Francisco (CA): Jossey-Bass Publishers;1981. p. 104.21. Kul M, Cengel Kültür E, Senses Dinç G, Bilginer Y, Uluç S, Baykan H. Quality of life in children and adolescents with chronic kidney disease: A comparative study between different disease stages and treatment modalities. The Turkish Journal of Pediatrics. 2013; 55(5):493–499.22. Shin MS, Cho SC, Jang JY, Cheong HI, Choi Y, Ha IS. Development of a quality of life scale for children on chronic peri- toneal dialysis. Childhood Kidney Diseases. 2008; 12(2):202–212. https://doi.org/10.3339/jkspn.2008.12.2.202.23. Sattoe JNT, Jedeloo S, van Staa A. Effective peer-to-peer support for young people with end-stage renal disease: A mixed methods evaluation of Camp COOL. BMC Nephrology. 2013; 14:279. https://doi.org/10.1186/1471-2369-14-279.
Article24. Taylor RM, Gibson F, Franck LS. The experience of living with a chronic illness during adolescence: A critical review of the literature. Journal of Clinical Nursing. 2008; 17(23):3083–3091. https://doi.org/10.1111/j.1365-2702.2008.02629.x.
Article25. Eklund PG, Sivberg B. Adolescents’ lived experience of epilepsy. Journal of Neuroscience Nursing. 2003; 35(1):40–49.
Article26. Shin EJ. Development of educational program for management of mental health and improvement of quality of life in children and adolescents with chronic illness and their parent. Seoul: Yonsei University;2015. Nov. Report No.: 2015-05.27. Tjaden LA, Vogelzang J, Jager KJ, van Stralen KJ, Maurice-Stam H, Grootenhuis MA. Long-term quality of life and social outcome of childhood end-stage renal disease. The Journal of Pediatrics. 2014; 165(2):336–342.e1. https://doi.org/10.1016/j.jpeds.2014.04.013.
Article28. Kim HO, Jeon MS, Kim MJ. Relationship between self-efficacy, social support and health promoting behavior in high school students. Journal of the Korean Society of Maternal and Child Health. 2015; 19(1):11–22.29. McGue M, Iacono WG, Krueger R. The association of early adolescent problem behavior and adult psychopathology: A multivariate behavioral genetic perspective. Behavior Genetics. 2006; 36(4):591–602. https://doi.org/10.1007/s10519-006-9061-z.
Article30. Burkhart PV, Rayens MK. Self-concept and health locus of control: Factors related to children’s adherence to recommended asthma regimen. Pediatric Nursing. 2005; 31(5):404–409.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Slowing the Progression of Chronic Kidney Disease in Children and Adolescents
- Peritoneal dialysis in children and adolescents
- Concept Analysis of Self-management in Children with Chronic Kidney Diseases through Walker and Avant’s Method
- Osteoporosis in Patients with Chronic Kidney Disease
- The gut-kidney connection in advanced chronic kidney disease