High-Carbohydrate Diets and Food Patterns and Their Associations with Metabolic Disease in the Korean Population
- Affiliations
-
- 1Major of Food Science and Nutrition, School of Human Ecology, The Catholic University of Korea, Bucheon, Korea. yjsong@catholic.ac.kr
- 2Department of Food and Nutrition, Hannam University, Daejeon, Korea.
- KMID: 2428909
- DOI: http://doi.org/10.3349/ymj.2018.59.7.834
Abstract
- PURPOSE
Although an Asian diet is typically high in carbohydrate and low in fat, there has been a steady increase in the rate of cardiometabolic disease in Asian countries over the past decade. We evaluated food patterns of a high-carbohydrate diet and examined their associations with metabolic disease.
MATERIALS AND METHODS
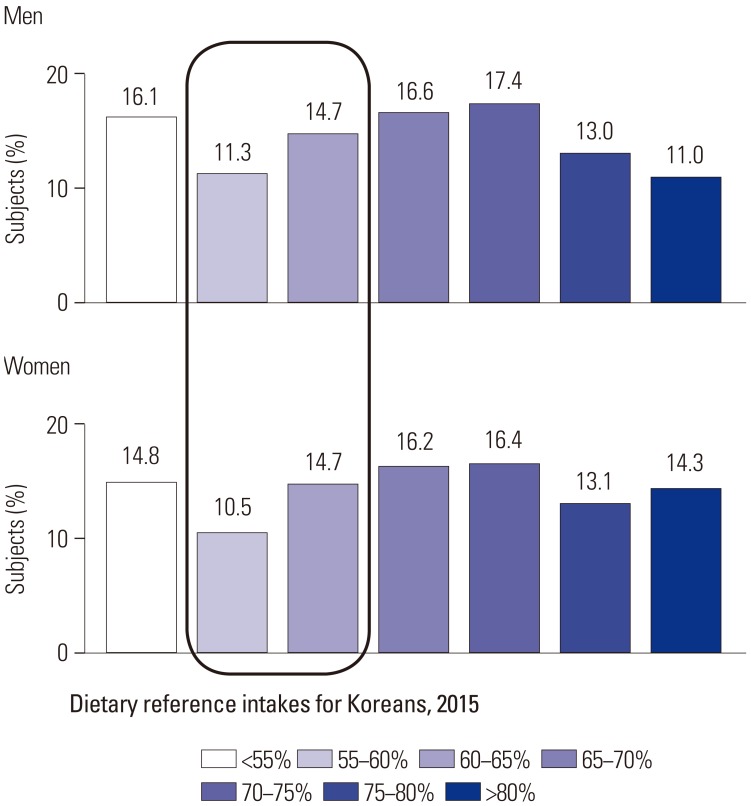
Using data from the 2013-2015 Korean National Health and Nutrition Examination Survey, we included a total of 13106 subjects aged 20 years or older in this study. Diet was divided into seven groups according to the percentage of energy from carbohydrates. Food patterns were evaluated as individual servings per food group. Multivariate logistic regression was conducted to estimate odds ratios (OR) for metabolic disease.
RESULTS
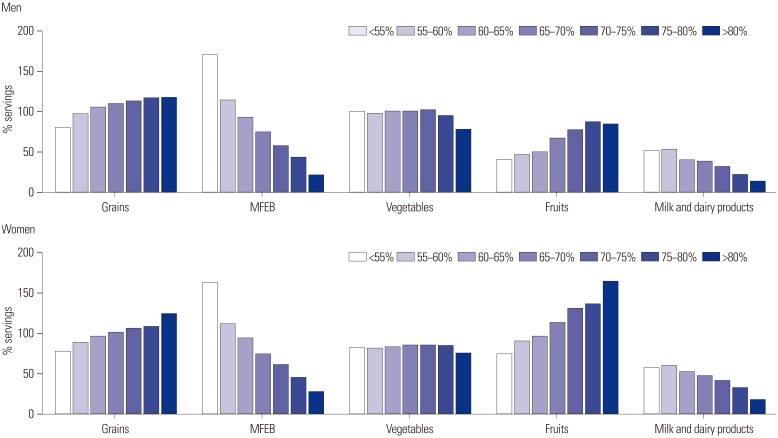
The proportions of men and women exceeding the recommended range of carbohydrate intake were 58.0% and 60.0%, respectively. A higher carbohydrate diet was associated with intake of low energy and saturated fats, with more grains and fruit, but less meat, fish, egg, bean (MFEB), and dairy consumption. Carbohydrate intake decreased by 3.0-3.4% per serving of MFEB and milk. In men, the highest carbohydrate group showed an OR of 1.35 [95% confidence interval (CI), 0.91 to 1.99] for metabolic syndrome, although this failed to show statistical significance. In women, the highest carbohydrate group had an OR of 1.38 (95% CI, 1.06 to 1.80) for a reduced level of high-density lipoprotein cholesterol.
CONCLUSION
This study suggests that a very-high-carbohydrate diet for the Korean population is attributable to lower consumption of MFEB and dairy products and is associated with several metabolic risk factors. The appropriate distribution of macronutrients for the prevention and management of metabolic disease should be explored.
Keyword
MeSH Terms
Figure
Cited by 7 articles
-
Diabetes Fact Sheets in Korea, 2020: An Appraisal of Current Status
Chan-Hee Jung, Jang Won Son, Shinae Kang, Won Jun Kim, Hun-Sung Kim, Hae Soon Kim, Mihae Seo, Hye-Jung Shin, Seong-Su Lee, Su Jin Jeong, Yongin Cho, Seung Jin Han, Hyang Mi Jang, Mira Rho, Shinbi Lee, Mihyun Koo, Been Yoo, Jung-Wha Moon, Hye Young Lee, Jae-Seung Yun, Sun Young Kim, Sung Rae Kim, In-Kyung Jeong, Ji-Oh Mok, Kun Ho Yoon
Diabetes Metab J. 2021;45(1):1-10. doi: 10.4093/dmj.2020.0254.Leisure Time Physical Activity to Reduce Metabolic Syndrome Risk: A 10-Year Community-Based Prospective Study in Korea
Hoon Jo, Jang-Young Kim, Min-Ye Jung, Yeon-Soon Ahn, Sei-Jin Chang, Sang-Baek Koh
Yonsei Med J. 2020;61(3):218-228. doi: 10.3349/ymj.2020.61.3.218.Blood Sugar Control and Low-Carbohydrate High-Fat Diet
Eun Hee Kang
J Korean Diabetes. 2018;19(4):237-245. doi: 10.4093/jkd.2018.19.4.237.Associations of Dietary Intake with Cardiovascular Disease, Blood Pressure, and Lipid Profile in the Korean Population: a Systematic Review and Meta-Analysis
Jeongseon Kim, Tung Hoang, So Young Bu, Ji-Myung Kim, Jeong-Hwa Choi, Eunju Park, Seung-Min Lee, Eunmi Park, Ji Yeon Min, In Seok Lee, So Young Youn
J Lipid Atheroscler. 2020;9(1):205-229. doi: 10.12997/jla.2020.9.1.205.Estimated glycemic load (eGL) of mixed meals and its associations with cardiometabolic risk factors among Korean adults: data from the 2013 ~ 2016 Korea National Health and Nutrition Examination Survey
Kyungho Ha, Kisun Nam, YoonJu Song
J Nutr Health. 2019;52(4):354-368. doi: 10.4163/jnh.2019.52.4.354.Regional disparities related to cardiovascular diseases and diet quality in Korean adults: based on the 2013–2016 Korea National Health and Nutrition Examination Survey Data
Bo Young Seo, Eun Sil Her
Nutr Res Pract. 2022;16(6):755-764. doi: 10.4162/nrp.2022.16.6.755.Health-related quality of life and nutrient intake of the elderly with type 2 diabetes according to comorbidity burden: a cross-sectional study
Yejung Choi, Kyong Park
Korean J Community Nutr. 2024;29(5):418-430. doi: 10.5720/kjcn.2024.00014.
Reference
-
1. Accurso A, Bernstein RK, Dahlqvist A, Draznin B, Feinman RD, Fine EJ, et al. Dietary carbohydrate restriction in type 2 diabetes mellitus and metabolic syndrome: time for a critical appraisal. Nutr Metab (Lond). 2008; 5:9. PMID: 18397522.
Article2. Park YW, Zhu S, Palaniappan L, Heshka S, Carnethon MR, Heymsfield SB. The metabolic syndrome: prevalence and associated risk factor findings in the US population from the Third National Health and Nutrition Examination Survey, 1988–1994. Arch Intern Med. 2003; 163:427–436. PMID: 12588201.3. Song S, Lee JE, Song WO, Paik HY, Song Y. Carbohydrate intake and refined-grain consumption are associated with metabolic syndrome in the Korean adult population. J Acad Nutr Diet. 2014; 114:54–62. PMID: 24200655.
Article4. Villegas R, Liu S, Gao YT, Yang G, Li H, Zheng W, et al. Prospective study of dietary carbohydrates, glycemic index, glycemic load, and incidence of type 2 diabetes mellitus in middle-aged Chinese women. Arch Intern Med. 2007; 167:2310–2316. PMID: 18039989.
Article5. Yu D, Shu XO, Li H, Xiang YB, Yang G, Gao YT, et al. Dietary carbohydrates, refined grains, glycemic load, and risk of coronary heart disease in Chinese adults. Am J Epidemiol. 2013; 178:1542–1549. PMID: 24008907.
Article6. Radhika G, Van Dam RM, Sudha V, Ganesan A, Mohan V. Refined grain consumption and the metabolic syndrome in urban Asian Indians (Chennai Urban Rural Epidemiology Study 57). Metabolism. 2009; 58:675–681. PMID: 19375591.
Article7. Sahyoun NR, Jacques PF, Zhang XL, Juan W, McKeown NM. Whole-grain intake is inversely associated with the metabolic syndrome and mortality in older adults. Am J Clin Nutr. 2006; 83:124–131. PMID: 16400060.
Article8. McKeown NM, Meigs JB, Liu S, Saltzman E, Wilson PW, Jacques PF. Carbohydrate nutrition, insulin resistance, and the prevalence of the metabolic syndrome in the Framingham Offspring Cohort. Diabetes Care. 2004; 27:538–546. PMID: 14747241.
Article9. Esmaillzadeh A, Mirmiran P, Azizi F. Whole-grain consumption and the metabolic syndrome: a favorable association in Tehranian adults. Eur J Clin Nutr. 2005; 59:353–362. PMID: 15536473.
Article10. Mellen PB, Walsh TF, Herrington DM. Whole grain intake and cardiovascular disease: a meta-analysis. Nutr Metab Cardiovasc Dis. 2008; 18:283–290. PMID: 17449231.
Article11. Ye EQ, Chacko SA, Chou EL, Kugizaki M, Liu S. Greater whole-grain intake is associated with lower risk of type 2 diabetes, cardiovascular disease, and weight gain. J Nutr. 2012; 142:1304–1313. PMID: 22649266.
Article12. Greenwood DC, Threapleton DE, Evans CE, Cleghorn CL, Nykjaer C, Woodhead C, et al. Glycemic index, glycemic load, carbohydrates, and type 2 diabetes: systematic review and dose-response meta-analysis of prospective studies. Diabetes Care. 2013; 36:4166–4171. PMID: 24265366.13. Dong JY, Zhang YH, Wang P, Qin LQ. Meta-analysis of dietary glycemic load and glycemic index in relation to risk of coronary heart disease. Am J Cardiol. 2012; 109:1608–1613. PMID: 22440121.
Article14. Barclay AW, Petocz P, McMillan-Price J, Flood VM, Prvan T, Mitchell P, et al. Glycemic index, glycemic load, and chronic disease risk--a meta-analysis of observational studies. Am J Clin Nutr. 2008; 87:627–637. PMID: 18326601.
Article15. Ford ES, Dietz WH. Trends in energy intake among adults in the United States: findings from NHANES. Am J Clin Nutr. 2013; 97:848–853. PMID: 23426032.16. Yun S, Kim HJ, Oh K. Trends in energy intake among Korean adults, 1998–2015: results from the Korea National Health and Nutrition Examination Survey. Nutr Res Pract. 2017; 11:147–154. PMID: 28386388.
Article17. Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, et al. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES). Int J Epidemiol. 2014; 43:69–77. PMID: 24585853.
Article18. Korean Ministry of Health and Welfare. Dietary reference intakes for Koreans 2015. Sejong: Korean Ministry of Health and Welfare;2015.19. Korea Centers for Disease Control and Prevention. Manual for the fifth Korea National Health and Nutrition Examination Survey: health examination. Osong: Korea Centers for Disease Control and Prevention;2012.20. Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005; 112:2735–2752. PMID: 16157765.21. Lee SY, Park HS, Kim DJ, Han JH, Kim SM, Cho GJ, et al. Appropriate waist circumference cutoff points for central obesity in Korean adults. Diabetes Res Clin Pract. 2007; 75:72–80. PMID: 16735075.
Article22. Bosomworth NJ. Approach to identifying and managing atherogenic dyslipidemia: a metabolic consequence of obesity and diabetes. Can Fam Physician. 2013; 59:1169–1180. PMID: 24235189.23. Lee S. Association of whole grain consumption with socio-demographic and eating behavior factors in a Korean population: based on 2007–2008 Korea National Health and Nutrition Examination Survey. Korean J Community Nutr. 2011; 16:353–363.
Article24. Lichtenstein AH, Van Horn L. Very low fat diets. Circulation. 1998; 98:935–939. PMID: 9738652.
Article25. Schaefer EJ, Lichtenstein AH, Lamon-Fava S, McNamara JR, Schaefer MM, Rasmussen H, et al. Body weight and low-density lipoprotein cholesterol changes after consumption of a low-fat ad libitum diet. JAMA. 1995; 274:1450–1455. PMID: 7474191.
Article26. Lichtenstein AH, Ausman LM, Carrasco W, Jenner JL, Ordovas JM, Schaefer EJ. Short-term consumption of a low-fat diet beneficially affects plasma lipid concentrations only when accompanied by weight loss. Hypercholesterolemia, low-fat diet, and plasma lipids. Arterioscler Thromb. 1994; 14:1751–1760. PMID: 7947600.
Article27. Clevidence BA, Judd JT, Schatzkin A, Muesing RA, Campbell WS, Brown CC, et al. Plasma lipid and lipoprotein concentrations of men consuming a low-fat, high-fiber diet. Am J Clin Nutr. 1992; 55:689–694. PMID: 1312762.
Article28. Schwingshackl L, Hoffmann G. Comparison of long-term low-fat versus high-fat diets on blood lipids: a systematic review and meta-analysis. Proc Nutr Soc. 2012; 71:E220.
Article29. Feng R, Du S, Chen Y, Zheng S, Zhang W, Na G, et al. High carbohydrate intake from starchy foods is positively associated with metabolic disorders: a Cohort Study from a Chinese population. Sci Rep. 2015; 5:16919. PMID: 26581652.
Article30. Murakami K, Sasaki S, Takahashi Y, Okubo H, Hosoi Y, Horiguchi H, et al. Dietary glycemic index and load in relation to metabolic risk factors in Japanese female farmers with traditional dietary habits. Am J Clin Nutr. 2006; 83:1161–1169. PMID: 16685061.
Article31. Park S, Ahn J, Lee BK. Very-low-fat diets may be associated with increased risk of metabolic syndrome in the adult population. Clin Nutr. 2016; 35:1159–1167. PMID: 26602244.
Article32. Zhang XM, Zhang YB, Chi MH. Soy protein supplementation reduces clinical indices in type 2 diabetes and metabolic syndrome. Yonsei Med J. 2016; 57:681–689. PMID: 26996569.
Article33. Lee JE, McLerran DF, Rolland B, Chen Y, Grant EJ, Vedanthan R, et al. Meat intake and cause-specific mortality: a pooled analysis of Asian prospective cohort studies. Am J Clin Nutr. 2013; 98:1032–1041. PMID: 23902788.
Article34. Pan A, Sun Q, Bernstein AM, Schulze MB, Manson JE, Stampfer MJ, et al. Red meat consumption and mortality: results from 2 prospective cohort studies. Arch Intern Med. 2012; 172:555–563. PMID: 22412075.35. Larsson SC, Orsini N. Red meat and processed meat consumption and all-cause mortality: a meta-analysis. Am J Epidemiol. 2014; 179:282–289. PMID: 24148709.
Article36. Sauvaget C, Nagano J, Allen N, Grant EJ, Beral V. Intake of animal products and stroke mortality in the Hiroshima/Nagasaki Life Span Study. Int J Epidemiol. 2003; 32:536–543. PMID: 12913025.
Article37. Sauvaget C, Nagano J, Hayashi M, Yamada M. Animal protein, animal fat, and cholesterol intakes and risk of cerebral infarction mortality in the adult health study. Stroke. 2004; 35:1531–1537. PMID: 15166397.
Article38. Mizoue T, Yamaji T, Tabata S, Yamaguchi K, Ogawa S, Mineshita M, et al. Dietary patterns and glucose tolerance abnormalities in Japanese men. J Nutr. 2006; 136:1352–1358. PMID: 16614429.
Article39. Takata Y, Shu XO, Gao YT, Li H, Zhang X, Gao J, et al. Red meat and poultry intakes and risk of total and cause-specific mortality: results from cohort studies of Chinese adults in Shanghai. PLoS One. 2013; 8:e56963. PMID: 23451121.
Article40. Lee SA, Shu XO, Yang G, Li H, Gao YT, Zheng W. Animal origin foods and colorectal cancer risk: a report from the Shanghai Women's Health Study. Nutr Cancer. 2009; 61:194–205. PMID: 19235035.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Low-Carbohydrate Diets in Korea: Why Does It Matter, and What Is Next?
- Diet as a treatment for chronic kidney disease
- Effectiveness and safety of low-carbohydrate diets
- Association between Dietary Carbohydrate Intake and Cardiovascular Risk Factors According to Low-Density Lipoprotein Cholesterol Levels in Korean Adults
- Effects of a Low-carbohydrate, High-fat Diet