Allergy Asthma Immunol Res.
2019 Jan;11(1):79-89. 10.4168/aair.2019.11.1.79.
Association Between Epithelial Cytokines and Clinical Phenotypes of Elderly Asthma
- Affiliations
-
- 1Department of Allergy and Clinical Immunology, Ajou University School of Medicine, Suwon, Korea. hspark@ajou.ac.kr
- KMID: 2426787
- DOI: http://doi.org/10.4168/aair.2019.11.1.79
Abstract
- PURPOSE
Asthma in the elderly has different clinical features including more severe phenotypes with higher comorbidities. Epithelial cells are known to initiate innate/adaptive immune responses in asthmatic airways. We investigated clinical features and epithelial derived cytokine levels in elderly asthmatics compared to non-elderly asthmatics in a cross-sectional cohort of adult asthmatics in order to further understand its pathogenic mechanisms.
METHODS
A total of 1,452 adult asthmatics were enrolled from a single tertiary hospital and were classified into 2 groups: 234 elderly (≥ 60 years at initial diagnosis) and 1,218 non-elderly (< 60 years at initial diagnosis) asthmatics. Asthma-related clinical parameters were compared between the 2 groups. Serum levels of epithelial cell-derived cytokines including interleukin (IL)-31, IL-33, IL-8, eotaxin-2, transforming growth factor beta 1 (TGF-β1) and periostin were measured by enzyme-linked immunosorbent assay.
RESULTS
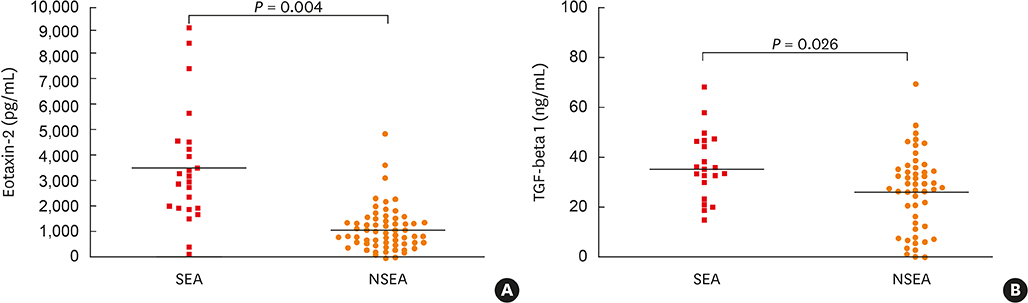
Significantly higher prevalence rates of late-onset asthma (onset age ≥ 40 years) and severe asthma, as well as the lower rate of atopy, blood/sputum eosinophil counts, total immunoglobulin E and eosinophil cationic protein levels were noted in elderly asthmatics compared to non-elderly asthmatics (P < 0.05, respectively). The forced expiratory volume in 1 second (FEV1, % predicted) level tended to be lower in elderly asthmatics (P = 0.07). In addition, serum IL-33 and IL-31 levels were significantly lower in elderly asthmatics, while no differences were found in the serum level of IL-8, eotaxin-2, TGF-β1 or periostin. Among elderly asthmatics, subjects with severe asthma had lower FEV1 (% predicted) value, but showed significantly higher serum levels of eotaxin-2 and TGF-β1, than those with non-severe asthma (P < 0.05 for each).
CONCLUSIONS
These findings suggest that age-related changes of epithelial cell-derived cytokines may affect clinical phenotypes and severity of elderly asthma: decreased levels of IL-33 and IL-31 may contribute to less Th2 phenotype, while increased levels of eotaxin-2 and TGF-β1 may contribute to severity.
Keyword
MeSH Terms
-
Adult
Aged*
Asthma*
Chemokine CCL24
Cohort Studies
Comorbidity
Cytokines*
Enzyme-Linked Immunosorbent Assay
Eosinophil Cationic Protein
Eosinophils
Epithelial Cells
Forced Expiratory Volume
Humans
Immunoglobulin E
Immunoglobulins
Interleukin-33
Interleukin-8
Interleukins
Phenotype*
Prevalence
Tertiary Care Centers
Transforming Growth Factor beta
Chemokine CCL24
Cytokines
Eosinophil Cationic Protein
Immunoglobulin E
Immunoglobulins
Interleukin-33
Interleukin-8
Interleukins
Transforming Growth Factor beta
Figure
Cited by 1 articles
-
Risk Factors for Acute Exacerbations in Elderly Asthma: What Makes Asthma in Older Adults Distinctive?
Kyoung-Hee Sohn, Woo-Jung Song, Jong-Sook Park, Heung-Woo Park, Tae-Bum Kim, Choon-Sik Park, Sang-Heon Cho,
Allergy Asthma Immunol Res. 2020;12(3):443-453. doi: 10.4168/aair.2020.12.3.443.
Reference
-
1. Hanania NA, King MJ, Braman SS, Saltoun C, Wise RA, Enright P, et al. Asthma in the elderly: Current understanding and future research needs--a report of a National Institute on Aging (NIA) workshop. J Allergy Clin Immunol. 2011; 128:S4–S24.
Article2. Gillman A, Douglass JA. Asthma in the elderly. Asia Pac Allergy. 2012; 2:101–108.
Article3. Park J, Kim TB, Joo H, Lee JS, Lee SD, Oh YM. Diseases concomitant with asthma in middle-aged and elderly subjects in Korea: a population-based study. Allergy Asthma Immunol Res. 2013; 5:16–25.
Article4. Park SY, Kim JH, Kim HJ, Seo B, Kwon OY, Chang HS, et al. High prevalence of asthma in elderly women: findings from a Korean national health database and adult asthma cohort. Allergy Asthma Immunol Res. 2018; 10:387–396.
Article5. Parameswaran K, Hildreth AJ, Chadha D, Keaney NP, Taylor IK, Bansal SK. Asthma in the elderly: underperceived, underdiagnosed and undertreated; a community survey. Respir Med. 1998; 92:573–577.
Article6. Moorman JE, Mannino DM. Increasing U.S. asthma mortality rates: who is really dying? J Asthma. 2001; 38:65–71.
Article7. Yáñez A, Cho SH, Soriano JB, Rosenwasser LJ, Rodrigo GJ, Rabe KF, et al. Asthma in the elderly: what we know and what we have yet to know. World Allergy Organ J. 2014; 7:8.
Article8. Mathur SK, Nyenhuis SM. Changes in immune function in asthma in the elderly. Aging Health. 2009; 5:551–559.
Article9. Murray MA, Chotirmall SH. The impact of immunosenescence on pulmonary disease. Mediators Inflamm. 2015; 2015:692546.
Article10. Hwang EK, Jin HJ, Nam YH, Shin YS, Ye YM, Nahm DH, et al. The predictors of poorly controlled asthma in elderly. Allergy Asthma Immunol Res. 2012; 4:270–276.
Article11. Di Salvo E, Ventura-Spagnolo E, Casciaro M, Navarra M, Gangemi S. IL-33/IL-31 axis: a potential inflammatory pathway. Mediators Inflamm. 2018; 2018:3858032.
Article12. Chai R, Liu B, Qi F. The significance of the levels of IL-4, IL-31 and TLSP in patients with asthma and/or rhinitis. Immunotherapy. 2017; 9:331–337.
Article13. Sidhu SS, Yuan S, Innes AL, Kerr S, Woodruff PG, Hou L, et al. Roles of epithelial cell-derived periostin in TGF-β activation, collagen production, and collagen gel elasticity in asthma. Proc Natl Acad Sci U S A. 2010; 107:14170–14175.
Article14. Coleman JM, Naik C, Holguin F, Ray A, Ray P, Trudeau JB, et al. Epithelial eotaxin-2 and eotaxin-3 expression: relation to asthma severity, luminal eosinophilia and age at onset. Thorax. 2012; 67:1061–1066.
Article15. Global Initiative for Asthma. Global strategy for asthma management and prevention [Internet]. place unknown: Global Initiative for Asthma;2018. Available from: http://www.ginasthma.org.16. Chung KF, Wenzel SE, Brozek JL, Bush A, Castro M, Sterk PJ, et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur Respir J. 2014; 43:343–373.17. Okamoto M, Hoshino T, Kitasato Y, Sakazaki Y, Kawayama T, Fujimoto K, et al. Periostin, a matrix protein, is a novel biomarker for idiopathic interstitial pneumonias. Eur Respir J. 2011; 37:1119–1127.
Article18. Baptist AP, Hao W, Karamched KR, Kaur B, Carpenter L, Song PX. Distinct asthma phenotypes among older adults with asthma. J Allergy Clin Immunol Pract. 2018; 6:244–249.e2.
Article19. Mathur SK. Allergy and asthma in the elderly. Semin Respir Crit Care Med. 2010; 31:587–595.
Article20. Kim MA, Shin SW, Park JS, Uh ST, Chang HS, Bae DJ, et al. Clinical characteristics of exacerbation prone adult asthmatics identified by cluster analysis. Allergy Asthma Immunol Res. 2017; 9:483–490.21. Hirano T, Matsunaga K. Late-onset asthma: current perspectives. J Asthma Allergy. 2018; 11:19–27.
Article22. Moskwa S, Piotrowski W, Marczak J, Pawełczyk M, Lewandowska-Polak A, Jarzębska M, et al. Innate immune response to viral infections in primary bronchial epithelial cells is modified by the atopic status of asthmatic patients. Allergy Asthma Immunol Res. 2018; 10:144–154.
Article23. Kim CK, Callaway Z, Gern JE. Viral infections and associated factors that promote acute exacerbations of asthma. Allergy Asthma Immunol Res. 2018; 10:12–17.
Article24. Barua P, O'Mahony MS. Overcoming gaps in the management of asthma in older patients: new insights. Drugs Aging. 2005; 22:1029–1059.25. Song WJ, Jee YK. More effective strategies are needed for elderly asthmatics in real-world practice. Allergy Asthma Immunol Res. 2015; 7:419–420.
Article26. Trinh HK, Ban GY, Lee JH, Park HS. Leukotriene receptor antagonists for the treatment of asthma in elderly patients. Drugs Aging. 2016; 33:699–710.
Article27. Choi GS, Shin YS, Kim JH, Choi SY, Lee SK, Nam YH, et al. Prevalence and risk factors for depression in Korean adult patients with asthma: is there a difference between elderly and non-elderly patients? J Korean Med Sci. 2014; 29:1626–1631.
Article28. Busse PJ, Zhang TF, Srivastava K, Schofield B, Li XM. Effect of ageing on pulmonary inflammation, airway hyperresponsiveness and T and B cell responses in antigen-sensitized and -challenged mice. Clin Exp Allergy. 2007; 37:1392–1403.
Article29. Busse PJ, Birmingham JM, Calatroni A, Manzi J, Goryachokovsky A, Fontela G, et al. Effect of aging on sputum inflammation and asthma control. J Allergy Clin Immunol. 2017; 139:1808–1818.e6.
Article30. Robinson D, Humbert M, Buhl R, Cruz AA, Inoue H, Korom S, et al. Revisiting type 2-high and type 2-low airway inflammation in asthma: current knowledge and therapeutic implications. Clin Exp Allergy. 2017; 47:161–175.
Article31. Ho JC, Chan KN, Hu WH, Lam WK, Zheng L, Tipoe GL, et al. The effect of aging on nasal mucociliary clearance, beat frequency, and ultrastructure of respiratory cilia. Am J Respir Crit Care Med. 2001; 163:983–988.
Article32. Svartengren M, Falk R, Philipson K. Long-term clearance from small airways decreases with age. Eur Respir J. 2005; 26:609–615.
Article33. Sjöberg LC, Nilsson AZ, Lei Y, Gregory JA, Adner M, Nilsson GP. Interleukin 33 exacerbates antigen driven airway hyperresponsiveness, inflammation and remodeling in a mouse model of asthma. Sci Rep. 2017; 7:4219.
Article34. Stolarski B, Kurowska-Stolarska M, Kewin P, Xu D, Liew FY. IL-33 exacerbates eosinophil-mediated airway inflammation. J Immunol. 2010; 185:3472–3480.
Article35. Ip WK, Wong CK, Li ML, Li PW, Cheung PF, Lam CW. Interleukin-31 induces cytokine and chemokine production from human bronchial epithelial cells through activation of mitogen-activated protein kinase signalling pathways: implications for the allergic response. Immunology. 2007; 122:532–541.
Article36. Lai T, Wu D, Li W, Chen M, Yi Z, Huang D, et al. Interleukin-31 expression and relation to disease severity in human asthma. Sci Rep. 2016; 6:22835.
Article37. Liu W, Luo R, Chen Y, Sun C, Wang J, Zhou L, et al. Interleukin-31 promotes helper T cell type-2 inflammation in children with allergic rhinitis. Pediatr Res. 2015; 77:20–28.
Article38. Vocca L, Di Sano C, Uasuf CG, Sala A, Riccobono L, Gangemi S, et al. IL-33/ST2 axis controls Th2/IL-31 and Th17 immune response in allergic airway diseases. Immunobiology. 2015; 220:954–963.
Article39. Al-Alawi M, Hassan T, Chotirmall SH. Transforming growth factor β and severe asthma: a perfect storm. Respir Med. 2014; 108:1409–1423.
Article40. Menzies-Gow A, Ying S, Sabroe I, Stubbs VL, Soler D, Williams TJ, et al. Eotaxin (CCL11) and eotaxin-2 (CCL24) induce recruitment of eosinophils, basophils, neutrophils, and macrophages as well as features of early- and late-phase allergic reactions following cutaneous injection in human atopic and nonatopic volunteers. J Immunol. 2002; 169:2712–2718.
Article41. Ben-Yehuda C, Bader R, Puxeddu I, Levi-Schaffer F, Breuer R, Berkman N. Airway eosinophil accumulation and eotaxin-2/CCL24 expression following allergen challenge in BALB/c mice. Exp Lung Res. 2008; 34:467–479.
Article42. Makinde T, Murphy RF, Agrawal DK. The regulatory role of TGF-β in airway remodeling in asthma. Immunol Cell Biol. 2007; 85:348–356.43. Kim MA, Izuhara K, Ohta S, Ono J, Yoon MK, Ban GY, et al. Association of serum periostin with aspirin-exacerbated respiratory disease. Ann Allergy Asthma Immunol. 2014; 113:314–320.
Article44. Izuhara K, Ohta S, Ono J. Using periostin as a biomarker in the treatment of asthma. Allergy Asthma Immunol Res. 2016; 8:491–498.
Article45. Parulekar AD, Atik MA, Hanania NA. Periostin, a novel biomarker of Th2-driven asthma. Curr Opin Pulm Med. 2014; 20:60–65.
Article46. Kim TB, Park CS, Bae YJ, Cho YS, Moon HB. COREA Study Group. Factors associated with severity and exacerbation of asthma: a baseline analysis of the cohort for reality and evolution of adult asthma in Korea (COREA). Ann Allergy Asthma Immunol. 2009; 103:311–317.
Article47. Sano H, Iwanaga T, Nishiyama O, Sano A, Higashimoto Y, Tomita K, et al. Characteristics of phenotypes of elderly patients with asthma. Allergol Int. 2016; 65:204–209.
Article48. Kim YK, Kim SH, Tak YJ, Jee YK, Lee BJ, Kim SH, et al. High prevalence of current asthma and active smoking effect among the elderly. Clin Exp Allergy. 2002; 32:1706–1712.
Article