Ann Surg Treat Res.
2018 Dec;95(6):297-302. 10.4174/astr.2018.95.6.297.
Preliminary study on application of augmented reality visualization in robotic thyroid surgery
- Affiliations
-
- 1Interdisciplinary Program, Bioengineering Major, Graduate School, Seoul National University, Seoul, Korea.
- 2Department of Biomedical Engineering, Chungnam National University Hospital, Chungnam National University College of Medicine, Daejeon, Korea.
- 3Department of Biomedical Engineering, Seoul National University Hospital, Seoul, Korea.
- 4Department of Surgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
- 5Department of Surgery, Seoul Metropolitan Government - Seoul National University Boramae Medical Center, Seoul, Korea. kevinjoon@naver.com
- 6Department of Biomedical Engineering, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
- 7Institute of Medical & Biological Engineering, Medical Research Center, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2426760
- DOI: http://doi.org/10.4174/astr.2018.95.6.297
Abstract
- PURPOSE
Increased robotic surgery is attended by increased reports of complications, largely due to limited operative view and lack of tactile sense. These kinds of obstacles, which seldom occur in open surgery, are challenging for beginner surgeons. To enhance robotic surgery safety, we created an augmented reality (AR) model of the organs around the thyroid glands, and tested the AR model applicability in robotic thyroidectomy.
METHODS
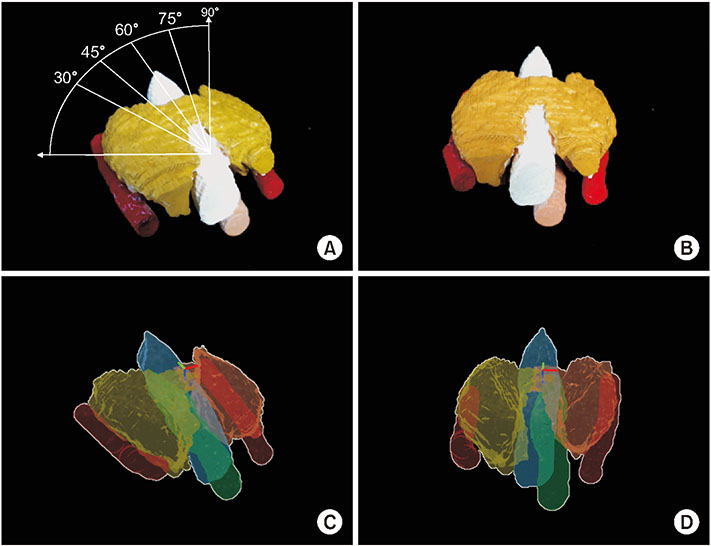
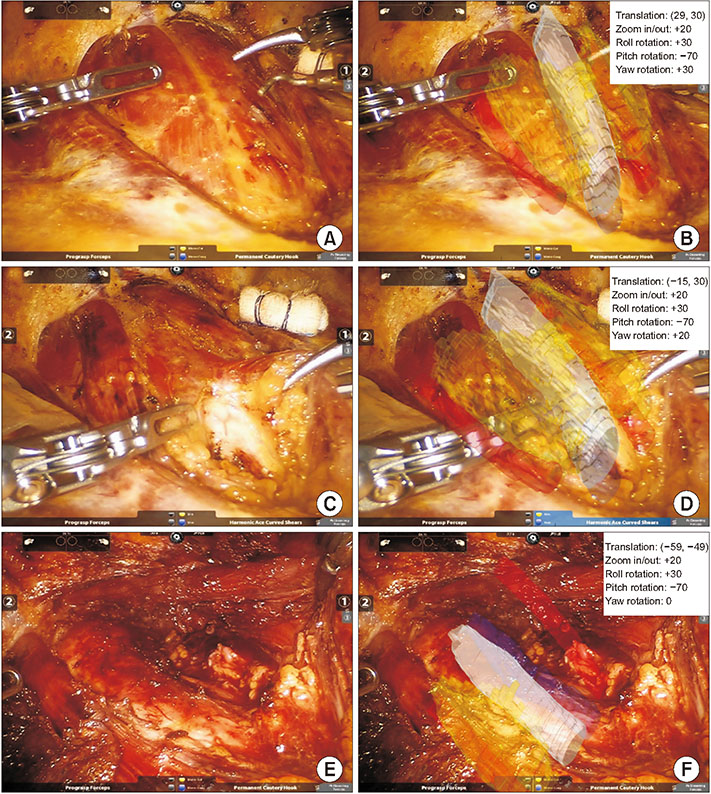
We created AR images of the thyroid gland, common carotid arteries, trachea, and esophagus using preoperative CT images of a thyroid carcinoma patient. For a preliminary test, we overlaid the AR images on a 3-dimensional printed model at five different angles and evaluated its accuracy using Dice similarity coefficient. We then overlaid the AR images on the real-time operative images during robotic thyroidectomy.
RESULTS
The Dice similarity coefficients ranged from 0.984 to 0.9908, and the mean of the five different angles was 0.987. During the entire process of robotic thyroidectomy, the AR images were successfully overlaid on the real-time operative images using manual registration.
CONCLUSION
We successfully demonstrated the use of AR on the operative field during robotic thyroidectomy. Although there are currently limitations, the use of AR in robotic surgery will become more practical as the technology advances and may contribute to the enhancement of surgical safety.
Keyword
MeSH Terms
Figure
Reference
-
1. Kang SW, Jeong JJ, Nam KH, Chang HS, Chung WY, Park CS. Robot-assisted endoscopic thyroidectomy for thyroid malignancies using a gasless transaxillary approach. J Am Coll Surg. 2009; 209:e1–e7.
Article2. Terris DJ, Singer MC, Seybt MW. Robotic facelift thyroidectomy: II. Clinical feasibility and safety. Laryngoscope. 2011; 121:1636–1641.
Article3. Kim HY, Chai YJ, Dionigi G, Anuwong A, Richmon JD. Transoral robotic thyroidectomy: lessons learned from an initial consecutive series of 24 patients. Surg Endosc. 2018; 32:688–694.
Article4. Chai YJ, Suh H, Woo JW, Yu HW, Song RY, Kwon H, et al. Surgical safety and oncological completeness of robotic thyroidectomy for thyroid carcinoma larger than 2 cm. Surg Endosc. 2017; 31:1235–1240.5. Chai YJ, Song J, Kang J, Woo JW, Song RY, Kwon H, et al. A comparative study of postoperative pain for open thyroidectomy versus bilateral axillo-breast approach robotic thyroidectomy using a self-reporting application for iPad. Ann Surg Treat Res. 2016; 90:239–245.
Article6. Landry CS, Grubbs EG, Warneke CL, Ormond M, Chua C, Lee JE, et al. Robot-assisted transaxillary thyroid surgery in the United States: is it comparable to open thyroid lobectomy? Ann Surg Oncol. 2012; 19:1269–1274.
Article7. Kandil EH, Noureldine SI, Yao L, Slakey DP. Robotic transaxillary thyroidectomy: an examination of the first one hundred cases. J Am Coll Surg. 2012; 214:558–564.
Article8. Ban EJ, Yoo JY, Kim WW, Son HY, Park S, Lee SH, et al. Surgical complications after robotic thyroidectomy for thyroid carcinoma: a single center experience with 3,000 patients. Surg Endosc. 2014; 28:2555–2563.
Article9. Lee S. Robotic thyroidectomy: pros and cons of various surgical approaches. Korean J Endocr Surg. 2015; 15:73–78.
Article10. Inabnet WB 3rd. Robotic thyroidectomy: must we drive a luxury sedan to arrive at our destination safely? Thyroid. 2012; 22:988–990.
Article11. Hansen C, Wieferich J, Ritter F, Rieder C, Peitgen HO. Illustrative visualization of 3D planning models for augmented reality in liver surgery. Int J Comput Assist Radiol Surg. 2010; 5:133–141.
Article12. Simpfendorfer T, Baumhauer M, Müller M, Gutt CN, Meinzer HP, Rassweiler JJ, et al. Augmented reality visualization during laparoscopic radical prostatectomy. J Endourol. 2011; 25:1841–1845.13. Haouchine N, Dequidt J, Berger MO, Cotin S. Deformation-based augmented reality for hepatic surgery. Stud Health Technol Inform. 2013; 184:182–188.14. Okamoto T, Onda S, Yanaga K, Suzuki N, Hattori A. Clinical application of navigation surgery using augmented reality in the abdominal field. Surg Today. 2015; 45:397–406.
Article15. Baumhauer M, Neuhaus J, Fritzsche K, Meinzer HP. The MITK image guided therapy toolkit and its exemplary application for augmented reality guided prostate surgery. In : Dossel Olaf, Schlegel WC, editors. Proceedings of World Congress on Medical Physics and Biomedical Engineering; Sep 7–12, 2009; Munich, Germany. IFMBE Proceedings, vol 25/6.16. Vemuri AS, Wu JC, Liu KC, Wu HS. Deformable three-dimensional model architecture for interactive augmented reality in minimally invasive surgery. Surg Endosc. 2012; 26:3655–3662.
Article17. Soler L, Nicolau S, Pessaux P, Mutter D, Marescaux J. Real-time 3D image reconstruction guidance in liver resection surgery. Hepatobiliary Surg Nutr. 2014; 3:73–81.18. Bodenstedt S, Goertler J, Wagner M, Kenngott H, Miller-Stich B, Dillmann R, et al. Superpixel-based structure classification for laparoscopic surgery. In : Medical Imaging 2016: Image-guided procedures, robotic interventions, and modeling; 2016 Feb 28-Mar 1; San Diego (CA).19. Bernhardt S, Nicolau SA, Soler L, Doignon C. The status of augmented reality in laparoscopic surgery as of 2016. Med Image Anal. 2017; 37:66–90.
Article20. Cheng A, Kang JU, Taylor RH, Boctor EM. Direct three-dimensional ultrasound-to-video registration using photoacoustic markers. J Biomed Opt. 2013; 18:066013.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Augmented Reality in Medicine
- Robotic Spine Surgery and Augmented Reality Systems: A State of the Art
- Enhancing recurrent laryngeal nerve localization during transoral endoscopic thyroid surgery using augmented reality: a proof-of-concept study
- The application of augmented reality for improving clinical skills: a scoping review
- The effect of utilizing augmented reality in a mobile application for sequential tooth carving by users