J Korean Med Assoc.
2018 Oct;61(10):623-629. 10.5124/jkma.2018.61.10.623.
Pharmacological treatment of osteoarthritis
- Affiliations
-
- 1Department of Rheumatology, Hanyang University Hospital for Rheumatic Diseases, Seoul, Korea. sungyk@hanyang.ac.kr
- KMID: 2426486
- DOI: http://doi.org/10.5124/jkma.2018.61.10.623
Abstract
- Osteoarthritis (OA) is a common chronic degenerative disease, and its prevalence increases with age. For patients with symptomatic OA, pharmacological treatment is suggested if symptoms and function do not improve with nonpharmacological modalities, including exercise, devices, manual therapy, or self-management programs. Attempts have been made to develop medications that prevent the structural progression of OA; however, the pharmacological treatment of OA has focused on the management of pain to improve the functional ability of joints. Clinicians try to prescribe adequate classes and doses of medications for pain relief, considering the affected parts of joints, each patient's comorbidities, and the clinical response to medical treatment, including tolerability and side effects. It is important to titrate the dose of medications as patients' symptoms change over time, maintaining the lowest effective dose for each individual.
Keyword
MeSH Terms
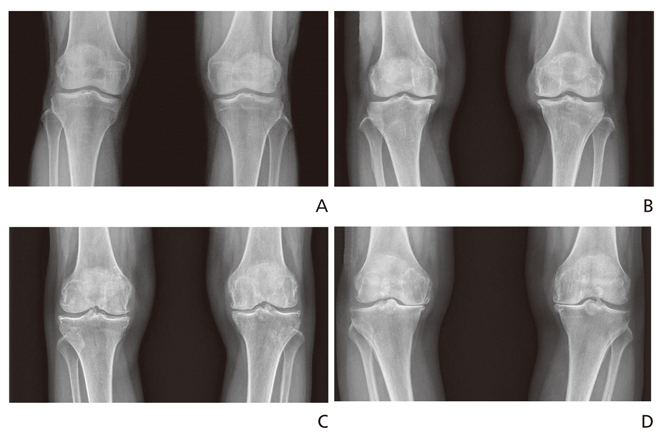
Figure
Reference
-
1. Loeser RF, Goldring SR, Scanzello CR, Goldring MB. Osteoarthritis: a disease of the joint as an organ. Arthritis Rheum. 2012; 64:1697–1707.
Article2. Cho NH, Kim S, Kim HA, Seo YI. The prevalence and risk factors of knee and hand osteoarthritis in Korea. J Korean Rheum Assoc. 2007; 14:354–362.
Article3. Park JH, Hong JY, Han K, Suh SW, Park SY, Yang JH, Han SW. Prevalence of symptomatic hip, knee, and spine osteoarthritis nationwide health survey analysis of an elderly Korean population. Medicine (Baltimore). 2017; 96:e6372.
Article4. Bijlsma JW, Berenbaum F, Lafeber FP. Osteoarthritis: an update with relevance for clinical practice. Lancet. 2011; 377:2115–2126.
Article5. Kim H, Cho SK, Kim D, Kim D, Jung SY, Jang EJ, Sung YK. Impact of osteoarthritis on household catastrophic health expenditures in Korea. J Korean Med Sci. 2018; 33:e161.
Article6. Park HR, Cho SK, Im SG, Jung SY, Kim D, Jang EJ, Sung YK. Treatment patterns of knee osteoarthritis patients in Korea. Korean J Intern Med. 2018; 03. 21. [Epub]. DOI: 10.3904/kjim.2017.304.
Article7. Machado GC, Maher CG, Ferreira PH, Pinheiro MB, Lin CW, Day RO, McLachlan AJ, Ferreira ML. Efficacy and safety of paracetamol for spinal pain and osteoarthritis: systematic review and meta-analysis of randomised placebo controlled trials. BMJ. 2015; 350:h1225.
Article8. Jordan KM, Arden NK, Doherty M, Bannwarth B, Bijlsma JW, Dieppe P, Gunther K, Hauselmann H, Herrero-Beaumont G, Kaklamanis P, Lohmander S, Leeb B, Lequesne M, Mazieres B, Martin-Mola E, Pavelka K, Pendleton A, Punzi L, Serni U, Swoboda B, Verbruggen G, Zimmerman-Gorska I, Dougados M. Standing Committee for International Clinical Studies Including Therapeutic Trials ESCISIT. EULAR Recommendations 2003: an evidence based approach to the management of knee osteoarthritis: Report of a Task Force of the Standing Committee for International Clinical Studies Including Therapeutic Trials (ESCISIT). Ann Rheum Dis. 2003; 62:1145–1155.9. Roberts E, Delgado Nunes V, Buckner S, Latchem S, Constanti M, Miller P, Doherty M, Zhang W, Birrell F, Porcheret M, Dziedzic K, Bernstein I, Wise E, Conaghan PG. Paracetamol: not as safe as we thought? A systematic literature review of observational studies. Ann Rheum Dis. 2016; 75:552–559.
Article10. Hochberg MC, Altman RD, April KT, Benkhalti M, Guyatt G, McGowan J, Towheed T, Welch V, Wells G, Tugwell P. American College of Rheumatology. American College of Rheumatology 2012 recommendations for the use of non-pharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res (Hoboken). 2012; 64:465–474.
Article11. Kim D, Cho SK, Nam SW, Kwon HH, Jung SY, Jeon CH, Im SG, Kim D, Jang EJ, Sung YK. Cardiovascular and gastrointestinal effects of etoricoxib in the treatment of osteo-arthritis: a systematic review and network meta-analysis. J Rheum Dis. 2017; 24:293–302.
Article12. Freedberg DE, Kim LS, Yang YX. The risks and benefits of long-term use of proton pump inhibitors: expert review and best practice advice from the American Gastroenterological Association. Gastroenterology. 2017; 152:706–715.
Article13. Patrono C, Baigent C. Nonsteroidal anti-inflammatory drugs and the heart. Circulation. 2014; 129:907–916.
Article14. White WB, West CR, Borer JS, Gorelick PB, Lavange L, Pan SX, Weiner E, Verburg KM. Risk of cardiovascular events in patients receiving celecoxib: a meta-analysis of randomized clinical trials. Am J Cardiol. 2007; 99:91–98.
Article15. Xu C, Gu K, Yasen Y, Hou Y. Efficacy and safety of celecoxib therapy in osteoarthritis: a meta-analysis of randomized controlled trials. Medicine (Baltimore). 2016; 95:e3585.16. Nissen SE, Yeomans ND, Solomon DH, Luscher TF, Libby P, Husni ME, Graham DY, Borer JS, Wisniewski LM, Wolski KE, Wang Q, Menon V, Ruschitzka F, Gaffney M, Beckerman B, Berger MF, Bao W, Lincoff AM. PRECISION Trial Investigators. Cardiovascular safety of celecoxib, naproxen, or ibuprofen for arthritis. N Engl J Med. 2016; 375:2519–2529.
Article17. Jung SY, Jang EJ, Choi S, Im SG, Cho SK, Kim H, Sung YK. The effect of national drug utilization review system on non-steroid anti-inflammatory drug therapeutic duplication among knee osteoarthritis patients in the Korea. J Rheum Dis. 2018; 25:Suppl 1. S207.18. Smith SR, Deshpande BR, Collins JE, Katz JN, Losina E. Comparative pain reduction of oral non-steroidal anti-inflammatory drugs and opioids for knee osteoarthritis: systematic analytic review. Osteoarthritis Cartilage. 2016; 24:962–972.
Article19. Jung SY, Jang EJ, Nam SW, Kwon HH, Im SG, Kim D, Cho SK, Kim D, Sung YK. Comparative effectiveness of oral pharmacologic interventions for knee osteoarthritis: a network meta-analysis. Mod Rheumatol. 2018; 03. 01. [Epub]. DOI: 10.1080/14397595.2018.1439694.
Article20. Zhang W, Nuki G, Moskowitz RW, Abramson S, Altman RD, Arden NK, Bierma-Zeinstra S, Brandt KD, Croft P, Doherty M, Dougados M, Hochberg M, Hunter DJ, Kwoh K, Lohmander LS, Tugwell P. OARSI recommendations for the management of hip and knee osteoarthritis: part III: changes in evidence following systematic cumulative update of research published through January 2009. Osteoarthritis Cartilage. 2010; 18:476–499.
Article21. Wang G, Bi L, Li X, Li Z, Zhao D, Chen J, He D, Wang CN, Duenas H, Skljarevski V, Yue L. Efficacy and safety of duloxetine in Chinese patients with chronic pain due to osteoarthritis: a randomized, double-blind, placebo-controlled study. Osteoarthritis Cartilage. 2017; 25:832–838.
Article22. Myers J, Wielage RC, Han B, Price K, Gahn J, Paget MA, Happich M. The efficacy of duloxetine, non-steroidal anti-inflammatory drugs, and opioids in osteoarthritis: a systema-tic literature review and meta-analysis. BMC Musculoskelet Disord. 2014; 15:76.
Article23. Zhang W, Doherty M, Leeb BF, Alekseeva L, Arden NK, Bijlsma JW, Dincer F, Dziedzic K, Hauselmann HJ, Herrero-Beaumont G, Kaklamanis P, Lohmander S, Maheu E, Martín-Mola E, Pavelka K, Punzi L, Reiter S, Sautner J, Smolen J, Verbruggen G, Zimmermann-Gorska I. EULAR evidence based recommendations for the management of hand osteoarthritis: report of a Task Force of the EULAR Standing Committee for International Clinical Studies Including Therapeutics (ESCISIT). Ann Rheum Dis. 2007; 66:377–388.
Article24. Cho SK, Kim H, Park HR, Choi W, Choi S, Jung S, Jang EJ, Sung YK. NSAID sparing effect of symptomatic slow acting drugs for osteoarthritis (SYSADOA) in knee osteoarthritis patients. J Rheum Dis. 2018; 25:Suppl 1. S266.25. Reginster JY, Deroisy R, Rovati LC, Lee RL, Lejeune E, Bruyere O, Giacovelli G, Henrotin Y, Dacre JE, Gossett C. Long-term effects of glucosamine sulphate on osteoarthritis progression: a randomised, placebo-controlled clinical trial. Lancet. 2001; 357:251–256.
Article26. Clegg DO, Reda DJ, Harris CL, Klein MA, O'Dell JR, Hooper MM, Bradley JD, Bingham CO 3rd, Weisman MH, Jackson CG, Lane NE, Cush JJ, Moreland LW, Schumacher HR Jr, Oddis CV, Wolfe F, Molitor JA, Yocum DE, Schnitzer TJ, Furst DE, Sawitzke AD, Shi H, Brandt KD, Moskowitz RW, Williams HJ. Glucosamine, chondroitin sulfate, and the two in combination for painful knee osteoarthritis. N Engl J Med. 2006; 354:795–808.
Article27. Kongtharvonskul J, Anothaisintawee T, McEvoy M, Attia J, Woratanarat P, Thakkinstian A. Efficacy and safety of glucosamine, diacerein, and NSAIDs in osteoarthritis knee: a systematic review and network meta-analysis. Eur J Med Res. 2015; 20:24.
Article28. Zeng C, Wei J, Li H, Wang YL, Xie DX, Yang T, Gao SG, Li YS, Luo W, Lei GH. Effectiveness and safety of Glucosamine, chondroitin, the two in combination, or celecoxib in the treatment of osteoarthritis of the knee. Sci Rep. 2015; 5:16827.
Article29. Mazieres B, Combe B, Phan Van A, Tondut J, Grynfeltt M. Chondroitin sulfate in osteoarthritis of the knee: a prospective, double blind, placebo controlled multicenter clinical study. J Rheumatol. 2001; 28:173–181.30. Hochberg MC, Zhan M, Langenberg P. The rate of decline of joint space width in patients with osteoarthritis of the knee: a systematic review and meta-analysis of randomized placebo-controlled trials of chondroitin sulfate. Curr Med Res Opin. 2008; 24:3029–3035.
Article31. Christensen R, Bartels EM, Astrup A, Bliddal H. Symptomatic efficacy of avocado-soybean unsaponifiables (ASU) in osteoarthritis (OA) patients: a meta-analysis of randomized controlled trials. Osteoarthritis Cartilage. 2008; 16:399–408.
Article32. van Middelkoop M, Arden NK, Atchia I, Birrell F, Chao J, Rezende MU, Lambert RG, Ravaud P, Bijlsma JW, Doherty M, Dziedzic KS, Lohmander LS, McAlindon TE, Zhang W, Bierma-Zeinstra SM. The OA Trial Bank: meta-analysis of individual patient data from knee and hip osteoarthritis trials show that patients with severe pain exhibit greater benefit from intra-articular glucocorticoids. Osteoarthritis Cartilage. 2016; 24:1143–1152.
Article33. McAlindon TE, LaValley MP, Harvey WF, Price LL, Driban JB, Zhang M, Ward RJ. Effect of intra-articular triamcinolone vs saline on knee cartilage volume and pain in patients with knee osteoarthritis: a randomized clinical trial. JAMA. 2017; 317:1967–1975.
Article34. Cooper C, Rannou F, Richette P, Bruyere O, Al-Daghri N, Altman RD, Brandi ML, Collaud Basset S, Herrero-Beaumont G, Migliore A, Pavelka K, Uebelhart D, Reginster JY. Use of intraarticular hyaluronic acid in the management of knee osteoarthritis in clinical practice. Arthritis Care Res (Hobo-ken). 2017; 69:1287–1296.
Article35. Cho J, Kim T, Park Y, Shin J, Kang S, Lee B. Invossa (Tissue-gene-C) in patients with osteoarthritis: a phase III trial. Osteo-arthritis Cartilage. 2016; 24(Supp 1):S190.