J Korean Med Assoc.
2018 Nov;61(11):680-686. 10.5124/jkma.2018.61.11.680.
Pharmacological treatment options for acne
- Affiliations
-
- 1Department of Dermatology, Chung-Ang University College of Medicine, Seoul, Korea. kyky@caumc.or.kr
- KMID: 2426478
- DOI: http://doi.org/10.5124/jkma.2018.61.11.680
Abstract
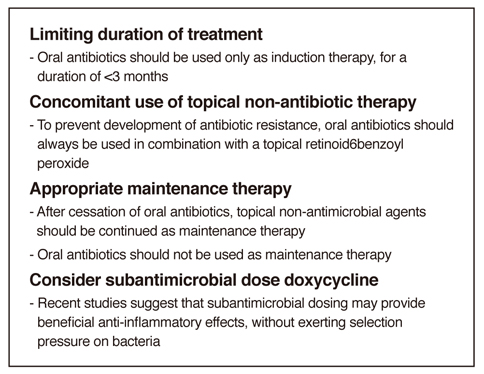
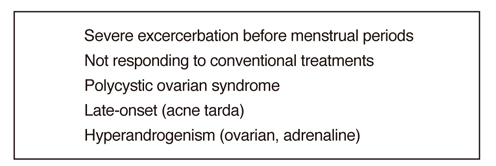
- Acne vulgaris is a very common condition affecting up of about 80% to 90% of adolescents. The patients with acne have been shown to be adversely impacted by the effect of acne on their quality of life. Four factors are believed to play a key role in the development of acne lesions: excess sebum production, disturbed keratinization within the follicle, colonization of the pilosebaceous duct by Propionibacterium acnes, and the release of inflammatory mediators into the skin. Consequently, the target for acne therapy is these well-known pathogenic factors responsible for this disease state. Topical retinoids correct abnormal keratinization, but it should be applied cautiously because of irritation. Benzoyl peroxide is an effective bactericidal agent against P. acnes. Main topical antibiotics are erythromycin and clindamycin. Fixed combination topical products with retinoids, benzoyl peroxide and antibiotics have been introduced. Use of systemic antibiotics, including tetracyclines and macrolides rapidly improves inflammatory acne lesions. Oral isotretinoin is effective against all of the main pathogenic features of acne but is contraindicated in pregnant women and has been associated with cheilitis and dry skin. Hormonal therapy has been found to improve acne in some selective patients and should be considered for appropriate candidates. This review will present the general aspects of the pharmacological treatments for acne.
Keyword
MeSH Terms
-
Acne Vulgaris*
Adolescent
Anti-Bacterial Agents
Benzoyl Peroxide
Cheilitis
Clindamycin
Colon
Drug Therapy
Erythromycin
Female
Humans
Isotretinoin
Macrolides
Pregnant Women
Propionibacterium acnes
Quality of Life
Retinoids
Sebum
Skin
Tetracyclines
Anti-Bacterial Agents
Benzoyl Peroxide
Clindamycin
Erythromycin
Isotretinoin
Macrolides
Retinoids
Tetracyclines
Figure
Reference
-
1. Zaenglein AL, Pathy AL, Schlosser BJ, Alikhan A, Baldwin HE, Berson DS, Bowe WP, Graber EM, Harper JC, Kang S, Keri JE, Leyden JJ, Reynolds RV, Silverberg NB, Stein Gold LF, Tollefson MM, Weiss JS, Dolan NC, Sagan AA, Stern M, Boyer KM, Bhushan R. Guidelines of care for the management of acne vulgaris. J Am Acad Dermatol. 2016; 74:945–973.e33.
Article2. Le Cleach L, Lebrun-Vignes B, Bachelot A, Beer F, Berger P, Brugere S, Chastaing M, Do-Pham G, Ferry T, Gand-Gavanou J, Guigues B, Join-Lambert O, Henry P, Khallouf R, Lavie E, Maruani A, Romain O, Sassolas B, Tran VT, Guillot B. French Acne Guidelines Working Group and Centre of Evidence of Dermatology. Guidelines for the management of acne: recommendations from a French multidisciplinary group. Br J Dermatol. 2017; 177:908–913.
Article3. Leyden J, Stein-Gold L, Weiss J. Why topical retinoids are mainstay of therapy for acne. Dermatol Ther (Heidelb). 2017; 7:293–304.
Article4. Farrah G, Tan E. The use of oral antibiotics in treating acne vulgaris: a new approach. Dermatol Ther. 2016; 29:377–384.
Article5. Tolkachjov SN, Sahoo A, Patel NG, Lohse CM, Murray JA, Tollefson MM. Surgical outcomes of patients on isotretinoin in the perioperative period: a single-center, retrospective analysis. J Am Acad Dermatol. 2017; 77:159–161.
Article6. Saluja SS, Walker ML, Summers EM, Tristani-Firouzi P, Smart DR. Safety of non-ablative fractional laser for acne scars within 1 month after treatment with oral isotretinoin: a randomized split-face controlled trial. Lasers Surg Med. 2017; 49:886–890.
Article7. Arowojolu AO, Gallo MF, Lopez LM, Grimes DA, Garner SE. Combined oral contraceptive pills for treatment of acne. Cochrane Database Syst Rev. 2009; (3):CD004425.
Article8. Brown J, Farquhar C, Lee O, Toomath R, Jepson RG. Spironolactone versus placebo or in combination with steroids for hirsutism and/or acne. Cochrane Database Syst Rev. 2009; (2):CD000194.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Innovative Use of Negative Air Ions As an Alternative Therapy for Acne Vulgaris: A Report of Three Cases
- Acne Conglobata Induced by Anabolic Androgenic Steroids
- Treatment of Acne
- The Quality of Life of Acne Patients
- Development of an effective formulation for an acne treatment cream with Ocimum basilicum using invasomes