J Neurocrit Care.
2018 Jun;11(1):58-62. 10.18700/jnc.180040.
Successful Endovascular Thrombectomy in a Patient with Monocular Blindness Due to Thrombus of the Ophthalmic Artery Orifice
- Affiliations
-
- 1Department of Neurology, Keimyung University Dongsan Medical Center, Korea. neurohong79@gmail.com
- KMID: 2426216
- DOI: http://doi.org/10.18700/jnc.180040
Abstract
- BACKGROUND
Retinal artery occlusion can lead to sudden visual loss without pain. The acute management of retinal artery occlusion remains unresolved.
CASE REPORT
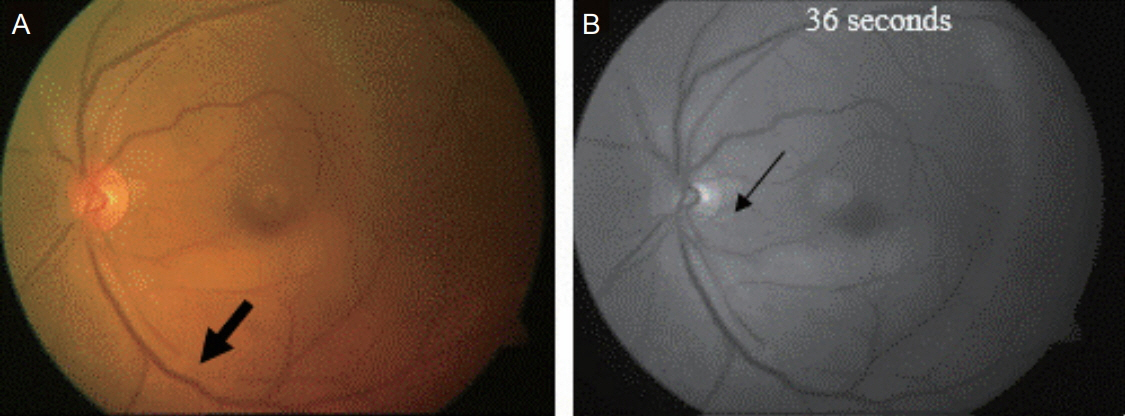
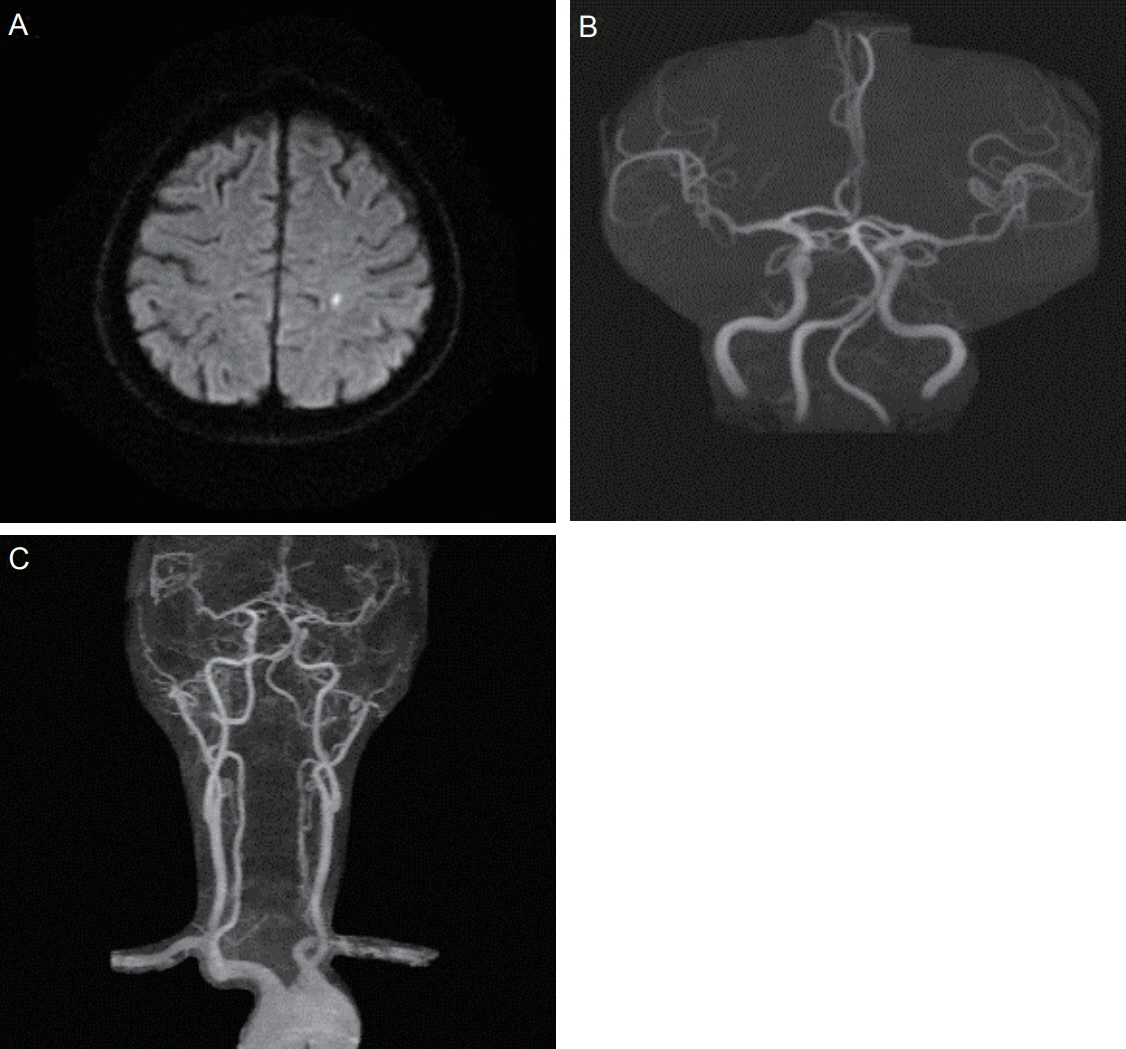
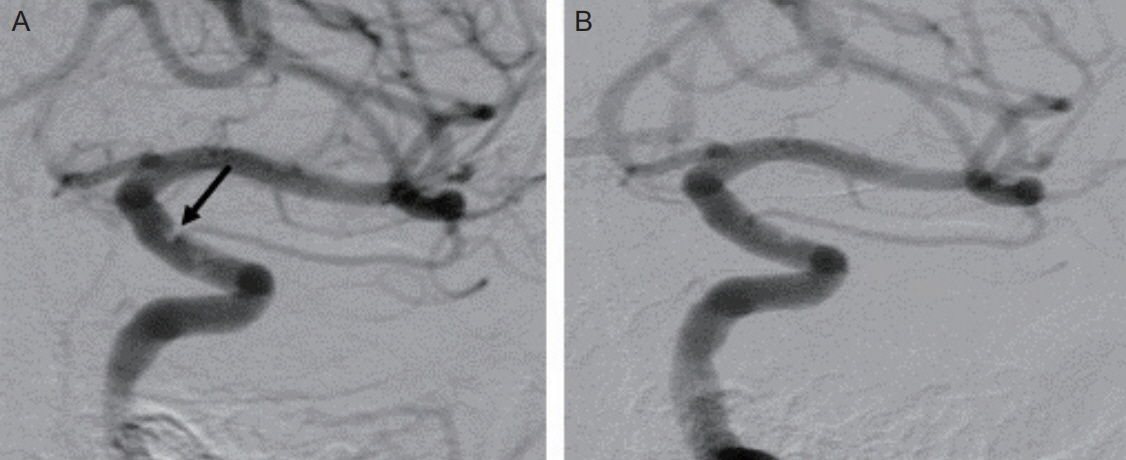
A 65-year-old male was hospitalized to an emergency room for visual loss on the left side within 6 hours of onset. Combined occlusion at retinal artery and ciliary artery was confirmed by an ophthalmologist and we assessed ophthalmic artery occlusion. However, MRA revealed no significant steno-occlusion of internal carotid artery. Transfemoral cerebral angiography was carried out immediately and showed a movable thrombus at the orifice of the ophthalmic artery. We decided on endovascular thrombectomy to prevent permanent visual loss. Finally, his visual acuity was improved after successful thrombectomy.
CONCLUSIONS
Although MRA is intact, small thrombus right at the orifice of the ophthalmic artery can cause a sudden monocular visual loss due to occlusion of the retinal artery. In this setting, urgent endovascular thrombectomy can offer visual improvement.
Keyword
MeSH Terms
Figure
Reference
-
1. Leavitt JA, Larson TA, Hodge DO, Gullerud RE. The incidence of central retinal artery occlusion in Olmsted County, Minnesota. Am J Ophthalmol. 2011; 152:820–3. e2.
Article2. Park SJ, Choi NK, Seo KH, Park KH, Woo SJ. Nationwide incidence of clinically diagnosed central retinal artery occlusion in Korea, 2008 to 2011. Ophthalmology. 2014; 121:1933–8.
Article3. Yuzurihara D, Iijima H. Visual outcome in central retinal and branch retinal artery occlusion. Jpn J Ophthalmol. 2004; 48:490–2.
Article4. Schumacher M, Schmidt D, Jurklies B, Gall C, Wanke I, Schmoor C, et al. Central retinal artery occlusion: local intraarterial fibrinolysis versus conservative treatment, a multicenter randomized trial. Ophthalmology. 2010; 117:1367–75. e1.
Article5. Hong JH, Sohn SI, Kwak J, Yoo J, Ahn SJ, Woo SJ, et al. Retinal artery occlusion and associated recurrent vascular risk with underlying etiologies. PLoS One. 2017; 12:e0177663.
Article6. Shin JW, Jeong JH, Jeong HY, Kim D, Moon J, Kim TJ, et al. Etiologies and vascular risk factors in patients with central retinal artery occlusion treated by intra-arterial thrombolysis. J Korean Neurol Assoc. 2012; 30:377–8.7. Babikian V, Wijman CA, Koleini B, Malik SN, Goyal N, Matjucha IC. Retinal ischemia and embolism. Etiologies and outcomes based on a prospective study. Cerebrovasc Dis. 2001; 12:108–13.8. Helenius J, Arsava EM, Goldstein JN, Cestari DM, Buonanno FS, Rosen BR, et al. Concurrent acute brain infarcts in patients with monocular visual loss. Ann Neurol. 2012; 72:286–93.
Article9. Cho KH, Kim CK, Woo SJ, Park KH, Park SJ. Cerebral small vessel disease in branch retinal artery occlusion. Invest Ophthalmol Vis Sci. 2016; 57:5818–24.
Article10. Schrag M, Youn T, Schindler J, Kirshner H, Greer D. Intravenous fibrinolytic therapy in central retinal artery occlusion: a patient-level meta-analysis. JAMA Neurol. 2015; 72:1148–54.11. Ahn SJ, Kim JM, Hong JH, Woo SJ, Ahn J, Park KH, et al. Efficacy and safety of intra-arterial thrombolysis in central retinal artery occlusion. Invest Ophthalmol Vis Sci. 2013; 54:7746–55.
Article12. Hwang GJ, Woo SJ, Hwang JM, Jung C, Park KH, Kwon OK. Reversal of ischemic retinopathy following balloon angioplasty of a stenotic ophthalmic artery. J Neuroophthalmol. 2010; 30:228–30.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Traditional Thrombus Composition and Related Endovascular Outcomes: Catching up with the Recent Evidence
- Real-Time Visualization of Thrombus during Suction Thrombectomy : Contrast-in-Stasis Technique
- Delayed Monocular Blindness after Coil Embolization of Large Paraclinoid Aneurysm
- Ophthalmic Artery ‘Steal’ Phenomenon as a Possible Mechanism of Transient Monocular Blindness in Internal Carotid Artery Dissection
- Transcarotid Mechanical Thrombectomy for Embolic Intracranial Large Vessel Occlusion after Endovascular Deconstructice Embolization for Carotid Blowout Syndrome