Cancer Res Treat.
2018 Oct;50(4):1260-1269. 10.4143/crt.2017.443.
Score for the Survival Probability in Metastasis Breast Cancer: A Nomogram-Based Risk Assessment Model
- Affiliations
-
- 1Department of Breast Surgery, Sun Yat-sen University Cancer Center, Guangzhou, China. wangxi@sysucc.org.cn
- 2State Key Laboratory of Oncology in Southern China, Guangzhou, China.
- 3Collaborative Innovation Center for Cancer Medicine, Guangzhou, China.
- KMID: 2424798
- DOI: http://doi.org/10.4143/crt.2017.443
Abstract
- PURPOSE
Survival of metastatic breast cancer (MBC) patient remains unknown and varies greatly from person to person. Thus, we aimed to construct a nomogram to quantify the survival probability of patients with MBC.
MATERIALS AND METHODS
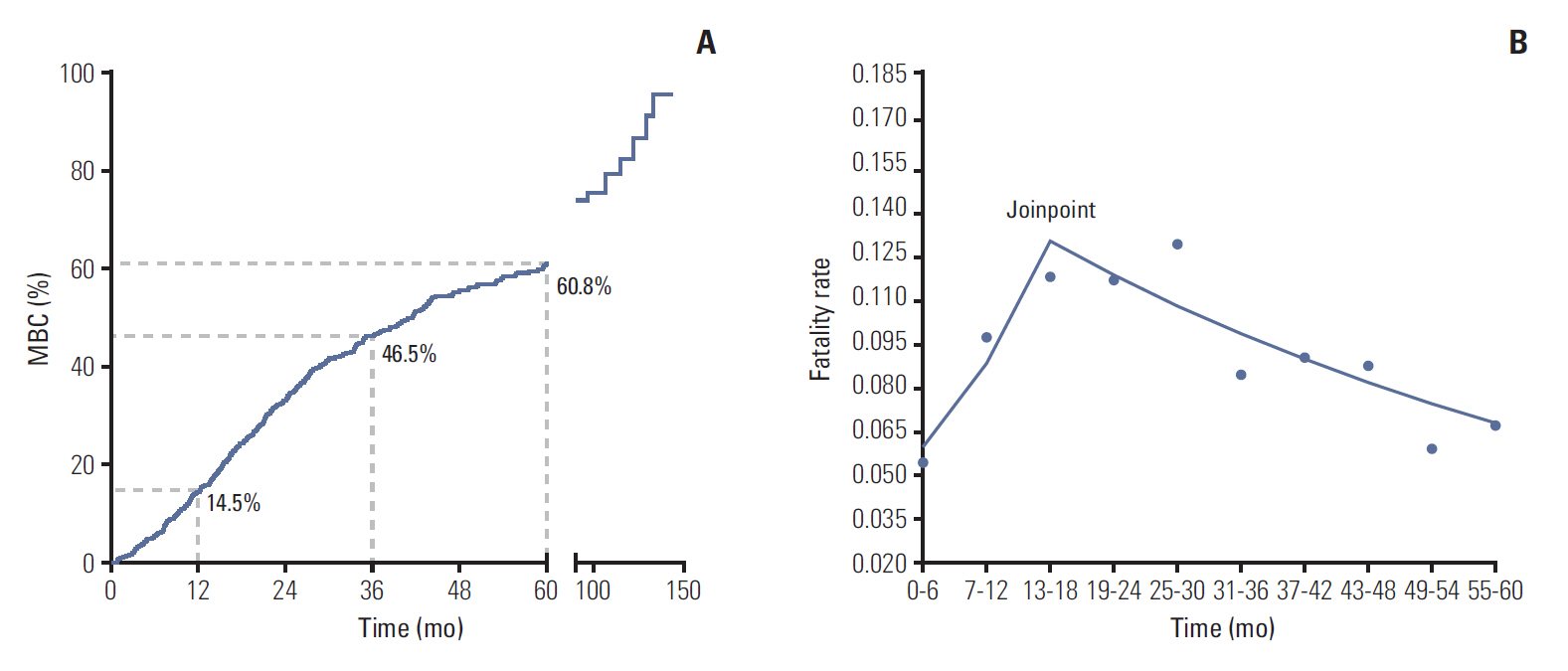
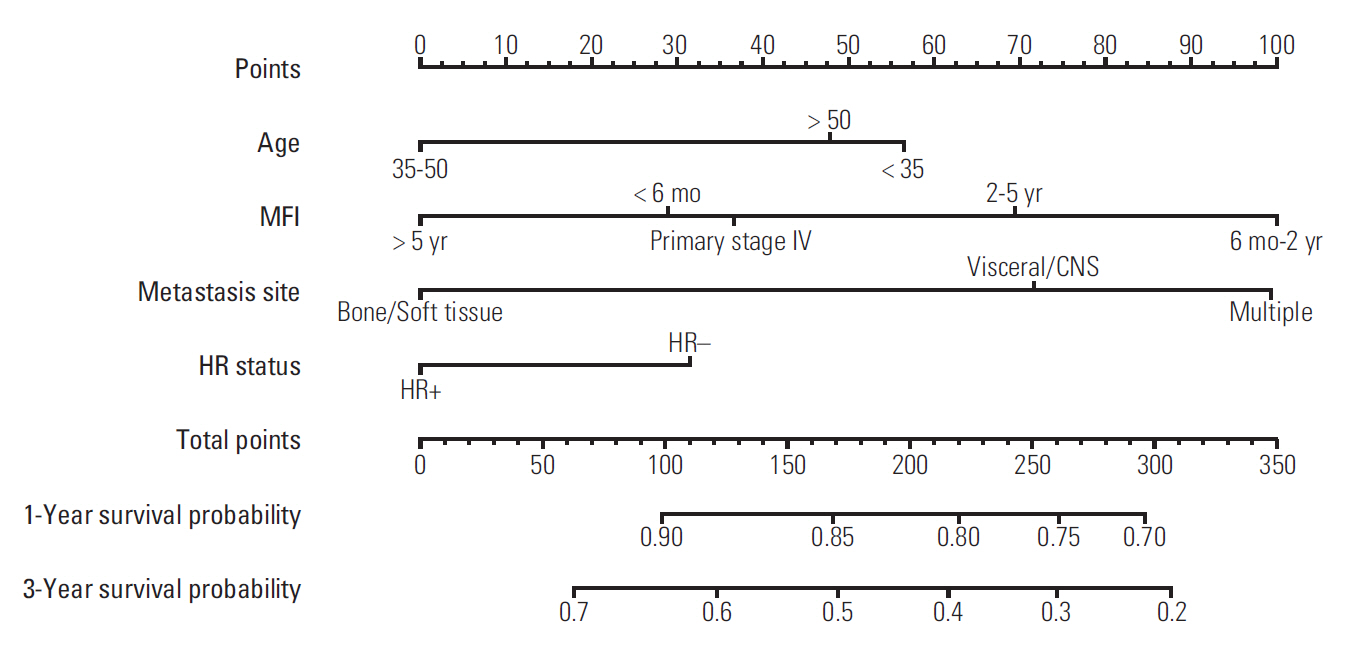
We had included 793 MBC patients and calculated trends of case fatality rate by Kaplan-Meier method and joinpoint regression. Six hundred thirty-four patients with MBC between January 2004 and July 2011 and 159 patients with MBC between August 2011 and July 2013 were assigned to training cohort and internal validation cohort, respectively. We constructed the nomogram based on the results of univariable and multivariable Cox regression analyses in the training cohort and validated the nomogram in the validation cohort. Concordance index and calibration curves were used to assess the effectiveness of nomogram.
RESULTS
Case fatality rate of MBC was increasing (annual percentage change [APC], 21.6; 95% confidence interval [CI], 1.0 to 46.3; p < 0.05) in the first 18 months and then decreased (APC, -4.5; 95% CI, -8.2 to -0.7; p < 0.05). Metastasis-free interval, age, metastasis location, and hormone receptor status were independent prognostic factors and were included in the nomogram, which had a concordance index of 0.69 in the training cohort and 0.67 in the validation cohort. Calibration curves indicated good consistency between the two cohorts at 1 and 3 years.
CONCLUSION
In conclusion, the fatality risk of MBC was increasing and reached the summit between 13th and 18th month after the detection of MBC. We have developed and validated a nomogram to predict the 1- and 3-year survival probability in MBC.
Keyword
MeSH Terms
Figure
Reference
-
References
1. DeSantis C, Ma J, Bryan L, Jemal A. Breast cancer statistics, 2013. CA Cancer J Clin. 2014; 64:52–62.
Article2. Miao H, Hartman M, Bhoo-Pathy N, Lee SC, Taib NA, Tan EY, et al. Predicting survival of de novo metastatic breast cancer in Asian women: systematic review and validation study. PLoS One. 2014; 9:e93755.
Article3. Cardoso F, Costa A, Senkus E, Aapro M, Andre F, Barrios CH, et al. 3rd ESO-ESMO International Consensus Guidelines for Advanced Breast Cancer (ABC 3). Ann Oncol. 2017; 28:16–33.
Article4. Turner NC, Neven P, Loibl S, Andre F. Advances in the treatment of advanced oestrogen-receptor-positive breast cancer. Lancet. 2017; 389:2403–14.
Article5. Harbeck N, Gnant M. Breast cancer. Lancet. 2017; 389:1134–50.
Article6. Amin MB, Greene FL, Edge SB, Compton CC, Gershenwald JE, Brookland RK, et al. The eighth edition AJCC cancer staging manual: continuing to build a bridge from a population-based to a more "personalized" approach to cancer staging. CA Cancer J Clin. 2017; 67:93–9.
Article7. MammaPrint reduces breast cancer overtreatment. Cancer Discov. 2016; 6:OF4.8. Kennecke H, Yerushalmi R, Woods R, Cheang MC, Voduc D, Speers CH, et al. Metastatic behavior of breast cancer subtypes. J Clin Oncol. 2010; 28:3271–7.
Article9. Lin C, Liao W, Jian Y, Peng Y, Zhang X, Ye L, et al. CGI-99 promotes breast cancer metastasis via autocrine interleukin-6 signaling. Oncogene. 2017; 36:3695–705.
Article10. Lee ES, Jung SY, Kim JY, Kim JJ, Yoo TK, Kim YG, et al. Identifying the potential long-term survivors among breast cancer patients with distant metastasis. Ann Oncol. 2016; 27:828–33.
Article11. den Brok WD, Speers CH, Gondara L, Baxter E, Tyldesley SK, Lohrisch CA. Survival with metastatic breast cancer based on initial presentation, de novo versus relapsed. Breast Cancer Res Treat. 2017; 161:549–56.
Article12. Eng LG, Dawood S, Sopik V, Haaland B, Tan PS, Bhoo-Pathy N, et al. Ten-year survival in women with primary stage IV breast cancer. Breast Cancer Res Treat. 2016; 160:145–52.
Article13. Lobbezoo DJ, van Kampen RJ, Voogd AC, Dercksen MW, van den Berkmortel F, Smilde TJ, et al. Prognosis of metastatic breast cancer: are there differences between patients with de novo and recurrent metastatic breast cancer? Br J Cancer. 2015; 112:1445–51.
Article14. Wang H, Zhang C, Zhang J, Kong L, Zhu H, Yu J. The prognosis analysis of different metastasis pattern in patients with different breast cancer subtypes: a SEER based study. Oncotarget. 2017; 8:26368–79.
Article15. Rapiti E, Verkooijen HM, Vlastos G, Fioretta G, Neyroud-Caspar I, Sappino AP, et al. Complete excision of primary breast tumor improves survival of patients with metastatic breast cancer at diagnosis. J Clin Oncol. 2006; 24:2743–9.
Article16. Gong Y, Liu YR, Ji P, Hu X, Shao ZM. Impact of molecular subtypes on metastatic breast cancer patients: a SEER population-based study. Sci Rep. 2017; 7:45411.
Article17. Robertson JF, Bondarenko IM, Trishkina E, Dvorkin M, Panasci L, Manikhas A, et al. Fulvestrant 500 mg versus anastrozole 1 mg for hormone receptor-positive advanced breast cancer (FALCON): an international, randomised, double-blind, phase 3 trial. Lancet. 2016; 388:2997–3005.
Article18. Denkert C, Liedtke C, Tutt A, von Minckwitz G. Molecular alterations in triple-negative breast cancer: the road to new treatment strategies. Lancet. 2017; 389:2430–42.19. Graesslin O, Abdulkarim BS, Coutant C, Huguet F, Gabos Z, Hsu L, et al. Nomogram to predict subsequent brain metastasis in patients with metastatic breast cancer. J Clin Oncol. 2010; 28:2032–7.
Article20. Lim YJ, Lee SW, Choi N, Kwon J, Eom KY, Kang E, et al. A novel prognostic nomogram for predicting risks of distant failure in patients with invasive breast cancer following postoperative adjuvant radiotherapy. Cancer Res Treat. 2018; 50:1140–8.
Article21. Kim MK, Han W, Moon HG, Ahn SK, Kim J, Lee JW, et al. Nomogram for predicting breast conservation after neoadjuvant chemotherapy. Cancer Res Treat. 2015; 47:197–207.
Article22. Dawood S, Broglio K, Ensor J, Hortobagyi GN, Giordano SH. Survival differences among women with de novo stage IV and relapsed breast cancer. Ann Oncol. 2010; 21:2169–74.
Article23. Thomas A, Khan SA, Chrischilles EA, Schroeder MC. Initial surgery and survival in stage IV breast cancer in the United States, 1988-2011. JAMA Surg. 2016; 151:424–31.
Article24. Joinpoint Regression Program, version 4.5.0.1 [Internet]. Bethesda, MD: Statistical Research and Applications Branch, National Cancer Institute;2017 [cited 2017 Jun 12]. Available from: https://surveillance.cancer.gov/joinpoint/download.25. Di Meglio A, Freedman RA, Lin NU, Barry WT, Metzger-Filho O, Keating NL, et al. Time trends in incidence rates and survival of newly diagnosed stage IV breast cancer by tumor histology: a population-based analysis. Breast Cancer Res Treat. 2016; 157:587–96.
Article26. Di Lascio S, Pagani O. Oligometastatic breast cancer: a shift from palliative to potentially curative treatment? Breast Care (Basel). 2014; 9:7–14.
Article27. Park S, Han W, Kim J, Kim MK, Lee E, Yoo TK, et al. Risk factors associated with distant metastasis and survival outcomes in breast cancer patients with locoregional recurrence. J Breast Cancer. 2015; 18:160–6.
Article28. Iasonos A, Schrag D, Raj GV, Panageas KS. How to build and interpret a nomogram for cancer prognosis. J Clin Oncol. 2008; 26:1364–70.
Article29. Hart CD, Migliaccio I, Malorni L, Guarducci C, Biganzoli L, Di Leo A. Challenges in the management of advanced, ER-positive, HER2-negative breast cancer. Nat Rev Clin Oncol. 2015; 12:541–52.
Article30. Wang X, Lin C, Zhao X, Liu A, Zhu J, Li X, et al. Acylglycerol kinase promotes cell proliferation and tumorigenicity in breast cancer via suppression of the FOXO1 transcription factor. Mol Cancer. 2014; 13:106.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Novel Prognostic Nomogram for Predicting Risks of Distant Failure in Patients with Invasive Breast Cancer Following Postoperative Adjuvant Radiotherapy
- Establishment and Validation of a Nomogram for Nasopharyngeal Carcinoma Patients Concerning the Prognostic Effect of Parotid Lymph Node Metastases
- Development and validation of a prognostic model based on metabolic risk score to predict overall survival of endometrial cancer in Chinese patients
- Validation of Traditional Prognosis Scoring Systems and Skeletal Oncology Research Group Nomogram for Predicting Survival of Spinal Metastasis Patients Undergoing Surgery
- Nomogram of Naive Bayesian Model for Recurrence Prediction of Breast Cancer