Neurointervention.
2018 Mar;13(1):32-40. 10.5469/neuroint.2018.13.1.32.
Treatment of Intracranial Aneurysms with the Pipeline Embolization Device Only: a Single Center Experience
- Affiliations
-
- 1Department of Diagnostic and Interventional Neuroradiology, University Hospital Cologne, Cologne, Germany. volker.maus@uk-koeln.de
- 2Department of Neuroradiology, Charité, Berlin, Germany.
- 3Department of Neuroradiology, University Hospital Munich (LMU), Munich, Germany.
- 4Department of Neurosurgery, University Hospital Cologne, Cologne, Germany.
- KMID: 2424047
- DOI: http://doi.org/10.5469/neuroint.2018.13.1.32
Abstract
- PURPOSE
The aim of this study was to evaluate the technical feasibility and rate of mid-term occlusion in aneurysms treated solely with the Pipeline Embolization Device (PED) in a German tertiary care university hospital.
MATERIALS AND METHODS
Forty-nine non-consecutive intracranial aneurysms underwent endovascular treatment using the PED exclusively between March 2011 and May 2017 at our institution. Primary endpoint was a favorable aneurysm occlusion defined as OKM C1-3 and D (O'Kelly Marotta Scale). Secondary endpoints were retreatment rate and delayed complications. Median follow-up was 200 days.
RESULTS
The mean aneurysm size was 7.1 ± 5.3 mm. Forty-four aneurysms were located in the anterior circulation (90%). Ten aneurysms were ruptured (20%). Branching vessels from the sac were observed in 11 aneurysms (22%). Favorable obliteration immediately after PED placement was seen in 13/49 aneurysms (27%), of those nine aneurysms were completely occluded (18%). Angiographic and clinical follow-up was available for 45 cases (92%); 36/45 aneurysms (80%) were occluded completely and 40/45 aneurysms (89%) showed a favorable occlusion result. A branching vessel arising from the aneurysm sac was associated with incomplete occlusion (P < .05). All electively treated patients had good outcome (mRS 0). Three aneurysms (6%) required additional treatment due to aneurysm recurrence.
CONCLUSION
In our series, treatment of intracranial aneurysms with the PED was associated with favorable occlusion rates and low complication rates at mid-term follow-up. The presence of branching vessels arising from the aneurysms sac was predictive for an incomplete occlusion.
MeSH Terms
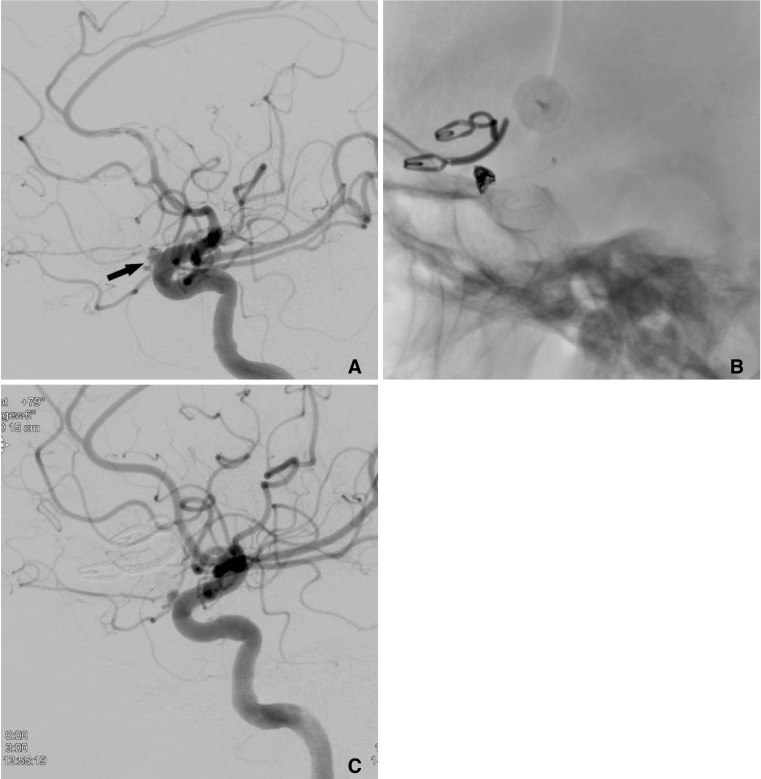
Figure
Reference
-
1. Guglielmi G, Vinuela F, Sepetka I, Macellari V. Electrothrombosis of saccular aneurysms via endovascular approach. Part 1: Electrochemical basis, technique, and experimental results. J Neurosurg. 1991; 75:1–7. PMID: 2045891.2. Naggara ON, Lecler A, Oppenheim C, Meder JF, Raymond J. Endovascular treatment of intracranial unruptured aneurysms: a systematic review of the literature on safety with emphasis on subgroup analyses. Radiology. 2012; 263:828–835. PMID: 22623696.
Article3. Brinjikji W, Murad MH, Lanzino G, Cloft HJ, Kallmes DF. Endovascular treatment of intracranial aneurysms with flow diverters: a meta-analysis. Stroke. 2013; 44:442–447. PMID: 23321438.
Article4. Jabbour P, Chalouhi N, Tjoumakaris S, Gonzalez LF, Dumont AS, Randazzo C, et al. The Pipeline Embolization Device: learning curve and predictors of complications and aneurysm obliteration. Neurosurgery. 2013; 73:113–120. PMID: 23615106.5. Pierot L, Wakhloo AK. Endovascular treatment of intracranial aneurysms: current status. Stroke. 2013; 44:2046–2054. PMID: 23798560.6. Becske T, Kallmes DF, Saatci I, McDougall CG, Szikora I, Lanzino G, et al. Pipeline for uncoilable or failed aneurysms: results from a multicenter clinical trial. Radiology. 2013; 267:858–868. PMID: 23418004.
Article7. Chalouhi N, Starke RM, Yang S, Bovenzi CD, Tjoumakaris S, Hasan D, et al. Extending the indications of flow diversion to small, unruptured, saccular aneurysms of the anterior circulation. Stroke. 2014; 45:54–58. PMID: 24253543.
Article8. Kan P, Siddiqui AH, Veznedaroglu E, Liebman KM, Binning MJ, Dumont TM, et al. Early postmarket results after treatment of intracranial aneurysms with the pipeline embolization device: a U.S. multicenter experience. Neurosurgery. 2012; 71:1080–1087. PMID: 22948199.9. Nelson PK, Lylyk P, Szikora I, Wetzel SG, Wanke I, Fiorella D. The pipeline embolization device for the intracranial treatment of aneurysms trial. AJNR Am J Neuroradiol. 2011; 32:34–40. PMID: 21148256.
Article10. McAuliffe W, Wycoco V, Rice H, Phatouros C, Singh TJ, Wenderoth J. Immediate and midterm results following treatment of unruptured intracranial aneurysms with the pipeline embolization device. AJNR Am J Neuroradiol. 2012; 33:164–170. PMID: 21979492.
Article11. Saatci I, Yavuz K, Ozer C, Geyik S, Cekirge HS. Treatment of intracranial aneurysms using the pipeline flow-diverter embolization device: a single-center experience with long-term follow-up results. AJNR Am J Neuroradiol. 2012; 33:1436–1446. PMID: 22821921.
Article12. Murthy SB, Shah J, Mangat HS. Treatment of Intracranial Aneurysms With Pipeline Embolization Device: Newer Applications and Technical Advances. Curr Treat Options Neurol. 2016; 18:16. PMID: 26923606.
Article13. Szikora I, Berentei Z, Kulcsar Z, Marosfoi M, Vajda ZS, Lee W, et al. Treatment of intracranial aneurysms by functional reconstruction of the parent artery: the Budapest experience with the pipeline embolization device. AJNR Am J Neuroradiol. 2010; 31:1139–1147. PMID: 20150304.
Article14. Amenta PS, Dalyai RT, Kung D, Toporowski A, Chandela S, Hasan D, et al. Stent-assisted coiling of wide-necked aneurysms in the setting of acute subarachnoid hemorrhage: experience in 65 patients. Neurosurgery. 2012; 70:1415–1429. PMID: 22186840.15. Kabbasch C, Mpotsaris A, Behme D, Dorn F, Stavrinou P. Pipeline Embolization Device for Treatment of Intracranial Aneurysms-The More, the Better? A Single-center Retrospective Observational Study. J Vasc Interv Neurol. 2016; 9:14–20. PMID: 27829966.16. Maus V, Mpotsaris A, Dorn F, Mohlenbruch M, Borggrefe J, Stavrinou P, et al. The Use of Flow-Diverter in Ruptured, Dissecting Intracranial Aneurysms of the Posterior Circulation. World Neurosurg. 2017; 12. 23. S1878-8750(17)32211-8. DOI: 10.1016/J.wneu.2017.12.095. [Epub ahead of printing].17. O'Kelly C J, Krings T, Fiorella D. A novel grading scale for the angiographic assessment of intracranial aneurysms treated using flow diverting stents. Interv Neuroradiol. 2010; 16:133–137. PMID: 20642887.18. Shapiro M, Raz E, Becske T, Nelson PK. Building multidevice pipeline constructs of favorable metal coverage: a practical guide. AJNR Am J Neuroradiol. 2014; 35:1556–1561. PMID: 24676003.
Article19. Lopes D. Histological postmortem study of an internal carotid artery aneurysm treated with the Neuroform stent. Neurosurgery. 2005; 56:E416. PMID: 15670395.
Article20. Krishna C, Sonig A, Natarajan SK, Siddiqui AH. The expanding realm of endovascular neurosurgery: flow diversion for cerebral aneurysm management. Methodist Debakey Cardiovasc J. 2014; 10:214–219. PMID: 25624975.21. Kallmes DF, Hanel R, Lopes D, Boccardi E, Bonafe A, Cekirge S, et al. International retrospective study of the pipeline embolization device: a multicenter aneurysm treatment study. AJNR Am J Neuroradiol. 2015; 36:108–115. PMID: 25355814.
Article22. O'Kelly CJ, Spears J, Chow M, Wong J, Boulton M, Weill A, et al. Canadian experience with the pipeline embolization device for repair of unruptured intracranial aneurysms. AJNR Am J Neuroradiol. 2013; 34:381–387. PMID: 22859284.23. Murthy SB, Shah S, Venkatasubba Rao CP, Bershad EM, Suarez JI. Treatment of unruptured intracranial aneurysms with the pipeline embolization device. J Clin Neurosci. 2014; 21:6–11. PMID: 24055205.
Article24. Yu SC, Kwok CK, Cheng PW, Chan KY, Lau SS, Lui WM, et al. Intracranial aneurysms: midterm outcome of pipeline embolization device--a prospective study in 143 patients with 178 aneurysms. Radiology. 2012; 265:893–901. PMID: 22996749.
Article25. Chiu AH, Cheung AK, Wenderoth JD, De Villiers L, Rice H, Phatouros CC, et al. Long-Term Follow-Up Results following Elective Treatment of Unruptured Intracranial Aneurysms with the Pipeline Embolization Device. AJNR Am J Neuroradiol. 2015; 36:1728–1734. PMID: 25999412.
Article26. Chalouhi N, Tjoumakaris S, Phillips JL, Starke RM, Hasan D, Wu C, et al. A single pipeline embolization device is sufficient for treatment of intracranial aneurysms. AJNR Am J Neuroradiol. 2014; 35:1562–1566. PMID: 24788125.
Article27. Lin N, Brouillard AM, Keigher KM, Lopes DK, Binning MJ, Liebman KM, et al. Utilization of Pipeline embolization device for treatment of ruptured intracranial aneurysms: US multicenter experience. J Neurointerv Surg. 2015; 7:808–815. PMID: 25230839.
Article28. Chalouhi N, Zanaty M, Whiting A, Tjoumakaris S, Hasan D, Ajiboye N, et al. Treatment of ruptured intracranial aneurysms with the pipeline embolization device. Neurosurgery. 2015; 76:165–172. PMID: 25549187.
Article29. Brinjikji W, Piano M, Fang S, Pero G, Kallmes DF, Quilici L, et al. Treatment of ruptured complex and large/giant ruptured cerebral aneurysms by acute coiling followed by staged flow diversion. J Neurosurg. 2016; 125:120–127. PMID: 26654182.
Article30. Mut F, Lohner R, Chien A, Tateshima S, Viñnuela F, Putman C, et al. Computational Hemodynamics Framework for the Analysis of Cerebral Aneurysms. Int J Numer Method Biomed Eng. 2011; 27:822–839. PMID: 21643491.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Flow diverter stenting for intracranial aneurysms in the pediatric population: Two case reports and literature review
- A Case of Migration of Pipeline Embolization Device Causing Rupture during Treatment of an Unruptured Vertebral Artery Dissecting Aneurysm
- Pipeline Embolization Device for Giant Internal Carotid Artery Aneurysms: 9-Month Follow-Up Results of Two Cases
- Persistent Aneurysm Growth Following Pipeline Embolization Device Assisted Coiling of a Fusiform Vertebral Artery Aneurysm: A Word of Caution!
- Clinical Experience of Thromboembolic Complications of Coil Embolization for Intracranial Aneurysms with Literature Review