Prog Med Phys.
2018 Sep;29(3):81-91. 10.14316/pmp.2018.29.3.81.
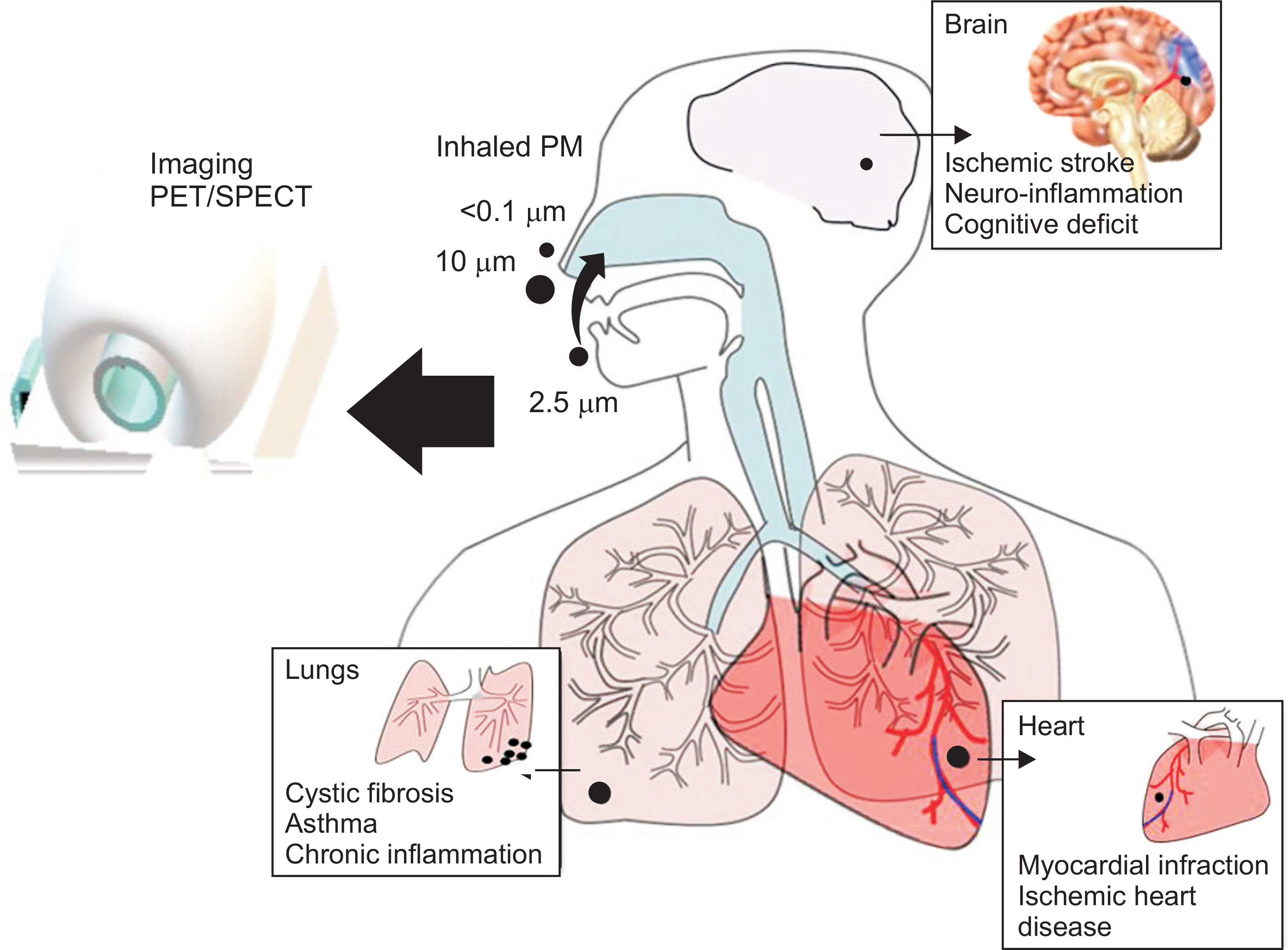
Effect of Particulate Matter on Human Health, Prevention, and Imaging Using PET or SPECT
- Affiliations
-
- 1Division of RI Application, Korea Institute of Radiological and Medical Sciences (KIRAMS), Seoul, Korea. kjs@kirams.re.kr
- 2Radiological and Medico-Oncological Sciences, University of Science and Technology (UST), Seoul, Korea.
- 3Advanced Radiation Technology Institute, Korea Atomic Energy Research Institute (KAERI), Jeongeup, Korea.
- 4Radiation Biotechnology and Applied Radioisotope Science, University of Science and Technology (UST), Daejeon, Korea.
- 5Center for Environment, Health and Welfare Research, Korea Institute of Science and Technology (KIST), Seoul, Korea.
- KMID: 2421704
- DOI: http://doi.org/10.14316/pmp.2018.29.3.81
Abstract
- Particulate matter (PM) in dust causes serious pathological conditions, and it has been considered a critical health issue for many years. Respiratory disorders such as bronchitis, asthma, and chronic inflammation, are the most common illnesses due to PM that appears as dust. There is evidence that cardiovascular and neurological abnormalities are caused by PM. Although an extensive amount of work has been conducted on this topic, including studies on the nature of the particles, particle size measurements, particle distribution upon inhalation, the health effects of fine particles, disease prevention, diagnosis, and treatment, to this date, there is still a considerable lack of knowledge in these areas. Therefore, the identification of the key components that cause diseases owing to PM, and the specific diagnoses of the diseases, is important. This review will explore the current literature on the origin and nature of PM and their effects on human health. In addition, it will also highlight the approaches that have been adopted in order to diagnose the effects of PM using positron emission tomography (PET) or single-photon emission computerized tomography (SPECT).
Keyword
MeSH Terms
Figure
Reference
-
1.Kang D., Kim JE. Fine, ultrafine, and yellow dust: emerging health problems in Korea. J Korean Med Sci. 2014. 29:621–622.
Article2.Shepherd M. NARSTO report Ch 1.Perspective for mang-ing PM. US, Mexico, Canada. NARSTO 2004.53–68.3.Jemmett-Smith BC., Marsham JH., Knippertz P., Gilkeson CA. Quantifying global dust devil occurrence from meteorological analyses. Geophys Res Lett. 2015. 42:1275–1282.4.Wang X., Cheng H., Che H, et al. Modern dust aerosol availability in northwestern China. Sci Rep. 2017. 7:8741.
Article5.Kandler K., Benker N., Bundke U. Chemical composition and complex refractive index of saharan mineral dust at Izaña, Tenerife (Spain) derived by electron microscopy. Atmospheric Environ. 2007. 41:8058–8074.
Article6.Maxwel-Meier K., Weber R., Song C., Orsini ., Ma Y. Inorganic composition of fine particles in mixed mineral dust-pollution plumes observed from airborne measurements during ACE-Asia. J Geophys Res: Atmospheres. 2004. 109:D19S07.
Article7.Farfel MR., Orlova AO., Lees PSJ., Rohde C., Ashley PJ., Chi-solm JJ. A study of urban housing demolitions as sources of lead in ambient dust: demolition practices and exterior dust fall. Environmental Health Perspectives. 2003. 111:1228–1234.
Article8.Bućko MS., Magiera T., Johanson B., Petrovský E., Pesonen LJ. Identification of magnetic particulates in road dust accumulated on roadside snow using magnetic, geochemical and micro-morphological analyses. Environ Pollut. 2011. 159:1266–1276.
Article9.Takada H., Onda T., Harada M., Ogura N. Distribution and sources of polycyclic aromatic hydrocarbons (PAHs) in street dust from the Tokyo metropolitan area. Sci Total Environ. 1991. 107:45–69.
Article10.Sofilic T., Rastovcan-Mioc A., Cerjan-Stefanovic S., Novosel-Radovic V., Jenko M. Characterization of steel mill electric-arc furnace dust. J Hazard Mater. 2004. 109:59–70.11.Wheatley AD., Sadhra S. Occupational exposure to diesel exhaust fumes. Ann Occup Hyg. 2004. 148:369–376.12.Snider G., Weagle C., L MurdymootooK, et al. Variation in global chemical composition of PM2.5: emerging results from SPARTAN.Atmos. Chem. Phys. 2016. 16:9629–9653.13.Chen W., Liu Y., Wang H., Hnizdo E, et al. Long-term exposure to silica dust and risk of total and cause-specific mortality in Chinese workers: a cohort study. PLoS Med. 2012. 9(4):e1001206.
Article14.Jeong SH., Jeong HE., Byong KS, et al. Comparison of air pollution and the prevalence of allergy-related diseases in Incheon and Jeju City. Korean J Pediatrics. 2011. 54:501–506.
Article15.Laney AS., Petsonk EL., Hale JM., Wolfe AL., Attfield MD. Potential determinants of coal worker's pneumoconiosis, advanced pneumoconiosis, and progressive massive fibrosis among underground coal miners in the United States, 2005-2009. Am J Public Health. 2012. 102(Suppl 2):S279–283.
Article16.Mamuya SH., Moen B., Bratveit M. Quartz exposure and increased respiratory symptoms among coal mine workers in Tanzania. East Afr J Public Health. 2011. 8:190–195.17.Moreno T., Kojima T., Querol X, et al. Natural versus anthropogenic inhalable aerosol chemistry of transbound-ary East Asian atmospheric outflows into western Japan. Scie Total Environ. 2012. 424:182–192.
Article18.Neghab M., Mohraz MH., Hassanzadeh J. Symptoms of respiratory disease and lung functional impairment associated with occupational inhalation exposure to carbon black dust. J Occup Health. 2011. 53:432–438.
Article19.Sahle W., Krantz S., Christensson B., Laszlo I. Preliminary data on hard metal workers exposure to tungsten oxide fibres. Sci Total Environ. 1996. 191:153–167.
Article20.Bharadwaj P., Burney J. Cognition impact of sand and dust storms highlights future research needs? Lancet. Planet Health. 2018. 2(5):); e196-e197.
Article21.Wu JZ., Dan-Dan G., Lin-fu Z., Ling Y., Ying Z., Qi Yuan L. Effects of particulate matter on allergic respiratory diseases. Chronic Dis Transl Med. 2018. 4:95–102.
Article22.Chen B., Kan H. Air pollution and population health: a global challenge. Environ Health Preventive Med. 2008. 13:94–101.
Article23.Kolpakova AF., Sharipov RN., Kolpakov FA. Air pollution by particulate matter as the risk factor for the cardiovascular diseases. Gigiena i Sanitariia. 2017. 96:133–137.
Article24.Tsai S-S., Goggins WB., Chiu HF., Yang C-Y. Evidence for an association between air pollution and daily stroke admissions in Kaohsiung, Taiwan. Stroke. 2003. 34:2612–2616.
Article25.Pinault LL., Weichenthal S., Crouse DL, et al. Associations between fine particulate matter and mortality in the 2001 Canadian Census Health and Environment Cohort. Environ Res. 2017. 159:406–415.
Article26.Nemery B., Hoet PHM., Nemmar A. The Meuse valley fog of 1930: an air pollution disaster. Lancet. 2001. 357:704–708.
Article27.Logan WPD. Mortality in the London fog incident, 1952. Lancet. 1953. 261:336–338.
Article28.Brook RD., Franklin B., Cascio W, et al. Air pollution and cardiovascular disease. A statement for healthcare professionals from the expert panel on population and prevention science of the American Heart Association. Circ. 2004. 109:2655–2671.
Article29.Milojevic A., Paul W., Ben A, et al. Short-term effects of air pollution on a range of cardiovascular events in England and Wales: case-crossover analysis of the MINAP database, hospital admissions and mortality. Heart. 2014. 100:1093–1098.
Article30.Middleton N., Panayiotis Y., Savvas K, et al. A 10-year time-series analysis of respiratory and cardiovascular morbidity in Nicosia, Cyprus: the effect of short-term changes in air pollution and dust storms. Environ Health. 2008. 7:39.
Article31.Pope IC., Burnett RT., Thun MJ, et al. Lung cancer, cardiopulmonary mortality, and long-term exposure to fine particulate air pollution. JAMA. 2002. 287:1132–1141.32.Urch B., Frances S., Paul S, et al. Acute blood pressure responses in healthy adults during controlled air pollution exposures. Environ Health Perspectives. 2005. 113:1052–1055.
Article33.Brook RD., Brooke JR., Urch B, et al. Inhalation of fine particulate air pollution and ozone causes acute arterial vasoconstriction in healthy adults. Circ. 2002. 105:1534–1536.
Article34.Peters A., Stephenie VK., Margit H, et al. Exposure to traffic and the onset of myocardial infarction. New England J Med. 2004. 351:1721–1730.
Article35.Ueda K., Shimizu A., Nitta H., Inoue K. Long-range transported Asian dust and emergency ambulance dispatches. Inhalation Toxicol. 2012. 24:858–867.
Article36.Lee J-T., Kim H., Cho YS, et al. Air pollution and hospital admissions for ischemic heart diseases among individuals 64+ years of age residing in Seoul, Korea. Arch Environ Health: Int J. 2003. 58:617–623.
Article37.Tam WWS., Wong TW., Wong AHS. Effect of dust storm events on daily emergency admissions for cardiovascular diseases. Circ. 2012. 76:655–660.
Article38.Mueller-Anneling LJ., O'Neill ME., Thorne PS. Biomonitor-ing for assessment of organic dust-induced lung inflammation. Eur Resp J. 2006. 27:1096–1102.
Article39.Kang J-H., Keller JJ., Chen C-S., Lin H-C. Asian dust storm events are associated with an acute increase in pneumonia hospitalization. Ann Epidemiol. 2012. 22:257–263.
Article40.Burnett RT., Smith-Doiron M., Stieb D., Cakmak S., Brook JR. Effects of particulate and gaseous air pollution on cardiorespiratory hospitalizations. Arch Environ Health: Int J. 1999. 54:130–139.
Article41.Schwartz J. PM10 ozone, and hospital admissions for the elderly in Minneapolis-St. Paul, Minnesota. Arch Environ Health: Int J. 1994. 49:366–374.42.Fusco D., Forestiere F., Michelozzi P, et al. Air pollution and hospital admissions for respiratory conditions in Rome, Italy. Eur Resp J. 2001. 17:1143–1150.
Article43.Wagner GR. Asbestosis and silicosis. Lancet. 1997. 349:1311–1315.
Article44.Middleton EL. Industrial pulmonary disease due to the inhalation of dust with special reference to silieosis. Lancet. 1936. 139:59–64.45.Bhattacharjee P., Paul S., Bhattacharjee P. Risk of occupational exposure to asbestos, silicon and arsenic on pulmonary disorders: understanding the genetic-epigenetic interplay and future prospects. Environ Res. 2016. 147:425–434.
Article46.Michel O., Kipps J., Duchateau J, et al. Severity of asthma is related to endotoxin in house dust. Am J Resp. Crit Care Med. 1996. 154:1641–1646.47.Lin M-T., Chew TK., Chun C-C, et al. Association of meteorological factors and air NO2 and O3 concentrations with acute exacerbation of elderly chronic obstructive pulmonary disease. Sci Rep. 2018. 8:10192.
Article48.Tiwari RR., Sharma YK., Saiyed HN. Tuberculosis among workers exposed to free silica dust. Indian J Occup and Environ Med. 2007. 11:61–64.
Article49.Middleton NJ. Desert dust hazards: A global review. Aeolian Res. 2017. 24:53–63.
Article50.Zhang ZF., Yu SZ., Zhou GD. Indoor air pollution of coal fumes as a risk factor of stroke. Shanghai. Am J Public Health. 1988. 78:975–977.51.Block ML. Calderón-Garcidueñas. Air pollution: mechanisms of neuroinflammation and CNS disease. Trends in Neurosci. 2009. 32:506–516.
Article52.Calderón-Garcidueñas L., Mora-Tiscareño A., Ontiveros E, et al. Air pollution, cognitive deficits and brain abnormalities: A pilot study with children and dogs. Brain and Cog-nit. 2008. 68:117–127.
Article53.Lee KK., Miller MR., Shah ASV. Air pollution and stroke. J Stroke. 2018. 20:2–11.
Article54.Yang C-Y., Chen Y-S., Chiu H-F., Goggins W. Effects of Asian dust storm events on daily stroke admissions in Taipei, Taiwan. Environ Res. 2005. 99(1):79–84.
Article55.Kang JH., Liu TC., Keller J., Lin HC. Asian dust storm events are associated with an acute increase in stroke hospitalisation. J Epidemiol Commun Health. 2013. 67:125–131.
Article56.Scheuch G., Bennett W., Borgström L, et al. Deposition, imaging, and clearance: what remains to be done? J Aerosol-Med Pulm Drug Deliv. 2010. 23(Suppl 2):S39–57.
Article57.Laube BL., Jashnani R., Dalby RN., Zeitlin PL. Targeting aerosol deposition in patients with cystic fibrosis. Chest. 2000. 118:1069–1076.
Article58.EC Pratt, TM Shaffer, J Grimm. Nanoparticles and radiotracers: advances towards radionanomedicine. Wiley Interdisciplinary Reviews: Nanomedicine and Nanobio-technology. 2016. 8:872–890.59.Nemmar AD., Hoest PHM, et al. Passage of inhaled particle into the blood circulation in humans. Circ. 2002. 105:1411–414.60.Berridge M.S.., Lee Z.., Heald D.L. Pulmonary distribution and kinetics of inhaled 11C-tiamcinolone acetonide. J Nucl Med. 2000. 41:1603–1611.61.Visser TJ., Van WA,Doze P, et al. Characterisation of β2-adrenoceptors, using the agonist 11C-formoterol and positron emission tomography. Eur J Pharmacol. 1998. 361:35–41.62.Guenther KJ., Yoganathan S., Garofalo R, et al. Synthesis and in vitro evaluation of 18F- and 19F-labeled insulin: A new radiotracer for PET-based molecular imaging studies. J Med Chem. 2006. 49:1466–1474.63.Iozzo P., Osman S., Glaser M, et al. In vivo imaging of insulin receptors by PET: preclinical evaluation of 125I and 124I labelled human insulin. Nuc Med Biol. 2002. 29:73–82.64.Dolovich MB. 18F-FDG positron emission tomographic imaging of pulmonary functions, pathology, and drug delivery. Proc Am Thorac Soc. 2009. 6:477–485.65.Tarkin JM., Joshi FR., Rudd JH. PET imaging of inflammation in atherosclerosis. 2014. 11:443–57.66.Capitanio S., Nordin AJ., Noraini AR., Rossetti C. PET/CT in nononcological lung diseases: current applications and future perspectives. Eur Resp Rev. 2016. 25:247–258.
Article67.Dusad A., Geoffrey MT., Lynell WK, et al. Vitamin D supplementation protects against bone loss following inhalant organic dust and lipopolysaccharide exposures in mice. Immunol Res. 2015. 62:46–59.
Article68.Nordgren TM., Friemel TD., Heires AJ, et al. The omega-3 fatty acid docosahexaenoic acid attenuates organic dust-induced airway inflammation. Nutrients. 2014. 6:5434–54.
Article69.Shim H.E.., Lee J.Y.., Lee C.H., et al. Quantification of inhaled aerosol particles composed of toxic house hold disinfectant using radioanalytical method. Chemophere. 2018. 207:649–654.70.Baldacci S., Maio S., Cerrai S, et al. Allergy and asthma: Effects of the exposure to particulate matter and biological allergens. Resp Med. 2015. 109:1089–1104.
Article71.Jalbert I., Golebiowski B. Environmental aeroallergens and allergic rhino-conjunctivitis. Curr Opin Allergy Clin Im-munol. 2015. 15:476–481.
Article72.Tian Y., Xiao X., Yiqun W, et al. Fine particulate air pollution and first hospital admissions for ischemic stroke in Beijing, China. Sci Rep. 2017. 7(1):3897.
Article73.Akbarzadeh MA., Khaheshi I., Sharifi A, et al. The association between exposure to air pollutants including PM10, PM2.5, ozone, carbon monoxide, sulfur dioxide, and nitrogen dioxide concentration and the relativerisk of developingSTEMI: A case-crossover design. Environ Res. 2018. 161:299–303.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Association of Particulate Matter With ENT Diseases
- Publication trends in research on particulate matter and health impact over a 10-year period: 2009–2018
- The Relationships between Particulate Matter Risk Perception, Knowledge, and Health Promoting Behaviors among College Students
- Premature Deaths Attributable to Exposure to Ambient Fine Particulate Matter in the Republic of Korea: Implication for Future Environmental Health
- Health effects of particulate matter