J Korean Med Assoc.
2018 Dec;61(12):749-755. 10.5124/jkma.2018.61.12.749.
Health effects of particulate matter
- Affiliations
-
- 1Department of Preventive Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 2Department of Preventive Medicine, College of Medicine, Seoul National University, Seoul, Korea. ychong1@snu.ac.kr
- KMID: 2429339
- DOI: http://doi.org/10.5124/jkma.2018.61.12.749
Abstract
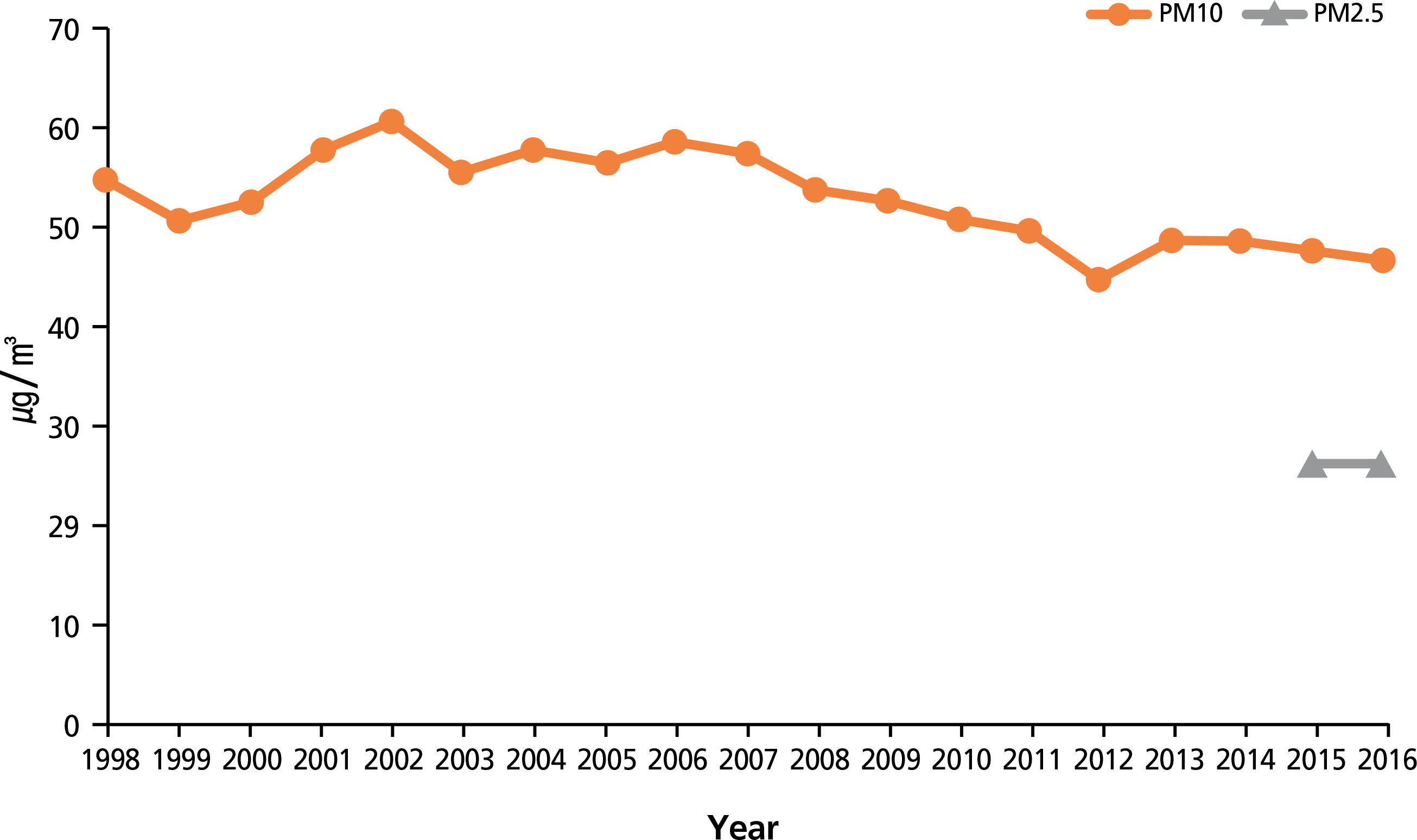
- Particulate matter is an air pollutant emitted from both natural and anthropogenic sources, and its adverse health effects have been well documented in time-series analyses and cohort studies. The effect size of particulate matter exposure"”a roughly 0.5% increase in mortality for each 10 µg/m³ increment of short-term exposure to particulate matter with aerodynamic diameter ≤10 µm and approximately a 10% increase for each 10 µg/m³ increment of long-term exposure to particulate matter with aerodynamic diameter ≤2.5 µm"”is small compared to other risk factors, but the exposure is involuntary and affects the entire population, which makes particulate matter pollution an important public health issue. The World Health Organization and Korean government have both established guidelines for particulate matter concentrations, but the Korean guideline is less stringent than that of the World Health Organization. The annual mean concentration of particulate matter in Korea is decreasing, but the trend seems to be slowing. In addition to policy efforts to reduce particulate matter emission, personal approaches such as the use of face masks and air purifiers have been recommended. Personal approaches may not solve the fundamental problem, but can provide temporary mitigation until efforts to reduce emission make progress.
MeSH Terms
Figure
Reference
-
1. Ryou HG, Heo J, Kim SY. Source apportionment of PM(10) and PM(2.5) air pollution, and possible impacts of study characteristics in South Korea. Environ Pollut. 2018; 240:963–972.
Article2. Miller FJ, Gardner DE, Graham JA, Lee RE Jr, Wilson WE, Bachmann JD. Miller FJ, Gardner DE, Graham JA, Lee RE, Wilson WE, Bachmann JD. Size considerations for establishing a standard for inhalable particles. J Air Pollut Control Assoc. 1979; 29:610–615.3. National Institute of Environmental Research. Annual report of air quality in Korea 2016. Incheon: National Institute of Environmental Research;2017.4. Korea Environmental Corporation. Air Korea [Internet]. Incheon: Korea Environmental Corporation [cited 2018 Nov 30]. Available from:. https://www.airkorea.or.kr/index.5. World Health Organization. Air quality guidelines: global update 2005 [Internet]. Geneva: World Health Organization;2006. [cited 2018 Nov 30]. Available from:. https://www.who.int/phe/health_topics/outdoorair/outdoorair_aqg/en/.6. Loney T, Nagelkerke NJ. The individualistic fallacy, ecological studies and instrumental variables: a causal interpretation. Emerg Themes Epidemiol. 2014; 11:18.
Article7. Pope CA 3rd, Schwartz J, Ransom MR. Daily mortality and PM10 pollution in Utah Valley. Arch Environ Health. 1992; 47:211–217.
Article8. Dockery DW, Schwartz J, Spengler JD. Air pollution and daily mortality: associations with particulates and acid aerosols. Environ Res. 1992; 59:362–373.
Article9. Kim SE, Honda Y, Hashizume M, Kan H, Lim YH, Lee H, Kim CT, Yi SM, Kim H. Seasonal analysis of the short-term effects of air pollution on daily mortality in Northeast Asia. Sci Total Environ. 2017; 576:850–857.
Article10. Park HY, Bae S, Hong YC. PM(10) exposure and non-accidental mortality in Asian populations: a metaanalysis of time-series and case-crossover studies. J Prev Med Public Health. 2013; 46:10–18.
Article11. Dockery DW, Pope CA 3rd, Xu X, Spengler JD, Ware JH, Fay ME, Ferris BG Jr, Speizer FE. An association between air pollution and mortality in six U.S. cities. N Engl J Med. 1993; 329:1753–1759.12. Di Q, Wang Y, Zanobetti A, Wang Y, Koutrakis P, Choirat C, Dominici F, Schwartz JD. Air pollution and mortality in the medicare population. N Engl J Med. 2017; 376:2513–2522.
Article13. Han C, Kim S, Lim YH, Bae HJ, Hong YC. Spatial and temporal trends of number of deaths attributable to ambient PM(2.5) in the Korea. J Korean Med Sci. 2018; 33:e193.
Article14. Kim JH, Oh IH, Park JH, Cheong HK. Premature deaths attributable to longterm exposure to ambient fine particulate matter in the Republic of Korea. J Korean Med Sci. 2018; 33:e251.
Article15. National Institute of Environmental Research. Standard methods for the examination of air pollution. Incheon: National Institute of Environmental Research;2017.16. Zou B, Wilson JG, Zhan FB, Zeng Y. Air pollution exposure assessment methods utilized in epidemiological studies. J Environ Monit. 2009; 11:475–490.
Article17. Jang AS. Impact of particulate matter on health. J Korean Med Assoc. 2014; 57:763–768.
Article18. Brook RD, Rajagopalan S, Pope CA 3rd, Brook JR, Bhatnagar A, Diez-Roux AV, Holguin F, Hong Y, Luepker RV, Mittleman MA, Peters A, Siscovick D, Smith SC Jr, Whitsel L, Kaufman JD. American Heart Association Council on Epidemiology and Prevention, Council on the Kidney in Cardiovascular Disease, and Council on Nutrition, Physical Activity and Metabolism. Particulate matter air pollution and cardiovascular disease: an update to the scientific statement from the American Heart Association. Circulation. 2010; 121:2331–2378.19. Doll R, Peto R, Boreham J, Sutherland I. Mortality in relation to smoking: 50 years' observations on male British doctors. BMJ. 2004; 328:1519.
Article20. Hamra GB, Guha N, Cohen A, Laden F, Raaschou-Nielsen O, Samet JM, Vineis P, Forastiere F, Saldiva P, Yorifuji T, Loomis D. Outdoor particulate matter exposure and lung cancer: a systematic review and metaanalysis. Environ Health Perspect. 2014; 122:906–911.
Article21. International Agency for Research on Cancer; World Health Organization. Outdoor air pollution [Internet]. Lyon: International Agency for Research on Cancer;2015. [cited 2018 Nov 30]. Available from:. http://www.indiaenvironmentportal.org.in/files/file/outdoor%20air%20pollution_0.pdf.22. Lamichhane DK, Kim HC, Choi CM, Shin MH, Shim YM, Leem JH, Ryu JS, Nam HS, Park SM. Lung cancer risk and residential exposure to air pollution: a Korean population-based case-control study. Yonsei Med J. 2017; 58:1111–1118.
Article23. Khreis H, Kelly C, Tate J, Parslow R, Lucas K, Nieuwenhuijsen M. Exposure to traffic-related air pollution and risk of development of childhood asthma: a systematic review and metaanalysis. Environ Int. 2017; 100:1–31.
Article24. Achilleos S, Kioumourtzoglou MA, Wu CD, Schwartz JD, Koutrakis P, Papatheodorou SI. Acute effects of fine particulate matter constituents on mortality: a systematic review and meta-regression analysis. Environ Int. 2017; 109:89–100.
Article25. Miller KA, Siscovick DS, Sheppard L, Shepherd K, Sullivan JH, Anderson GL, Kaufman JD. Longterm exposure to air pollution and incidence of cardiovascular events in women. N Engl J Med. 2007; 356:447–458.
Article26. Wang Y, Eliot MN, Wellenius GA. Short-term changes in ambient particulate matter and risk of stroke: a systematic review and metaanalysis. J Am Heart Assoc. 2014; 3:e000983.
Article27. Mustafic H, Jabre P, Caussin C, Murad MH, Escolano S, Tafflet M, Perier MC, Marijon E, Vernerey D, Empana JP, Jouven X. Main air pollutants and myocardial infarction: a systematic review and metaanalysis. JAMA. 2012; 307:713–721.28. Hong YC, Lee JT, Kim H, Ha EH, Schwartz J, Christiani DC. Effects of air pollutants on acute stroke mortality. Environ Health Perspect. 2002; 110:187–191.
Article29. Lim YH, Kim H, Kim JH, Bae S, Park HY, Hong YC. Air pollution and symptoms of depression in elderly adults. Environ Health Perspect. 2012; 120:1023–1028.
Article30. Kim KN, Lim YH, Bae HJ, Kim M, Jung K, Hong YC. Longterm fine particulate matter exposure and major depressive disorder in a community-based urban cohort. Environ Health Perspect. 2016; 124:1547–1553.
Article31. Kim C, Jung SH, Kang DR, Kim HC, Moon KT, Hur NW, Shin DC, Suh I. Ambient particulate matter as a risk factor for suicide. Am J Psychiatry. 2010; 167:1100–1107.
Article32. Cherrie JW, Apsley A, Cowie H, Steinle S, Mueller W, Lin C, Horwell CJ, Sleeuwenhoek A, Loh M. Effectiveness of face masks used to protect Beijing residents against particulate air pollution. Occup Environ Med. 2018; 75:446–452.
Article33. Langrish JP, Li X, Wang S, Lee MM, Barnes GD, Miller MR, Cassee FR, Boon NA, Donaldson K, Li J, Li L, Mills NL, Newby DE, Jiang L. Reducing personal exposure to particulate air pollution improves cardiovascular health in patients with coronary heart disease. Environ Health Perspect. 2012; 120:367–372.
Article34. Li H, Cai J, Chen R, Zhao Z, Ying Z, Wang L, Chen J, Hao K, Kinney PL, Chen H, Kan H. Particulate matter exposure and stress hormone levels: a randomized, double-blind, crossover trial of air purification. Circulation. 2017; 136:618–627.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Health Effects of Ambient Particulate Matter
- Publication trends in research on particulate matter and health impact over a 10-year period: 2009–2018
- Association of Particulate Matter With ENT Diseases
- Premature Deaths Attributable to Exposure to Ambient Fine Particulate Matter in the Republic of Korea: Implication for Future Environmental Health
- Fine Particulate Matter and Urology: Emphasis on the Lower Urinary Tract