J Vet Sci.
2018 Sep;19(5):608-619. 10.4142/jvs.2018.19.5.608.
Evaluation of renal injury caused by acute volume replacement with hydroxyethyl starch 130/0.4 or Ringer's lactate solution in pigs
- Affiliations
-
- 1Department of Veterinary Medicine, ICAAM Research Center, University of Évora, 7006-554 Évora, Portugal.
- 2Educational, Technologies and Health Study Center (CI&DETS), Polytechnic Institute of Viseu, 3504-510 Viseu, Portugal.
- 3Centre for the Research and Technology of Agro-Environmental and Biological Sciences (CITAB), University of Trás-os-Montes and Alto Douro, 5001-801 Vila Real, Portugal. anafaustino.faustino@sapo.pt
- 4REQUIMTE - Faculty of Pharmacy, University of Porto, 4099-002 Porto, Portugal.
- 5Department of Veterinary Medicine, University of Cambridge, Cambridge CB2 1TN, United Kingdom.
- KMID: 2420929
- DOI: http://doi.org/10.4142/jvs.2018.19.5.608
Abstract
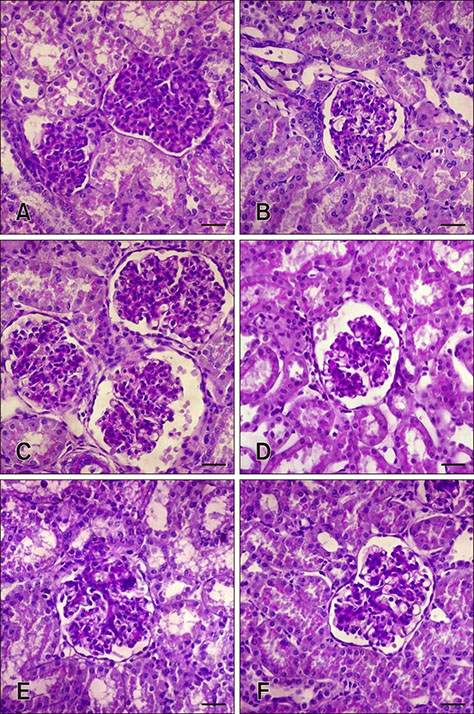
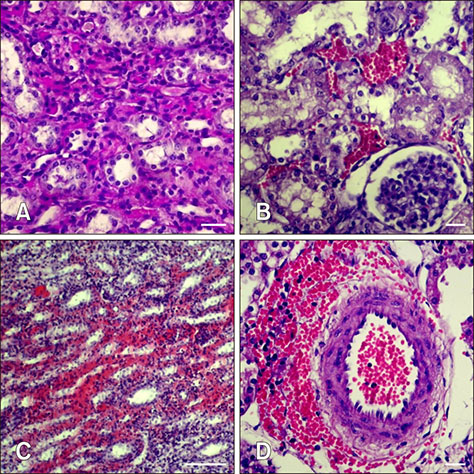
- This work aimed to evaluate the effects on renal tissue integrity after hydroxyethyl starch (HES) 130/0.4 and Ringer's lactate (RL) administration in pigs under general anesthesia after acute bleeding. A total of 30 mL/kg of blood were passively removed from the femoral artery in two groups of Large White pigs, under total intravenous anesthesia with propofol and remifentanil. After bleeding, Group 1 (n = 11) received RL solution (25 mL/kg) and Group 2 (n = 11) received HES 130/0.4 solution (20 mL/kg). Additionally, Group 3 (n = 6) was not submitted to bleeding or volume replacement. Pigs were euthanized and kidneys were processed for histopathological and immunohistochemical analyses. Minimal to moderate glomerular, tubular, and interstitial changes, as well as papillary necrosis, were observed in all experimental groups. Pre-apoptosis and apoptosis indicators were higher in pigs that received HES 130/0.4, indicating a higher renal insult. Both HES 130/0.4 and RL administration may cause renal injury, although renal injury may be more significant in pigs receiving HES 13/0.4. Results also suggest that total intravenous anesthesia with propofol and remifentanil may cause renal injury, and this effect can be dose related.
Keyword
MeSH Terms
Figure
Reference
-
1. Badr KF, Ichikawa I. Prerenal failure: a deleterious shift from renal compensation to decompensation. N Engl J Med. 1988; 319:623–629.
Article2. Basile DP, Anderson MD, Sutton TA. Pathophysiology of acute kidney injury. Compr Physiol. 2012; 2:1303–1353.
Article3. Bock C, Stachel CS. Development and validation of a confirmatory method for the determination of tranquilisers and a β-blocker in porcine and bovine kidney by LC-MS/MS. Food Addit Contam Part A Chem Anal Control Expo Risk Assess. 2013; 30:1000–1011.
Article4. Bonegio R, Lieberthal W. Role of apoptosis in the pathogenesis of acute renal failure. Curr Opin Nephrol Hypertens. 2002; 11:301–308.
Article5. Casserly B, O'Mahony E, Timm EG, Haqqie S, Eisele G, Urizar R. Propofol infusion syndrome: an unusual cause of renal failure. Am J Kidney Dis. 2004; 44:e98–e101.
Article6. Castro VJ, Astiz ME, Rackow EC. Effect of crystalloid and colloid solutions on blood rheology in sepsis. Shock. 1997; 8:104–107.
Article7. Cerkvenik-Flajs V. Determination of residues of azaperone in the kidneys by liquid chromatography with fluorescence detection. Anal Chim Acta. 2007; 586:374–382.
Article8. Cevatemre B, Ulukaya E, Sarimahmut M, Oral AY, Frame FM. The M30 assay does not detect apoptosis in epithelial-derived cancer cells expressing low levels of cytokeratin 18. Tumour Biol. 2015; 36:6857–6865.
Article9. de Azevedo VLF, Santos PSS, de Oliveira GS Jr, Módolo GP, Domingues MAC, Castiglia YMM, Vianna PTG, Vane LA, Módolo NSP. The effect of 6% Hydroxyethyl starch vs. Ringer's lactate on acute kidney injury after renal ischemia in rats. Acta Cir Bras. 2013; 28:5–9.10. Demir A, Yılmaz FM, Ceylan C, Doluoglu OG, Uçar P, Züngün C, Guclu CY, Ünal U, Karadeniz U, Günertem E, Lafci G, Çağlı K, Özgök A. A comparison of the effects of ketamine and remifentanil on renal functions in coronary artery bypass graft surgery. Ren Fail. 2015; 37:819–826.
Article11. Ebcioglu Z, Cohen DJ, Crew RJ, Hardy MA, Ratner LE, D'Agati VD, Markowitz GS. Osmotic nephrosis in a renal transplant recipient. Kidney Int. 2006; 70:1873–1876.
Article12. Ertmer C, Köhler G, Rehberg S, Morelli A, Lange M, Ellger B, Pinto BB, Rübig E, Erren M, Fischer LG, Van Aken H, Westphal M. Renal effects of saline-based 10% pentastarch versus 6% tetrastarch infusion in ovine endotoxemic shock. Anesthesiology. 2010; 112:936–947.
Article13. Flemming B, Seeliger E, Wronski T, Steer K, Arenz N, Persson PB. Oxygen and renal hemodynamics in the conscious rat. J Am Soc Nephrol. 2000; 11:18–24.
Article14. Hammond KL, Margolin DA. Surgical hemorrhage, damage control, and the abdominal compartment syndrome. Clin Colon Rectal Surg. 2006; 19:188–194.
Article15. Havasi A, Borkan SC. Apoptosis and acute kidney injury. Kidney Int. 2011; 80:29–40.
Article16. Hughes J, Gobe G. Identification and quantification of apoptosis in the kidney using morphology, biochemical and molecular markers. Nephrology (Carlton). 2007; 12:452–458.
Article17. Hussmann B, Lendemans S, de Groot H, Rohrig R. Volume replacement with Ringer-lactate is detrimental in severe hemorrhagic shock but protective in moderate hemorrhagic shock: studies in a rat model. Crit Care. 2014; 18:R5.
Article18. Hüttemann M, Pecina P, Rainbolt M, Sanderson TH, Kagan VE, Samavati L, Doan JW, Lee I. The multiple functions of cytochrome c and their regulation in life and death decisions of the mammalian cell: from respiration to apoptosis. Mitochondrion. 2011; 11:369–381.
Article19. Ishikawa S, Griesdale DE, Lohser J. Acute kidney injury after lung resection surgery: incidence and perioperative risk factors. Anesth Analg. 2012; 114:1256–1262.20. Lopes JA, Fernandes P, Jorge S, Gonçalves S, Alvarez A, Costa e Silva Z, França C, Prata MM. Acute kidney injury in intensive care unit patients: a comparison between the RIFLE and the Acute Kidney Injury Network classifications. Crit Care. 2008; 12:R110.
Article21. Madjdpour C, Dettori N, Frascarolo P, Burki M, Boll M, Fisch A, Bombeli T, Spahn DR. Molecular weight of hydroxyethyl starch: is there an effect on blood coagulation and pharmacokinetics? Br J Anaesth. 2005; 94:569–576.
Article22. Magder S, Potter BJ, Varennes BD, Doucette S, Fergusson D. Fluids after cardiac surgery: a pilot study of the use of colloids versus crystalloids. Crit Care Med. 2010; 38:2117–2124.
Article23. Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG, Levin A. Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007; 11:R31.
Article24. Mitrowska K, Posyniak A, Zmudzki J. Rapid method for the determination of tranquilizers and a beta-blocker in porcine and bovine kidney by liquid chromatography with tandem mass spectrometry. Anal Chim Acta. 2009; 637:185–192.
Article25. Molitoris BA. Acute renal failure. Drugs Today (Barc). 1999; 35:659–666.
Article26. Moran M, Kapsner C. Acute renal failure associated with elevated plasma oncotic pressure. N Engl J Med. 1987; 317:150–153.
Article27. Myers BD, Carrie BJ, Yee RR, Hilberman M, Michaels AS. Pathophysiology of hemodynamically mediated acute renal failure in man. Kidney Int. 1980; 18:495–504.
Article28. Ortiz AL, Vala H, Venâncio C, Mesquita J, Silva A, Gonzalo-Orden JM, Ferreira D. The influence of Ringer's lactate or HES 130/0.4 administration on the integrity of the small intestinal mucosa in a pig hemorrhagic shock model under general anesthesia. J Vet Emerg Crit Care (San Antonio). 2017; 27:96–107.
Article29. Piriou V, Chiari P, Lehot JJ, Foëx P, Arvieux CC. Effects of propofol on haemodynamics and on regional blood flows in dogs submitted or not to a volaemic expansion. Eur J Anaesthesiol. 1999; 16:615–621.
Article30. Saigusa S, Inoue Y, Tanaka K, Okugawa Y, Toiyama Y, Uchida K, Mohri Y, Kusunoki M. Lack of M30 expression correlates with factors reflecting tumor progression in rectal cancer with preoperative chemoradiotherapy. Mol Clin Oncol. 2014; 2:99–104.
Article31. Saraste A, Pulkki K. Morphologic and biochemical hallmarks of apoptosis. Cardiovasc Res. 2000; 45:528–537.
Article32. Silva A, Ortiz AL, Venâncio C, Souza AP, Ferreira LM, Branco PS, de Pinho PG, Amorim P, Ferreira DA. Effects of acute bleeding followed by hydroxyethyl starch 130/0.4 or a crystalloid on propofol concentrations, cerebral oxygenation, and electroencephalographic and haemodynamic variables in pigs. Vet Med Int. 2014; 2014:710394.
Article33. Silva A, Venâncio C, Ortiz AL, Souza AP, Amorim P, Ferreira DA. The effect of high doses of remifentanil in brain near-infrared spectroscopy and in electroencephalographic parameters in pigs. Vet Anaesth Analg. 2014; 41:153–162.
Article34. Tervaert TW, Mooyaart AL, Amann K, Cohen AH, Cook HT, Drachenberg CB, Ferrario F, Fogo AB, Haas M, de Heer E, Joh K, Noël LH, Radhakrishnan J, Seshan SV, Bajema IM, Bruijn JA. Pathologic classification of diabetic nephropathy. J Am Soc Nephrol. 2010; 21:556–563.
Article35. Vianna PT, Castiglia YM, Braz JR, Viero RM, Beier S, Vianna Filho PT, Vitória A, Reinoldes Bizarria Guilherme G, de Assis Golim M, Deffune E. Remifentanil, isoflurane, and preconditioning attenuate renal ischemia/reperfusion injury in rats. Transplant Proc. 2009; 41:4080–4082.
Article36. Wang X. The expanding role of mitochondria in apoptosis. Genes Dev. 2001; 15:2922–2933.37. Winkelmayer WC, Glynn RJ, Levin R, Avorn J. Hydroxyethyl starch and change in renal function in patients undergoing coronary artery bypass graft surgery. Kidney Int. 2003; 64:1046–1049.
Article38. Zawadzka I, Rodziewicz L. [Determination of azaperone and carazolol residues in animals kidney using LC-MS/MS method]. Rocz Panstw Zakl Hig. 2009; 60:19–23. Polish.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of hydroxyethyl starch on blood glucose levels
- The effect of 6% hydroxyethyl starch 130/0.4 preloading on the blood glucose levels in diabetic patients undergoing orthopedic surgery with spinal anesthesia: a randomized pilot study
- Recent findings on the use of hydroxyethyl starch
- The Effects of Low Molecular Weight Hydroxyethyl Starch Replacement Solution in Acute Normovolemic Hemodilution
- Effects of Intravascular Volume Therapy with a Hydroxyethyl Starch (HES 130/0.4) on Blood Coagulation in Children Undergoing Cardiac Surgery