Anesth Pain Med.
2023 Apr;18(2):139-147. 10.17085/apm.22246.
The effect of 6% hydroxyethyl starch 130/0.4 preloading on the blood glucose levels in diabetic patients undergoing orthopedic surgery with spinal anesthesia: a randomized pilot study
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Chosun University Hospital, Gwangju, Korea
- 2Department of Anesthesiology and Pain Medicine, School of Medicine, Chosun University, Gwangju, Korea
- 3Department of Anesthesiology and Pain Medicine, Yonsei Bon Hospital, Seoul, Korea
- KMID: 2543655
- DOI: http://doi.org/10.17085/apm.22246
Abstract
- Background
Perioperative hyperglycemia can occur in surgical patients and may increase postoperative morbidity and mortality, especially in patients with diabetes. Therefore, we conducted the present study to evaluate whether the administration of 6% hydroxyethyl starch (HES)-130/0.4 increases blood glucose levels in patients with diabetes.
Methods
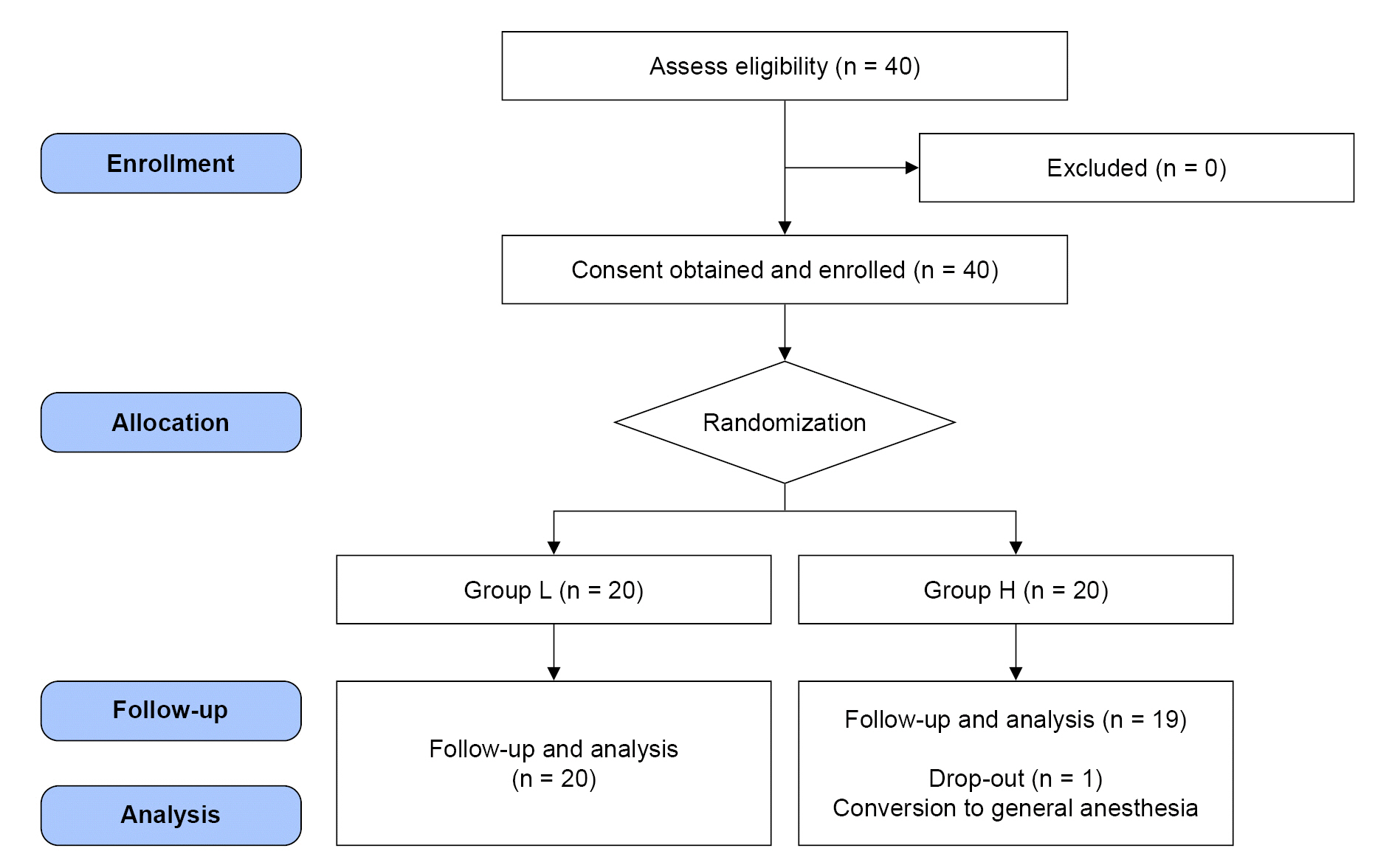
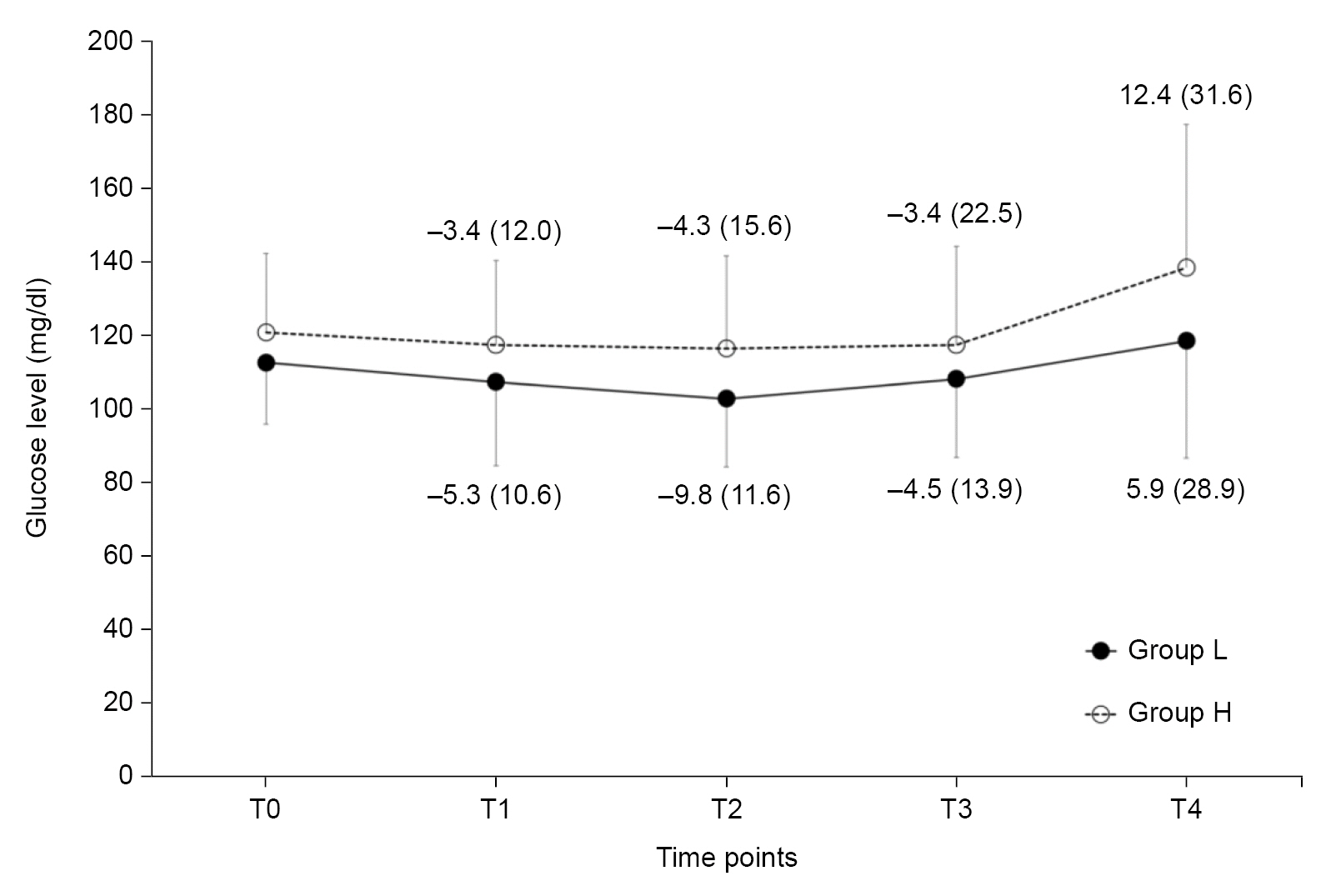
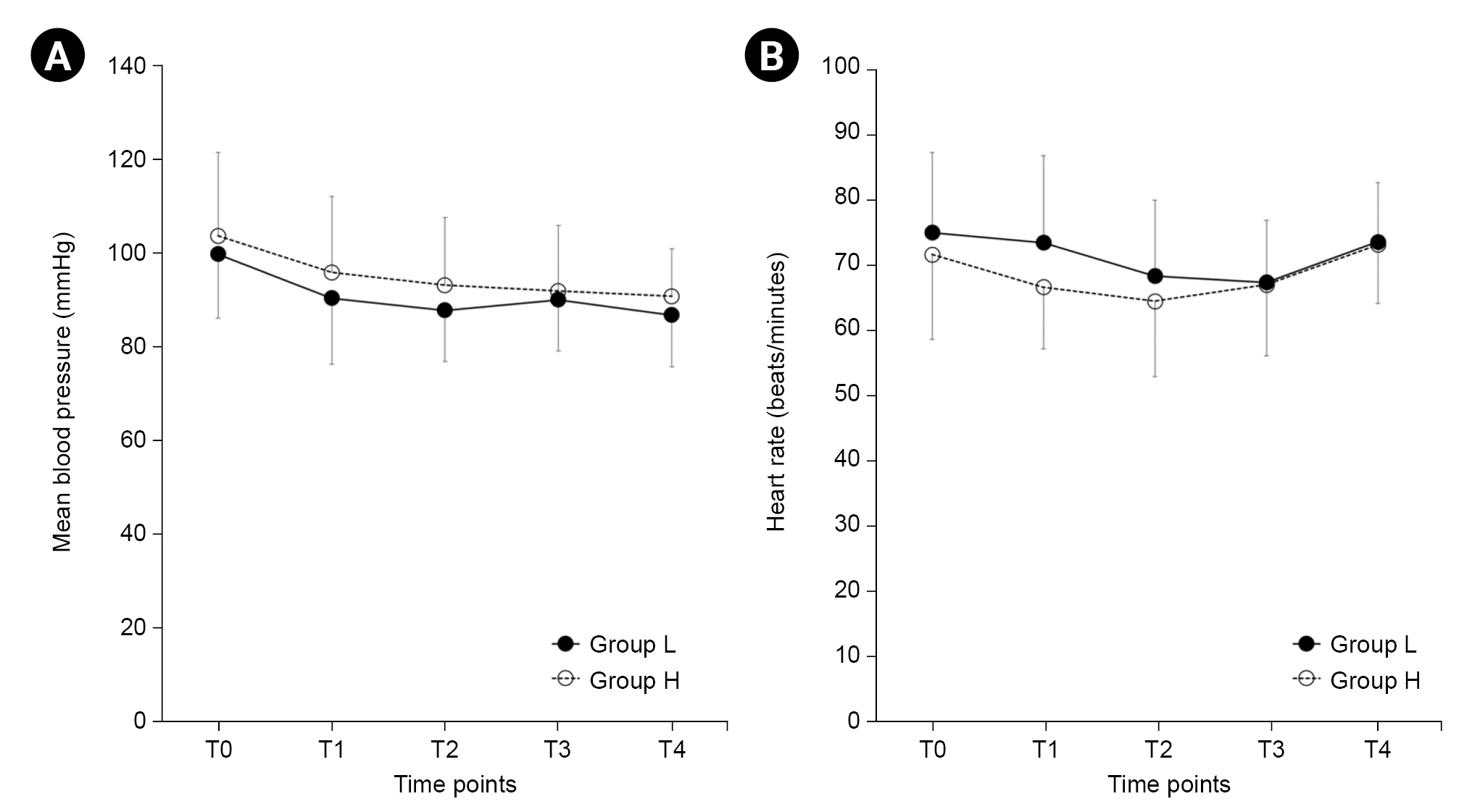
Forty patients undergoing lower limb surgery under spinal anesthesia were randomly allocated into two groups according to the fluids administered 20 min before spinal anesthesia (Group L, lactated Ringer’s solution; Group H, 6% HES-130/0.4). Patient characteristics, intraoperative variables, blood glucose levels, mean blood pressure (MBP), and heart rate (HR) were recorded at five time-points (0, 20, 60, 120, and 240 min).
Results
A total of 39 patients were analyzed (Group L, n = 20; Group H, n = 19). The amount of intraoperative fluid was significantly higher in Group L than in Group H (718.2 ml vs. 530.0 ml, P = 0.010). There were no significant differences in the changes in blood glucose levels, HR, or MBP between the two groups (P = 0.737, P = 0.896, and P = 0.141, respectively). Serial changes in mean blood glucose levels from baseline also showed no significant differences between the groups (P = 0.764).
Conclusions
There were no significant changes in blood glucose levels when lactated Ringer’s solution or 6% HES-130 was used. When compared to the lactated Ringer’s solution, no evidence that 6% HES-130/0.4 produces hyperglycemia in diabetic patients could be found. Further evaluation of larger populations is needed.
Keyword
Figure
Reference
-
1. Duggan EW, Carlson K, Umpierrez GE. Perioperative hyperglycemia management: an update. Anesthesiology. 2017; 126:547–60.2. Seo KH. Perioperative glucocorticoid management based on current evidence. Anesth Pain Med (Seoul). 2021; 16:8–15.
Article3. Vriesendorp TM, Morélis QJ, Devries JH, Legemate DA, Hoekstra JB. Early post-operative glucose levels are an independent risk factor for infection after peripheral vascular surgery. A retrospective study. Eur J Vasc Endovasc Surg. 2004; 28:520–5.
Article4. Cheisson G, Jacqueminet S, Cosson E, Ichai C, Leguerrier AM, Nicolescu-Catargi B, et al. Perioperative management of adult diabetic patients. Intraoperative period. Anaesth Crit Care Pain Med. 2018; 37 Suppl 1:S21–5.5. Lee SY, Lee KM, Lee JG, Lim JA, Woo NS, Lee YC. Effect of hyperglycemia on the length of postoperative hospital stay. Korean J Anesthesiol. 2005; 48:565–9.
Article6. Frisch A, Chandra P, Smiley D, Peng L, Rizzo M, Gatcliffe C, et al. Prevalence and clinical outcome of hyperglycemia in the perioperative period in noncardiac surgery. Diabetes Care. 2010; 33:1783–8.
Article7. Jeon YS. Recent findings on the use of hydroxyethyl starch. Anesth Pain Med. 2014; 9:159–64.8. Myburgh JA. Fluid resuscitation in acute medicine: what is the current situation? J Intern Med. 2015; 277:58–68.
Article9. Jungheinrich C, Neff TA. Pharmacokinetics of hydroxyethyl starch. Clin Pharmacokinet. 2005; 44:681–99.
Article10. Buggy D, Higgins P, Moran C, O'Brien D, O'Donovan F, McCarroll M. Prevention of spinal anesthesia-induced hypotension in the elderly: comparison between preanesthetic administration of crystalloids, colloids, and no prehydration. Anesth Analg. 1997; 84:106–10.11. Chawnchhim AL, Jacob M, Jaiswal A, Paul D, Kaur KB, Ray A, et al. Effect of hydroxyethyl starch on blood sugar levels in surgeries under subarachnoid block: a cross-sectional study. J Clin Diagnostic Res. 2020; 14:UC11–4.
Article12. Jung KT, Shim SB, Choi WY, An TH. Effect of hydroxyethyl starch on blood glucose levels. Korean J Anesthesiol. 2016; 69:350–6.
Article13. Lou S, Bian L, Long C, Wang Z, Ma J, Zhou B. Does 6% hydroxyethyl starch 130/0.4 impact differently on blood glucose than 4% gelatin in patients receiving open heart surgery? Perfusion. 2012; 27:113–8.
Article14. Murty SS, Kamath SK, Chaudhari LS. Effects of hydroxyethyl starches on blood sugar levels: a randomized double blind study. Indian J Anaesth. 2004; 48:196–200.15. Patki A, Shelgaonkar V. Effect of 6% hydroxyethyl starch-450 and low molecular weight dextran on blood sugar levels during surgery under subarachnoid block: a prospective randomised study. Indian J Anaesth. 2010; 54:448–52.
Article16. Chandra AP. Effects of preloading with isotonically balanced tetra hydroxyethyl starch versus preloading with gelufusine on blood glucose level in diabetic patients. Acad Anesthesiol Int. 2020; 5:162–7.17. Marks JB. Perioperative management of diabetes. Am Fam Physician. 2003; 67:93–100.18. Sudhakaran S, Surani SR. Guidelines for perioperative management of the diabetic patient. Surg Res Pract. 2015; 2015:284063.
Article19. American Diabetes Association. 14. Diabetes care in the hospital: standards of medical care in diabetes-2018. Diabetes Care. 2018; 41(Suppl 1):S144–51.20. Kang H. Sample size determination for repeated measures design using G Power software. Anesth Pain Med. 2015; 10:6–15.
Article21. Cohen J. A power primer. Psychol Bull. 1992; 112:155–9.
Article22. Gottschalk A, Rink B, Smektala R, Piontek A, Ellger B, Gottschalk A. Spinal anesthesia protects against perioperative hyperglycemia in patients undergoing hip arthroplasty. J Clin Anesth. 2014; 26:455–60.
Article23. Baron JF. A new hydroxyethyl starch: HES 130/0.4 Voluven®. Transfus Altern Transfus Med. 2000; 2:13–21.24. Kirch W, Köhler H, Horstmann HJ. Retarded elimination of a high-molecular enzyme-substrate-complex after hydroxyethyl-starch-infusion. Toxicological aspects of food safety. In : Leonard BJ, editor. Berlin: Springer;1978. p. 335–8.25. Yadav R, Bhartiya JP, Verma SK, Nandkeoliar MK. The evaluation of serum amylase in the patients of type 2 diabetes mellitus, with a possible correlation with the pancreatic functions. J Clin Diagn Res. 2013; 7:1291–4.
Article26. Bajwa SJ, Kulshrestha A, Jindal R. Co-loading or pre-loading for prevention of hypotension after spinal anaesthesia! A therapeutic dilemma. Anesth Essays Res. 2013; 7:155–9.
Article27. Kim CS, Ahn HJ, Shin SH, Choi DH. Prevention of hypotension with crystalloid versus colloid during spinal or combined spinal-epidural anesthesia for cesarean delivery. Korean J Anesthesiol. 2004; 46:408–13.
Article28. Mannion JD, Rather A, Manifold S, Gardner K, McEvilly M, Yaeger J, et al. Postoperative hyperglycemia in patients with and without diabetes after major joint replacement: the impact of an enhanced glucose management program. JB JS Open Access. 2021; 6:e20.00172.
Article29. Thomas DJ, Alberti KG. Hyperglycaemic effects of Hartmann's solution during surgery in patients with maturity onset diabetes. Br J Anaesth. 1978; 50:185–8.
Article30. Simpson AK, Levy N, Hall GM. Peri-operative i.v. fluids in diabetic patients--don't forget the salt. Anaesthesia. 2008; 63:1043–5.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of hydroxyethyl starch on blood glucose levels
- Effect of 10% Pentastarch Preloading on Hemodynamic Changes during Transurethral Resection of Prostate (TURP) under Spinal Anesthesia
- The Effects of 10 % Pentastarch Preloading for Cesarean Section Under Epidural Anesthesia
- Recent findings on the use of hydroxyethyl starch
- The Effect of 6% Hydroxyethyl Starch 130/0.4 on Hemostasis and Hemodynamic Efficacy in Off-pump Coronary Artery Bypass Surgery: a Comparison with 6% Hydroxyethyl Starch 200/0.5