World J Mens Health.
2018 Sep;36(3):199-222. 10.5534/wjmh.180032.
Impact of Testosterone Deficiency and Testosterone Therapy on Lower Urinary Tract Symptoms in Men with Metabolic Syndrome
- Affiliations
-
- 1Department of Urology, Boston University School of Medicine, Boston, MA, USA. atraish@bu.edu
- KMID: 2419321
- DOI: http://doi.org/10.5534/wjmh.180032
Abstract
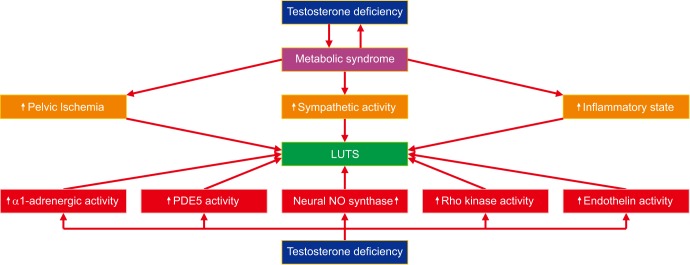
- Lower urinary tract function is modulated by neural, vascular and urethral and bladder structural elements. The pathophysiological mechanisms of lower urinary tract symptoms (LUTS) encompass prostate enlargement, alterations in urethra histological structure bladder fibrosis and alterations in pelvic neuronal and vascular networks, The complex pathophysiological relationship between testosterone (T) deficiency (TD) and the constellations LUTS, and metabolic dysfunction manifested in the metabolic syndrome (Met S) remains poorly understood. TD has emerged as one the potential targets by which Met S may contribute to the onset and development as well as worsening of LUTS. Because it has been recognized that treatment of men with Met S with T therapy ameliorates Met S components, it is postulated that T therapy may represent a therapeutic target in improving LUTS. Furthermore, the effect of TD on the prostate remains unclear, and often debatable. It is believed that T exclusively promotes prostate growth, however recent evidence has strongly contradicted this belief. The true relationship between benign prostatic hyperplasia, TD, and LUTS remains elusive and further research will be required to clarify the role of T in both benign prostatic hypertrophy (BPH) and LUTS as a whole. Although there is conflicting evidence about the benefits of T therapy in men with BPH and LUTS, the current body of literature supports the safety of using this therapy in men with enlarged prostate. As the population afflicted with obesity epidemic continues to age, the number of men suffering from Met S and LUTS together is expected to increase.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Diagnosis and treatment of sexual dysfunction in elderly men
Hyun Jun Park
J Korean Med Assoc. 2019;62(6):308-314. doi: 10.5124/jkma.2019.62.6.308.
Reference
-
1. Vignozzi L, Gacci M, Maggi M. Lower urinary tract symptoms, benign prostatic hyperplasia and metabolic syndrome. Nat Rev Urol. 2016; 13:108–119. PMID: 26754190.
Article2. Traish AM, Guay A, Feeley R, Saad F. The dark side of testosterone deficiency: I. Metabolic syndrome and erectile dysfunction. J Androl. 2009; 30:10–22. PMID: 18641413.
Article3. Traish AM, Saad F, Guay A. The dark side of testosterone deficiency: II. Type 2 diabetes and insulin resistance. J Androl. 2009; 30:23–32. PMID: 18772488.
Article4. Traish AM, Saad F, Feeley RJ, Guay A. The dark side of testosterone deficiency: III. Cardiovascular disease. J Androl. 2009; 30:477–494. PMID: 19342698.
Article5. Grosman H, Fabre B, Lopez M, Scorticati C, Lopez Silva M, Mesch V, et al. Complex relationship between sex hormones, insulin resistance and leptin in men with and without prostatic disease. Aging Male. 2016; 19:40–45. PMID: 26526283.
Article6. Hsu B, Cumming RG, Naganathan V, Blyth FM, Le Couteur DG, Seibel MJ, et al. Associations between circulating reproductive hormones and SHBG and prevalent and incident metabolic syndrome in community-dwelling older men: the Concord Health and Ageing in Men Project. J Clin Endocrinol Metab. 2014; 99:E2686–E2691. PMID: 25259909.
Article7. Rao PM, Kelly DM, Jones TH. Testosterone and insulin resistance in the metabolic syndrome and T2DM in men. Nat Rev Endocrinol. 2013; 9:479–493. PMID: 23797822.
Article8. Maneschi E, Morelli A, Filippi S, Cellai I, Comeglio P, Mazzanti B, et al. Testosterone treatment improves metabolic syndrome-induced adipose tissue derangements. J Endocrinol. 2012; 215:347–362. PMID: 23045189.
Article9. Wang C, Jackson G, Jones TH, Matsumoto AM, Nehra A, Perelman MA, et al. Low testosterone associated with obesity and the metabolic syndrome contributes to sexual dysfunction and cardiovascular disease risk in men with type 2 diabetes. Diabetes Care. 2011; 34:1669–1675. PMID: 21709300.
Article10. Muraleedharan V, Jones TH. Testosterone and the metabolic syndrome. Ther Adv Endocrinol Metab. 2010; 1:207–223. PMID: 23148165.11. Corona G, Monami M, Rastrelli G, Aversa A, Tishova Y, Saad F, et al. Testosterone and metabolic syndrome: a meta-analysis study. J Sex Med. 2011; 8:272–283. PMID: 20807333.
Article12. Zitzmann M. Testosterone deficiency, insulin resistance and the metabolic syndrome. Nat Rev Endocrinol. 2009; 5:673–681. PMID: 19859074.
Article13. Stanworth RD, Jones TH. Testosterone in obesity, metabolic syndrome and type 2 diabetes. Front Horm Res. 2009; 37:74–90. PMID: 19011290.
Article14. Gorbachinsky I, Akpinar H, Assimos DG. Metabolic syndrome and urologic diseases. Rev Urol. 2010; 12:e157–e180. PMID: 21234260.15. Lee JH, Kwon H, Park YW. Association of lower urinary tract symptom/benign prostatic hyperplasia measures with international index of erectile function 5 in middle-aged policemen of Korea and the role of metabolic syndrome and testosterone in their relationship. Urology. 2013; 82:1008–1012. PMID: 24041675.
Article16. De Nunzio C, Cindolo L, Gacci M, Pellegrini F, Carini M, Lombardo R, et al. Metabolic syndrome and lower urinary tract symptoms in patients with benign prostatic enlargement: a possible link to storage symptoms. Urology. 2014; 84:1181–1187. PMID: 25443931.
Article17. Kseneva SI, Yurmazov ZA, Timofeev MS, Borodulina EV, Udut VV. Lower urinary tract symptoms in metabolic syndrome in young adults. Endocr Metab Immune Disord Drug Targets. 2018; 18:230–234. PMID: 29437022.
Article18. Ozer K, Horsanali MO, Gorgel SN, Horsanali BO, Ozbek E. Association between benign prostatic hyperplasia and neutrophil-lymphocyte ratio, an indicator of inflammation and metabolic syndrome. Urol Int. 2017; 98:466–471. PMID: 27464069.
Article19. Zhao S, Chen C, Chen Z, Xia M, Tang J, Shao S, et al. Relationship between metabolic syndrome and predictors for clinical benign prostatic hyperplasia progression and international prostate symptom score in patients with moderate to severe lower urinary tract symptoms. Urol J. 2016; 13:2717–2726. PMID: 27351328.20. Rył A, Rotter I, Słojewski M, Jędrzychowska A, Marcinowska Z, Grabowska M, et al. Can metabolic disorders in aging men contribute to prostatic hyperplasia eligible for transurethral resection of the prostate (TURP)? Int J Environ Res Public Health. 2015; 12:3327–3342. PMID: 25809513.21. Russo GI, Castelli T, Urzì D, Privitera S, Fragalà E, La Vignera S, et al. Connections between lower urinary tract symptoms related to benign prostatic enlargement and metabolic syndrome with its components: a systematic review and meta-analysis. Aging Male. 2015; 18:207–216. PMID: 26171768.
Article22. Gooren L. Androgen deficiency in the aging male: benefits and risks of androgen supplementation. J Steroid Biochem Mol Biol. 2003; 85:349–355. PMID: 12943721.
Article23. Pradidarcheep W. Lower urinary tract symptoms and its potential relation with late-onset hypogonadism. Aging Male. 2008; 11:51–55. PMID: 18570055.
Article24. Chang IH, Oh SY, Kim SC. A possible relationship between testosterone and lower urinary tract symptoms in men. J Urol. 2009; 182:215–220. PMID: 19447426.
Article25. Demir O, Akgul K, Akar Z, Cakmak O, Ozdemir I, Bolukbasi A, et al. Association between severity of lower urinary tract symptoms, erectile dysfunction and metabolic syndrome. Aging Male. 2009; 12:29–34. PMID: 19326294.
Article26. Vignozzi L, Cellai I, Santi R, Lombardelli L, Morelli A, Comeglio P, et al. Antiinflammatory effect of androgen receptor activation in human benign prostatic hyperplasia cells. J Endocrinol. 2012; 214:31–43. PMID: 22562653.
Article27. Park YW, Min SK, Lee JH. Relationship between lower urinary tract symptoms/benign prostatic hyperplasia and metabolic syndrome in Korean men. World J Mens Health. 2012; 30:183–188. PMID: 23596610.
Article28. Kwon H, Kang HC, Lee JH. Relationship between predictors of the risk of clinical progression of benign prostatic hyperplasia and metabolic syndrome in men with moderate to severe lower urinary tract symptoms. Urology. 2013; 81:1325–1329. PMID: 23602796.
Article29. Kristal AR, Arnold KB, Schenk JM, Neuhouser ML, Weiss N, Goodman P, et al. Race/ethnicity, obesity, health related behaviors and the risk of symptomatic benign prostatic hyperplasia: results from the prostate cancer prevention trial. J Urol. 2007; 177:1395–1400. PMID: 17382740.
Article30. Dahle SE, Chokkalingam AP, Gao YT, Deng J, Stanczyk FZ, Hsing AW. Body size and serum levels of insulin and leptin in relation to the risk of benign prostatic hyperplasia. J Urol. 2002; 168:599–604. PMID: 12131317.
Article31. Gacci M, Vignozzi L, Sebastianelli A, Salvi M, Giannessi C, De Nunzio C, et al. Metabolic syndrome and lower urinary tract symptoms: the role of inflammation. Prostate Cancer Prostatic Dis. 2013; 16:101–106. PMID: 23165431.
Article32. Gacci M, Corona G, Vignozzi L, Salvi M, Serni S, De Nunzio C, et al. Metabolic syndrome and benign prostatic enlargement: a systematic review and meta-analysis. BJU Int. 2015; 115:24–31.
Article33. Gacci M, Corona G, Sebastianelli A, Serni S, De Nunzio C, Maggi M, et al. Male lower urinary tract symptoms and cardiovascular events: a systematic review and meta-analysis. Eur Urol. 2016; 70:788–796. PMID: 27451136.
Article34. Gacci M, Sebastianelli A, Salvi M, De Nunzio C, Tubaro A, Gravas S, et al. The impact of central obesity on storage luts and urinary incontinence after prostatic surgery. Curr Urol Rep. 2016; 17:61. PMID: 27432378.
Article35. Kasturi S, Russell S, McVary KT. Metabolic syndrome and lower urinary tract symptoms secondary to benign prostatic hyperplasia. Curr Urol Rep. 2006; 7:288–292. PMID: 16930500.
Article36. Gratzke C, Bachmann A, Descazeaud A, Drake MJ, Madersbacher S, Mamoulakis C, et al. EAU Guidelines on the assessment of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol. 2015; 67:1099–1109. PMID: 25613154.
Article37. Vignozzi L, Gacci M, Cellai I, Santi R, Corona G, Morelli A, et al. Fat boosts, while androgen receptor activation counteracts, BPH-associated prostate inflammation. Prostate. 2013; 73:789–800. PMID: 23620238.
Article38. Kupelian V, McVary KT, Kaplan SA, Hall SA, Link CL, Aiyer LP, et al. Association of lower urinary tract symptoms and the metabolic syndrome: results from the Boston Area Community Health Survey. J Urol. 2009; 182:616–624. PMID: 19539955.
Article39. Besiroglu H, Dursun M, Otunctemur A, Ozbek E. The association between triglyceride high density lipoprotein cholesterol ratio and benign prostate hyperplasia in non-diabetic patients:a cross-sectional study. Aging Male. 2017; 20:198–204. PMID: 28332908.
Article40. Kim YH, Kim JJ, Kim SM, Choi Y, Jeon MJ. Association between metabolic syndrome and pelvic floor dysfunction in middle-aged to older Korean women. Am J Obstet Gynecol. 2011; 205:71.e1–71.e8. PMID: 21481837.
Article41. Laaksonen DE, Niskanen L, Punnonen K, Nyyssönen K, Tuomainen TP, Valkonen VP, et al. Testosterone and sex hormone-binding globulin predict the metabolic syndrome and diabetes in middle-aged men. Diabetes Care. 2004; 27:1036–1041. PMID: 15111517.
Article42. Laaksonen DE, Niskanen L, Punnonen K, Nyyssönen K, Tuomainen TP, Valkonen VP, et al. The metabolic syndrome and smoking in relation to hypogonadism in middle-aged men: a prospective cohort study. J Clin Endocrinol Metab. 2005; 90:712–719. PMID: 15536158.
Article43. Kupelian V, Page ST, Araujo AB, Travison TG, Bremner WJ, McKinlay JB. Low sex hormone-binding globulin, total testosterone, and symptomatic androgen deficiency are associated with development of the metabolic syndrome in nonobese men. J Clin Endocrinol Metab. 2006; 91:843–850. PMID: 16394089.
Article44. Rodriguez A, Muller DC, Metter EJ, Maggio M, Harman SM, Blackman MR, et al. Aging, androgens, and the metabolic syndrome in a longitudinal study of aging. J Clin Endocrinol Metab. 2007; 92:3568–3572. PMID: 17595254.
Article45. Akishita M, Fukai S, Hashimoto M, Kameyama Y, Nomura K, Nakamura T, et al. Association of low testosterone with metabolic syndrome and its components in middle-aged Japanese men. Hypertens Res. 2010; 33:587–591. PMID: 20339372.
Article46. Katabami T, Kato H, Asahina T, Hinohara S, Shin T, Kawata T, et al. Serum free testosterone and metabolic syndrome in Japanese men. Endocr J. 2010; 57:533–539. PMID: 20371984.
Article47. Liao CH, Huang CY, Li HY, Yu HJ, Chiang HS, Liu CK. Testosterone and sex hormone-binding globulin have significant association with metabolic syndrome in Taiwanese men. Aging Male. 2012; 15:1–6. PMID: 22091971.
Article48. Chin KY, Ima-Nirwana S, Mohamed IN, Aminuddin A, Ngah WZ. Total testosterone and sex hormone-binding globulin are significantly associated with metabolic syndrome in middle-aged and elderly men. Exp Clin Endocrinol Diabetes. 2013; 121:407–412. PMID: 23765753.
Article49. Chrysohoou C, Panagiotakos D, Pitsavos C, Siasos G, Oikonomou E, Varlas J, et al. Low total testosterone levels are associated with the metabolic syndrome in elderly men: the role of body weight, lipids, insulin resistance, and inflammation; the Ikaria study. Rev Diabet Stud. 2013; 10:27–38. PMID: 24172696.
Article50. Haring R, Völzke H, Spielhagen C, Nauck M, Wallaschofski H. The role of sex hormone-binding globulin and testosterone in the risk of incident metabolic syndrome. Eur J Prev Cardiol. 2013; 20:1061–1068. PMID: 22711969.
Article51. Kweon SS, Shin MH, Nam HS, Jeong SK, Park KS, Choi JS, et al. Sex differences in the associations of testosterone and sex hormone-binding globulin with metabolic syndrome in middle-aged and elderly Koreans: the Namwon study. Circ J. 2013; 77:734–740. PMID: 23182833.52. Tsujimura A, Miyagawa Y, Takezawa K, Okuda H, Fukuhara S, Kiuchi H, et al. Is low testosterone concentration a risk factor for metabolic syndrome in healthy middle-aged men? Urology. 2013; 82:814–819. PMID: 24074976.
Article53. Zhang J, Huang X, Liao M, Gao Y, Tan A, Yang X, et al. Both total testosterone and sex hormone-binding globulin are independent risk factors for metabolic syndrome: results from Fangchenggang Area Male Health and Examination Survey in China. Diabetes Metab Res Rev. 2013; 29:391–397. PMID: 23463406.
Article54. García-Cruz E, Leibar-Tamayo A, Romero-Otero J, Asiaín I, Carrión A, Castañeda R, et al. Marked testosterone deficiency-related symptoms may be associated to higher metabolic risk in men with low testosterone levels. J Sex Med. 2014; 11:2292–2301. PMID: 24975551.55. Grosman H, Rosales M, Fabre B, Nolazco C, Mazza O, Berg G, et al. Association between testosterone levels and the metabolic syndrome in adult men. Aging Male. 2014; 17:161–165. PMID: 24828370.
Article56. Antonio L, Wu FC, O'Neill TW, Pye SR, Carter EL, Finn JD, et al. Associations between sex steroids and the development of metabolic syndrome: a longitudinal study in European men. J Clin Endocrinol Metab. 2015; 100:1396–1404. PMID: 25636052.
Article57. Naifar M, Rekik N, Messedi M, Chaabouni K, Lahiani A, Turki M, et al. Male hypogonadism and metabolic syndrome. Andrologia. 2015; 47:579–586. PMID: 25040289.
Article58. Wickramatilake CM, Mohideen MR, Pathirana C. Association of metabolic syndrome with testosterone and inflammation in men. Ann Endocrinol (Paris). 2015; 76:260–263. PMID: 26142486.
Article59. Yang YH, Zhao MJ, Zhou SJ, Lu WH, Liang XW, Xiong CL, et al. Is serum sex hormone-binding globulin a dominant risk factor for metabolic syndrome? Asian J Androl. 2015; 17:991–995. PMID: 25851658.
Article60. Blaya R, Thomaz LD, Guilhermano F, Paludo Ade O, Rhoden L, Halmenschlager G, et al. Total testosterone levels are correlated to metabolic syndrome components. Aging Male. 2016; 19:85–89. PMID: 26961662.
Article61. Moon H, Choi I, Kim S, Ko H, Shin J, Lee K, et al. Cross-sectional association between testosterone, sex hormone-binding globulin and metabolic syndrome: the healthy twin study. Clin Endocrinol (Oxf). 2017; 87:523–531. PMID: 28581026.
Article62. Laouali N, Brailly-Tabard S, Helmer C, Ancelin ML, Tzourio C, Singh-Manoux A, et al. Testosterone and all-cause mortality in older men: the role of metabolic syndrome. J Endocr Soc. 2018; 2:322–335. PMID: 29577108.
Article63. Cunningham GR. Testosterone and metabolic syndrome. Asian J Androl. 2015; 17:192–196. PMID: 25652634.
Article64. Corona G, Vignozzi L, Sforza A, Mannucci E, Maggi M. Obesity and late-onset hypogonadism. Mol Cell Endocrinol. 2015; 418:120–133. PMID: 26143633.
Article65. Maggio M, Lauretani F, Ceda GP, Bandinelli S, Basaria S, Paolisso G, et al. Estradiol and metabolic syndrome in older italian men: The InCHIANTI Study. J Androl. 2010; 31:155–162. PMID: 19059904.
Article66. Braga-Basaria M, Dobs AS, Muller DC, Carducci MA, John M, Egan J, et al. Metabolic syndrome in men with prostate cancer undergoing long-term androgen-deprivation therapy. J Clin Oncol. 2006; 24:3979–3983. PMID: 16921050.
Article67. Brand JS, Rovers MM, Yeap BB, Schneider HJ, Tuomainen TP, Haring R, et al. Testosterone, sex hormone-binding globulin and the metabolic syndrome in men: an individual participant data meta-analysis of observational studies. PLoS One. 2014; 9:e100409. PMID: 25019163.
Article68. Saylor PJ, Smith MR. Metabolic complications of androgen deprivation therapy for prostate cancer. J Urol. 2013; 189:S34–S42. PMID: 23234628.
Article69. Mitsuzuka K, Arai Y. Metabolic changes in patients with prostate cancer during androgen deprivation therapy. Int J Urol. 2018; 25:45–53. PMID: 29052905.
Article70. Yucel C, Keskin MZ, Peskircioglu CL. The effect of transdermal testosterone administration on lower urinary tract symptoms and erectile dysfunction: a prospective, randomized, placebo-controlled trial. Curr Urol. 2017; 11:4–8. PMID: 29463970.
Article71. Shigehara K, Izumi K, Mizokami A, Namiki M. Testosterone deficiency and nocturia: a review. World J Mens Health. 2017; 35:14–21. PMID: 28459143.
Article72. Shim JS, Kim JH, Yoon YS, Choi H, Park JY, Bae JH. Serum testosterone levels are negatively correlated with international prostate symptom score and transitional prostate volume. Low Urin Tract Symptoms. 2018; 10:143–147. PMID: 29664237.
Article73. Haider KS, Haider A, Doros G, Traish A. Long-term testosterone therapy improves urinary and sexual function, and quality of life in men with hypogonadism: results from a propensity matched subgroup of a controlled registry study. J Urol. 2018; 199:257–265. PMID: 28728990.
Article74. De Nunzio C, Brassetti A, Proietti F, Deroma M, Esperto F, Tubaro A. Metabolic syndrome and smoking are associated with an increased risk of nocturia in male patients with benign prostatic enlargement. Prostate Cancer Prostatic Dis. 2017; [Epub]. DOI: 10.1038/s41391-017-0003-z.
Article75. Russo GI, Regis F, Spatafora P, Frizzi J, Urzì D, Cimino S, et al. Association between metabolic syndrome and intravesical prostatic protrusion in patients with benign prostatic enlargement and lower urinary tract symptoms (MIPS Study). BJU Int. 2018; 121:799–804. PMID: 28872764.
Article76. Wang JY, Fu YY, Kang DY. The association between metabolic syndrome and characteristics of benign prostatic hyperplasia: a systematic review and meta-analysis. Medicine (Baltimore). 2016; 95:e3243. PMID: 27175628.77. Kwon T, Park S, Park S, Moon KH. Metabolic syndrome is predictive of lower urinary tract symptom improvement after holmium laser enucleation of the prostate for benign prostatic obstruction. Int Urol Nephrol. 2017; 49:1105–1110. PMID: 28361474.
Article78. Favilla V, Cimino S, Castelli T, Madonia M, Barbagallo I, Morgia G. Relationship between lower urinary tract symptoms and serum levels of sex hormones in men with symptomatic benign prostatic hyperplasia. BJU Int. 2010; 106:1700–1703. PMID: 20575982.
Article79. Fu Y, Zhou Z, Yang B, Zhang K, He L, Zhang X. The relationship between the clinical progression of benign prostatic hyperplasia and metabolic syndrome: a prospective study. Urol Int. 2016; 97:330–335. PMID: 27509202.
Article80. Lee S, Min HG, Choi SH, Kim YJ, Oh SW, Kim YJ, et al. Central obesity as a risk factor for prostatic hyperplasia. Obesity (Silver Spring). 2006; 14:172–179. PMID: 16493136.
Article81. Muller RL, Gerber L, Moreira DM, Andriole G Jr, Hamilton RJ, Fleshner N, et al. Obesity is associated with increased prostate growth and attenuated prostate volume reduction by dutasteride. Eur Urol. 2013; 63:1115–1121. PMID: 23541458.
Article82. Pashootan P, Ploussard G, Cocaul A, de Gouvello A, Desgrandchamps F. Association between metabolic syndrome and severity of lower urinary tract symptoms (LUTS): an observational study in a 4666 European men cohort. BJU Int. 2015; 116:124–130. PMID: 25229124.
Article83. Rył A, Rotter I, Miazgowski T, Słojewski M, Dołęgowska B, Lubkowska A, et al. Metabolic syndrome and benign prostatic hyperplasia: association or coincidence? Diabetol Metab Syndr. 2015; 7:94. PMID: 26516352.
Article84. Shigehara K, Namiki M. Late-onset hypogonadism syndrome and lower urinary tract symptoms. Korean J Urol. 2011; 52:657–663. PMID: 22087358.
Article85. Schatzl G, Brössner C, Schmid S, Kugler W, Roehrich M, Treu T, et al. Endocrine status in elderly men with lower urinary tract symptoms: correlation of age, hormonal status, and lower urinary tract function. The Prostate Study Group of the Austrian Society of Urology. Urology. 2000; 55:397–402. PMID: 10699620.86. Litman HJ, Bhasin S, O'Leary MP, Link CL, McKinlay JB. An investigation of the relationship between sex-steroid levels and urological symptoms: results from the Boston Area Community Health survey. BJU Int. 2007; 100:321–326. PMID: 17506868.
Article87. Rohrmann S, Nelson WG, Rifai N, Kanarek N, Basaria S, Tsilidis KK, et al. Serum sex steroid hormones and lower urinary tract symptoms in Third National Health and Nutrition Examination Survey (NHANES III). Urology. 2007; 69:708–713. PMID: 17445656.
Article88. Trifiro MD, Parsons JK, Palazzi-Churas K, Bergstrom J, Lakin C, Barrett-Connor E. Serum sex hormones and the 20-year risk of lower urinary tract symptoms in community-dwelling older men. BJU Int. 2010; 105:1554–1559. PMID: 20002438.
Article89. Miwa Y, Kaneda T, Yokoyama O. Association between lower urinary tract symptoms and serum levels of sex hormones in men. Urology. 2008; 72:552–555. PMID: 18597822.
Article90. Tan MO, Karabiyik I, Uygur MC, Diker Y, Erol D. Serum concentrations of sex hormones in men with severe lower urinary tract symptoms and benign prostatic hyperplasia. Int Urol Nephrol. 2003; 35:357–363. PMID: 15160539.
Article91. Bravo G, Massa H, Rose'Meyer R, Chess-Williams R, McDermott C, Sellers DJ. Effect of short-term androgen deficiency on bladder contractility and urothelial mediator release. Naunyn Schmiedebergs Arch Pharmacol. 2017; 390:547–556. PMID: 28190243.
Article92. Vanella L, Russo GI, Cimino S, Fragalà E, Favilla V, Li Volti G, et al. Correlation between lipid profile and heme oxygenase system in patients with benign prostatic hyperplasia. Urology. 2014; 83:1444.e7–1444.e13.
Article93. Park HK, Lee HW, Lee KS, Byun SS, Jeong SJ, Hong SK, et al. Relationship between lower urinary tract symptoms and metabolic syndrome in a community-based elderly population. Urology. 2008; 72:556–560. PMID: 18597823.
Article94. Wang CC, Chancellor MB, Lin JM, Hsieh JH, Yu HJ. Type 2 diabetes but not metabolic syndrome is associated with an increased risk of lower urinary tract symptoms and erectile dysfunction in men aged <45 years. BJU Int. 2010; 105:1136–1140. PMID: 19804425.95. Gao Y, Wang M, Zhang H, Tan A, Yang X, Qin X, et al. Are metabolic syndrome and its components associated with lower urinary tract symptoms? Results from a Chinese male population survey. Urology. 2012; 79:194–201. PMID: 21924462.
Article96. Rohrmann S, Smit E, Giovannucci E, Platz EA. Association between markers of the metabolic syndrome and lower urinary tract symptoms in the Third National Health and Nutrition Examination Survey (NHANES III). Int J Obes (Lond). 2005; 29:310–316. PMID: 15672112.
Article97. Burnstock G. Therapeutic potential of purinergic signalling for diseases of the urinary tract. BJU Int. 2011; 107:192–204. PMID: 21208364.
Article98. Tanidir Y, Ercan F, Tarcan T. Exogenous testosterone and estrogen affect bladder tissue contractility and histomorphology differently in rat ovariectomy model. J Sex Med. 2011; 8:1626–1637. PMID: 21366882.
Article99. Fowler CJ. Editorial comment on: Influence of nerve transsections and combined bladder filling on intravesical electrostimulation-induced bladder contraction in the rat. Eur Urol. 2009; 56:533. PMID: 18472210.
Article100. Keast JR, Saunders RJ. Testosterone has potent, selective effects on the morphology of pelvic autonomic neurons which control the bladder, lower bowel and internal reproductive organs of the male rat. Neuroscience. 1998; 85:543–556. PMID: 9622251.
Article101. Birder L, Andersson KE. Urothelial signaling. Physiol Rev. 2013; 93:653–680. PMID: 23589830.
Article102. Hanna-Mitchell AT, Beckel JM, Barbadora S, Kanai AJ, de Groat WC, Birder LA. Non-neuronal acetylcholine and urinary bladder urothelium. Life Sci. 2007; 80:2298–2302. PMID: 17363007.
Article103. Maggi CA, Manzini S, Giuliani S, Meli A. Infravesical outflow obstruction in rats: a comparison of two models. Gen Pharmacol. 1989; 20:345–349. PMID: 2744400.
Article104. Pandita RK, Persson K, Hedlund P, Andersson KE. Testosterone-induced prostatic growth in the rat causes bladder overactivity unrelated to detrusor hypertrophy. Prostate. 1998; 35:102–108. PMID: 9568673.
Article105. Abdel-Hamid AA, Ali EM. Effect of testosterone therapy on the urinary bladder in experimental hypogonadism of rats. J Mol Histol. 2015; 46:263–272. PMID: 25805595.
Article106. Tek M, Balli E, Cimen B, Efesoy O, Oğuz I, Cayan S. The effect of testosterone replacement therapy on bladder functions and histology in orchiectomized mature male rats. Urology. 2010; 75:886–890. PMID: 19815256.
Article107. Celayir S. Effects of different sex hormones on male rabbit urodynamics: an experimental study. Horm Res. 2003; 60:215–220. PMID: 14614225.
Article108. Cheng CL, de Groat WC. Effect of orchiectomy and testosterone replacement on lower urinary tract function in anesthetized rats. Am J Physiol Renal Physiol. 2016; 311:F864–F870. PMID: 27534993.
Article109. Fernandes VS, Barahona MV, Recio P, Martínez-Sáenz A, Ribeiro AS, Contreras C, et al. Mechanisms involved in testosterone-induced relaxation to the pig urinary bladder neck. Steroids. 2012; 77:394–402. PMID: 22285851.
Article110. Hall R, Andrews PL, Hoyle CH. Effects of testosterone on neuromuscular transmission in rat isolated urinary bladder. Eur J Pharmacol. 2002; 449:301–309. PMID: 12167473.
Article111. Hristov KL, Parajuli SP, Provence A, Petkov GV. Testosterone decreases urinary bladder smooth muscle excitability via novel signaling mechanism involving direct activation of the BK channels. Am J Physiol Renal Physiol. 2016; 311:F1253–F1259. PMID: 27605581.
Article112. Ito H, Wang D, Zha X, Inamura S, Seki M, Taga M, et al. Castration increases PGE2 release from the bladder epithelium in male rats. Life Sci. 2018; 193:252–256. PMID: 29080694.113. Juan YS, Onal B, Broadaway S, Cosgrove J, Leggett RE, Whitbeck C, et al. Effect of castration on male rabbit lower urinary tract tissue enzymes. Mol Cell Biochem. 2007; 301:227–233. PMID: 17294138.
Article114. Zhang Y, Chen J, Hu L, Chen Z. Androgen deprivation induces bladder histological abnormalities and dysfunction via TGF-β in orchiectomized mature rats. Tohoku J Exp Med. 2012; 226:121–128. PMID: 22277325.115. Cayan F, Tek M, Balli E, Oztuna S, Karazindiyanoğlu S, Cayan S. The effect of testosterone alone and testosterone + estradiol therapy on bladder functions and smooth muscle/collagen content in surgically menopause induced rats. Maturitas. 2008; 60:248–252. PMID: 18774243.116. Saad F, Gooren LJ, Haider A, Yassin A. A dose-response study of testosterone on sexual dysfunction and features of the metabolic syndrome using testosterone gel and parenteral testosterone undecanoate. J Androl. 2008; 29:102–105. PMID: 17916569.
Article117. Heufelder AE, Saad F, Bunck MC, Gooren L. Fifty-two-week treatment with diet and exercise plus transdermal testosterone reverses the metabolic syndrome and improves glycemic control in men with newly diagnosed type 2 diabetes and subnormal plasma testosterone. J Androl. 2009; 30:726–733. PMID: 19578132.
Article118. Aversa A, Bruzziches R, Francomano D, Rosano G, Isidori AM, Lenzi A, et al. Effects of testosterone undecanoate on cardiovascular risk factors and atherosclerosis in middle-aged men with late-onset hypogonadism and metabolic syndrome: results from a 24-month, randomized, double-blind, placebo-controlled study. J Sex Med. 2010; 7:3495–3503. PMID: 20646185.
Article119. Haider A, Gooren LJ, Padungtod P, Saad F. Beneficial effects of 2 years of administration of parenteral testosterone undecanoate on the metabolic syndrome and on non-alcoholic liver steatosis and C-reactive protein. Horm Mol Biol Clin Investig. 2010; 1:27–33.
Article120. Kalinchenko SY, Tishova YA, Mskhalaya GJ, Gooren LJ, Giltay EJ, Saad F. Effects of testosterone supplementation on markers of the metabolic syndrome and inflammation in hypogonadal men with the metabolic syndrome: the double-blinded placebo-controlled Moscow study. Clin Endocrinol (Oxf). 2010; 73:602–612. PMID: 20718771.
Article121. Bhattacharya RK, Khera M, Blick G, Kushner H, Nguyen D, Miner MM. Effect of 12 months of testosterone replacement therapy on metabolic syndrome components in hypogonadal men: data from the Testim Registry in the US (TRiUS). BMC Endocr Disord. 2011; 11:18. PMID: 22044661.
Article122. Jeong SM, Ham BK, Park MG, Oh MM, Yoon DK, Kim JJ, et al. Effect of testosterone replacement treatment in testosterone deficiency syndrome patients with metabolic syndrome. Korean J Urol. 2011; 52:566–571. PMID: 21927705.
Article123. Jones TH, Arver S, Behre HM, Buvat J, Meuleman E, Moncada I, et al. Testosterone replacement in hypogonadal men with type 2 diabetes and/or metabolic syndrome (the TIMES2 study). Diabetes Care. 2011; 34:828–837. PMID: 21386088.
Article124. Hoyos CM, Yee BJ, Phillips CL, Machan EA, Grunstein RR, Liu PY. Body compositional and cardiometabolic effects of testosterone therapy in obese men with severe obstructive sleep apnoea: a randomised placebo-controlled trial. Eur J Endocrinol. 2012; 167:531–541. PMID: 22848006.
Article125. Stanworth RD, Akhtar S, Channer KS, Jones TH. The role of androgen receptor CAG repeat polymorphism and other factors which affect the clinical response to testosterone replacement in metabolic syndrome and type 2 diabetes: TIMES2 sub-study. Eur J Endocrinol. 2013; 170:193–200. PMID: 24165020.
Article126. Francomano D, Ilacqua A, Bruzziches R, Lenzi A, Aversa A. Effects of 5-year treatment with testosterone undecanoate on lower urinary tract symptoms in obese men with hypogonadism and metabolic syndrome. Urology. 2014; 83:167–173. PMID: 24139347.
Article127. Traish AM, Haider A, Doros G, Saad F. Long-term testosterone therapy in hypogonadal men ameliorates elements of the metabolic syndrome: an observational, long-term registry study. Int J Clin Pract. 2014; 68:314–329. PMID: 24127736.
Article128. Yassin DJ, El Douaihy Y, Yassin AA, Kashanian J, Shabsigh R, Hammerer PG. Lower urinary tract symptoms improve with testosterone replacement therapy in men with late-onset hypogonadism: 5-year prospective, observational and longitudinal registry study. World J Urol. 2014; 32:1049–1054. PMID: 24135918.
Article129. Shigehara K, Konaka H, Nohara T, Izumi K, Kitagawa Y, Kadono Y, et al. Effects of testosterone replacement therapy on metabolic syndrome among Japanese hypogonadal men: A subanalysis of a prospective randomised controlled trial (EARTH study). Andrologia. 2018; 50:[Epub]. DOI: 10.1111/and.12815.
Article130. Mårin P, Holmäng S, Gustafsson C, Jönsson L, Kvist H, Elander A, et al. Androgen treatment of abdominally obese men. Obes Res. 1993; 1:245–251. PMID: 16350577.
Article131. Kapoor D, Goodwin E, Channer KS, Jones TH. Testosterone replacement therapy improves insulin resistance, glycaemic control, visceral adiposity and hypercholesterolaemia in hypogonadal men with type 2 diabetes. Eur J Endocrinol. 2006; 154:899–906. PMID: 16728551.
Article132. Hackett G, Cole N, Bhartia M, Kennedy D, Raju J, Wilkinson P. Testosterone replacement therapy improves metabolic parameters in hypogonadal men with type 2 diabetes but not in men with coexisting depression: the BLAST study. J Sex Med. 2014; 11:840–856. PMID: 24308723.
Article133. Hoyos CM, Yee BJ, Phillips CL, Machan EA, Grunstein RR, Liu PY. Body compositional and cardiometabolic effects of testosterone therapy in obese men with severe obstructive sleep apnea: a randomized placebo-controlled trial. Eur J Endocrinol. 2015; 173:X3. PMID: 26516206.
Article134. Cai X, Tian Y, Wu T, Cao CX, Li H, Wang KJ. Metabolic effects of testosterone replacement therapy on hypogonadal men with type 2 diabetes mellitus: a systematic review and meta-analysis of randomized controlled trials. Asian J Androl. 2014; 16:146–152. PMID: 24369149.
Article135. Gianatti EJ, Dupuis P, Hoermann R, Strauss BJ, Wentworth JM, Zajac JD, et al. Effect of testosterone treatment on glucose metabolism in men with type 2 diabetes: a randomized controlled trial. Diabetes Care. 2014; 37:2098–2107. PMID: 24804695.
Article136. Haider A, Yassin A, Doros G, Saad F. Effects of long-term testosterone therapy on patients with “diabesity”: results of observational studies of pooled analyses in obese hypogonadal men with type 2 diabetes. Int J Endocrinol. 2014; [Epub]. DOI: 10.1155/2014/683515.
Article137. Traish AM. Testosterone and weight loss: the evidence. Curr Opin Endocrinol Diabetes Obes. 2014; 21:313–322. PMID: 25105998.138. Høst C, Gormsen LC, Hougaard DM, Christiansen JS, Pedersen SB, Gravholt CH. Acute and short-term chronic testosterone fluctuation effects on glucose homeostasis, insulin sensitivity, and adiponectin: a randomized, double-blind, placebo-controlled, crossover study. J Clin Endocrinol Metab. 2014; 99:E1088–E1096. PMID: 24606070.
Article139. Pitteloud N, Mootha VK, Dwyer AA, Hardin M, Lee H, Eriksson KF, et al. Relationship between testosterone levels, insulin sensitivity, and mitochondrial function in men. Diabetes Care. 2005; 28:1636–1642. PMID: 15983313.
Article140. Kalinchenko S, Vishnevskiy EL, Koval AN, Mskhalaya GJ, Saad F. Beneficial effects of testosterone administration on symptoms of the lower urinary tract in men with late-onset hypogonadism: a pilot study. Aging Male. 2008; 11:57–61. PMID: 18570056.
Article141. Karazindiyanoğlu S, Cayan S. The effect of testosterone therapy on lower urinary tract symptoms/bladder and sexual functions in men with symptomatic late-onset hypogonadism. Aging Male. 2008; 11:146–149. PMID: 18821291.142. Amano T, Imao T, Takemae K, Iwamoto T, Nakanome M. Testosterone replacement therapy by testosterone ointment relieves lower urinary tract symptoms in late onset hypogonadism patients. Aging Male. 2010; 13:242–246. PMID: 20795793.
Article143. Shigehara K, Konaka H, Koh E, Izumi K, Kitagawa Y, Mizokami A, et al. Effects of testosterone replacement therapy on nocturia and quality of life in men with hypogonadism: a subanalysis of a previous prospective randomized controlled study in Japan. Aging Male. 2015; 18:169–174. PMID: 26075538.
Article144. Permpongkosol S, Khupulsup K, Leelaphiwat S, Pavavattananusorn S, Thongpradit S, Petchthong T. Effects of 8-year treatment of long-acting testosterone undecanoate on metabolic parameters, urinary symptoms, bone mineral density, and sexual function in men with late-onset hypogonadism. J Sex Med. 2016; 13:1199–1211. PMID: 27436076.
Article145. Yassin A, Nettleship JE, Talib RA, Almehmadi Y, Doros G. Effects of testosterone replacement therapy withdrawal and re-treatment in hypogonadal elderly men upon obesity, voiding function and prostate safety parameters. Aging Male. 2016; 19:64–69. PMID: 26742589.
Article146. Koritsiadis G, Stravodimos K, Mitropoulos D, Doumanis G, Fokitis I, Koritsiadis S, et al. Androgens and bladder outlet obstruction: a correlation with pressure-flow variables in a preliminary study. BJU Int. 2008; 101:1542–1546. PMID: 18294304.
Article147. Traish AM, Park K, Dhir V, Kim NN, Moreland RB, Goldstein I. Effects of castration and androgen replacement on erectile function in a rabbit model. Endocrinology. 1999; 140:1861–1868. PMID: 10098525.148. Crawford ED, Poage W, Nyhuis A, Price DA, Dowsett SA, Muram D. Effects of testosterone level on lower urinary tract symptoms. Am J Mens Health. 2016; 10:440–442. PMID: 26077271.
Article149. Morgentaler A, Traish AM. Shifting the paradigm of testosterone and prostate cancer: the saturation model and the limits of androgen-dependent growth. Eur Urol. 2009; 55:310–320. PMID: 18838208.
Article150. Baas W, Köhler TS. Testosterone replacement therapy and voiding dysfunction. Transl Androl Urol. 2016; 5:890–897. PMID: 28078221.
Article151. Traish AM, Haider A, Haider KS, Doros G, Saad F. Long-term testosterone therapy improves cardiometabolic function and reduces risk of cardiovascular disease in men with hypogonadism: a real-life observational registry study setting comparing treated and untreated (control) groups. J Cardiovasc Pharmacol Ther. 2017; 22:414–433. PMID: 28421834.152. Debruyne FM, Behre HM, Roehrborn CG, Maggi M, Wu FC, Schröder FH, et al. Testosterone treatment is not associated with increased risk of prostate cancer or worsening of lower urinary tract symptoms: prostate health outcomes in the Registry of Hypogonadism in Men. BJU Int. 2017; 119:216–224. PMID: 27409523.
Article153. Kim JW, Oh MM, Yoon CY, Bae JH, Kim JJ, Moon du G. Nocturnal polyuria and decreased serum testosterone: is there an association in men with lower urinary tract symptoms? Int J Urol. 2014; 21:518–523. PMID: 24286364.
Article154. Björntorp P, Rosmond R. The metabolic syndrome: a neuroendocrine disorder? Br J Nutr. 2000; 83(Suppl 1):S49–S57. PMID: 10889792.155. Rosmond R, Dallman MF, Björntorp P. Stress-related cortisol secretion in men: relationships with abdominal obesity and endocrine, metabolic and hemodynamic abnormalities. J Clin Endocrinol Metab. 1998; 83:1853–1859. PMID: 9626108.
Article156. Teoh H, Verma S. C-reactive protein, metabolic syndrome, and end organ damage. Metabolism. 2007; 56:1620–1622. PMID: 17998011.
Article157. Liu HY, Chung MS, Wang HJ, Liu RT, Chuang YC. Nocturia indicates a poor health status and increases mortality in male patients with type 2 diabetes mellitus. Int Urol Nephrol. 2016; 48:1209–1214. PMID: 27156073.
Article158. Kohn TP, Mata DA, Ramasamy R, Lipshultz LI. Effects of testosterone replacement therapy on lower urinary tract symptoms: a systematic review and meta-analysis. Eur Urol. 2016; 69:1083–1090. PMID: 26874809.
Article159. Lorenzetti F, Pintarelli VL, Seraphim DC, Dambros M. Low testosterone levels induce apoptosis via active 3-caspase dependent signaling in the bladder wall of male rats. Aging Male. 2012; 15:216–219. PMID: 22967305.
Article160. Gallo CB, Miranda AF, Felix-Patricio B, Ramos CF, Cardoso LE, Costa WS, et al. Effects of castration and hormone replacement in the urinary bladder of rats: structural, ultrastructural, and biochemical analysis. J Androl. 2012; 33:684–690. PMID: 22052775.
Article161. Yassin AA, El-Sakka AI, Saad F, Gooren LJ. Lower urinary-tract symptoms and testosterone in elderly men. World J Urol. 2008; 26:359–364. PMID: 18594831.
Article162. Morelli A, Comeglio P, Filippi S, Sarchielli E, Cellai I, Vignozzi L, et al. Testosterone and farnesoid X receptor agonist INT-747 counteract high fat diet-induced bladder alterations in a rabbit model of metabolic syndrome. J Steroid Biochem Mol Biol. 2012; 132:80–92. PMID: 22406511.
Article163. Kirby MG, Wagg A, Cardozo L, Chapple C, Castro-Diaz D, de Ridder D, et al. Overactive bladder: is there a link to the metabolic syndrome in men? Neurourol Urodyn. 2010; 29:1360–1364. PMID: 20589717.
Article164. Temml C, Obermayr R, Marszalek M, Rauchenwald M, Madersbacher S, Ponholzer A. Are lower urinary tract symptoms influenced by metabolic syndrome? Urology. 2009; 73:544–548. PMID: 19118873.
Article165. Yeh HC, Liu CC, Lee YC, Wu WJ, Li WM, Li CC, et al. Associations of the lower urinary tract symptoms with the lifestyle, prostate volume, and metabolic syndrome in the elderly males. Aging Male. 2012; 15:166–172. PMID: 22452270.
Article166. Ohgaki K, Hikima N, Horiuchi K, Kondo Y. Association between metabolic syndrome and male lower urinary tract symptoms in Japanese subjects using three sets of criteria for metabolic syndrome and International Prostate Symptom Score. Urology. 2011; 77:1432–1438. PMID: 21316081.
Article167. Cohen PG. Abdominal obesity and intra-abdominal pressure: a new paradigm for the pathogenesis of the hypogonadal-obesity-BPH-LUTS connection. Horm Mol Biol Clin Investig. 2012; 11:317–320.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Testosterone Deficiency and Nocturia: A Review
- Late Onset Hypogonadism and Lower Urinary Tract Symptoms: New Insights
- Correlation Between Testosterone Replacement Treatment and Lower Urinary Tract Symptoms
- Testosterone and metabolic syndrome in men
- Testosterone therapy in men with testosterone deficiency: Are we beyond the point of no return?