Investig Clin Urol.
2016 Nov;57(6):384-400. 10.4111/icu.2016.57.6.384.
Testosterone therapy in men with testosterone deficiency: Are we beyond the point of no return?
- Affiliations
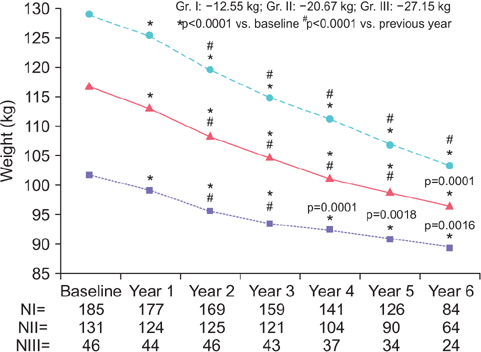
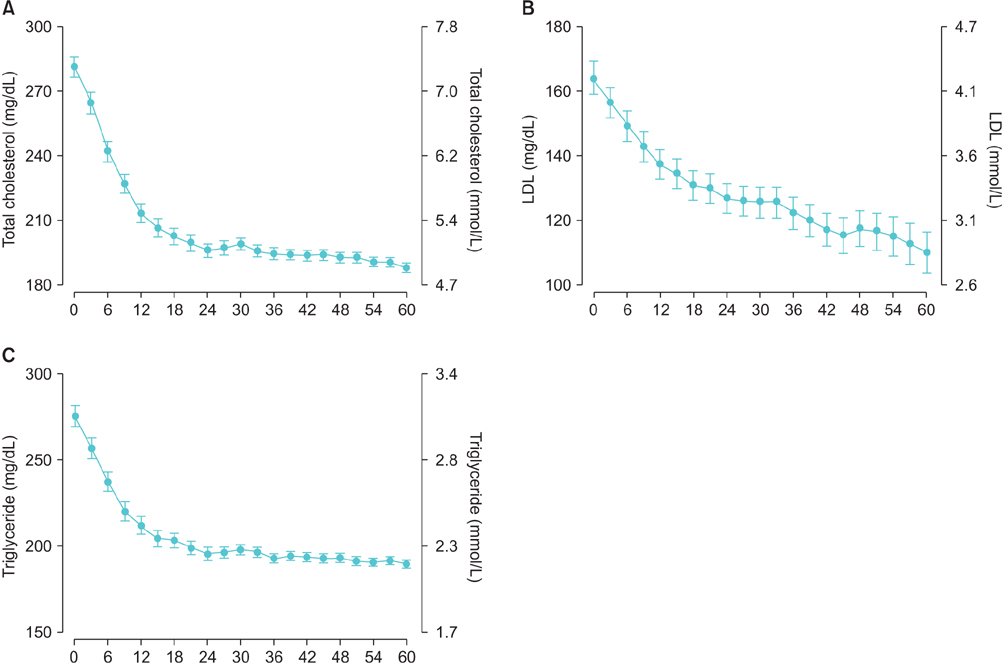
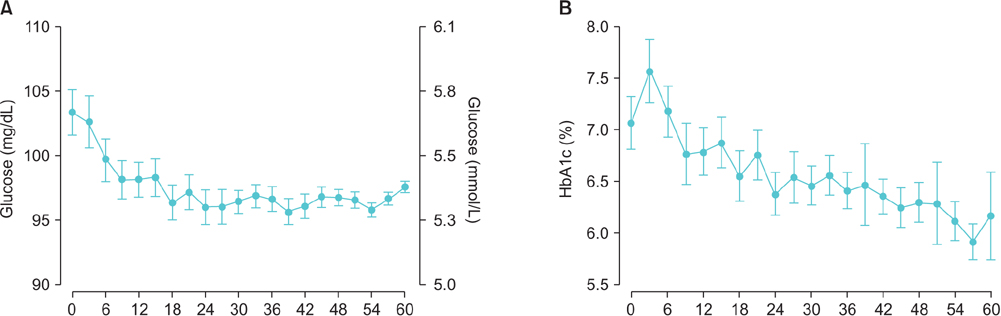
-
- 1Departments of Biochemistry and Urology, Boston University School of Medicine, Boston, MA, USA. atraish@bu.edu
- KMID: 2451397
- DOI: http://doi.org/10.4111/icu.2016.57.6.384
Abstract
- Although testosterone therapy in men with testosterone deficiency was introduced in the early 1940s, utilization of this effective treatment approach in hypogonadal men is met with considerable skepticism and resistance. Indeed, for decades, the fear that testosterone may cause prostate cancer has hampered clinical progress in this field. Nevertheless, even after considerable knowledge was acquired that this fear is unsubstantiated, many in the medical community remain hesitant to utilize this therapeutic approach to treat men with hypogonadism. As the fears concerning prostate cancer have subsided, a new controversy regarding use of testosterone therapy and increase in cardiovascular disease was introduced. Although the new controversy was based on one ill-fated clinical trial, one meta-analysis with studies that utilized unapproved formulation in men with liver cirrhosis, and two retrospective studies with suspect or nonvalidated statistical methodologies and database contaminations, the flames of such controversy were fanned by the lay press and academics alike. In this review we discuss the adverse effect of testosterone deficiency and highlight the numerous proven benefits of testosterone therapy on men's health and debunk the myth that testosterone therapy increases cardiovascular risk. Ultimately, we believe that there is considerable scientific and clinical evidence to suggest that testosterone therapy is safe and effective with restoration of physiological levels in men with testosterone deficiency, irrespective of its etiology.
MeSH Terms
Figure
Reference
-
1. Morgentaler A, Miner MM, Caliber M, Guay AT, Khera M, Traish AM. Testosterone therapy and cardiovascular risk: advances and controversies. Mayo Clin Proc. 2015; 90:224–251.2. Morgentaler A, Zitzmann M, Traish A, Fox AW, Jones T. Hugh, et al. International expert consensus conference on testosterone deficiency and its treatment- resolutions and conclusions. Mayo Clin Proc. 2016; 91:881–896.3. Snyder PJ, Bhasin S, Cunningham GR, Matsumoto AM, Stephens-Shields AJ, Cauley JA, et al. Effects of testosterone treatment in older men. N Engl J Med. 2016; 374:611–624.4. Traish AM, Haider A, Doros G, Saad F. Long-term testosterone therapy in hypogonadal men ameliorates elements of the metabolic syndrome: an observational, long-term registry study. Int J Clin Pract. 2014; 68:314–329.5. Traish AM. Testosterone therapy in men with testosterone deficiency: are the benefits and cardiovascular risks real or imagined? Am J Physiol Regul Integr Comp Physiol. 2016; 311:R566–R573.6. Kelly DM, Jones TH. Testosterone: a vascular hormone in health and disease. J Endocrinol. 2013; 217:R47–R71.7. Kelly DM, Jones TH. Testosterone: a metabolic hormone in health and disease. J Endocrinol. 2013; 217:R25–R45.8. Saad F, Yassin A, Doros G, Haider A. Effects of long-term treatment with testosterone on weight and waist size in 411 hypogonadal men with obesity classes I-III: observational data from two registry studies. Int J Obes (Lond). 2016; 40:162–170.9. Anderson JL, May HT, Lapp in. testosterone replacement therapy on myocardial infarction, stroke, and death in men with low testosterone concentrations in an integrated health care system. Am J Cardiol. 2016; 117:794–799.10. Sharma R, Oni OA, Gupta K, Chen G, Sharma M, Dawn B, et al. Normalization of testosterone level is associated with reduced incidence of myocardial infarction and mortality in men. Eur Heart J. 2015; 36:2706–2715.11. Sharma R, Oni OA, Chen G, Sharma M, Dawn B, Sharma R, et al. Association between testosterone replacement therapy and the incidence of DVT and Pulmonary embolism: a retrospective cohort study of the veterans administration database. Chest. 2016; 150:563–571.12. Wallis CJ, Lo K, Lee Y, Krakowsky Y, Garbens A, Satkunasivam R, et al. Survival and cardiovascular events in men treated with testosterone replacement therapy: an intention-to-treat observational cohort study. Lancet Diabetes Endocrinol. 2016; 4:498–506.13. Etminan M, Skeldon SC, Goldenberg SL, Carleton B, Brophy JM. Testosterone therapy and risk of myocardial infarction: a pharmacoepidemiologic study. Pharmacotherapy. 2015; 35:72–78.14. Baillargeon J, Urban RJ, Kuo YF, Ottenbacher KJ, Raji MA, Du F, et al. Risk of myocardial infarction in older men receiving testosterone therapy. Ann Pharmacother. 2014; 48:1138–1144.15. Baillargeon J, Urban RJ, Morgentaler A, Glueck CJ, Baillargeon G, Sharma G, et al. Risk of venous thromboembolism in men receiving testosterone therapy. Mayo Clin Proc. 2015; 90:1038–1045.16. Aub JC, Kety SS. Recent advances in testosterone therapy. N Engl J Med. 1943; 228:338–343.17. Beaser SB, Massell TB. Therapeutic evaluation of testosterone in peripheral vascular disease. N Engl J Med. 1942; 227:43–44.18. Lesser MA. Testosterone propionate therapy in one hundred cases of angina pectoris. J Clin Endocrinol Metab. 1946; 6:549–557.19. Morgentaler A. Testosterone therapy can be given to men with no concern that it will promote prostate cancer development or progression: pro. J Urol. 2016; 196:985–988.20. Huggins C, Hodges CV. Studies on prostatic cancer. I. The effect of castration, of estrogen and androgen injection on serum phosphatases in metastatic carcinoma of the prostate. CA Cancer J Clin. 1972; 22:232–240.21. Gleave ME, Klotz L. Testosterone therapy can be given to men with no concern that it will promote prostate cancer development or progression: con. J Urol. 2016; 196:985–988.22. Basaria S, Coviello AD, Travison TG, Storer TW, Farwell WR, Jette AM, et al. Adverse events associated with testosterone administration. N Engl J Med. 2010; 363:109–122.23. Xu L, Freeman G, Cowling BJ, Schooling CM. Testosterone therapy and cardiovascular events among men: a systematic review and meta-analysis of placebo-controlled randomized trials. BMC Med. 2013; 11:108.24. Vigen R, O'Donnell CI, Barón AE, Grunwald GK, Maddox TM, Bradley SM, et al. Association of testosterone therapy with mortality, myocardial infarction, and stroke in men with low testosterone levels. JAMA. 2013; 310:1829–1836.25. Finkle WD, Greenland S, Ridgeway GK, Adams JL, Frasco MA, Cook MB, et al. Increased risk of non-fatal myocardial infarction following testosterone therapy prescription in men. PLoS One. 2014; 9:e85805.26. Perls T, Handelsman DJ. Disease mongering of age-associated declines in testosterone and growth hormone levels. J Am Geriatr Soc. 2015; 63:809–811.27. The Editorial Board. Overselling testosterone, dangerously [internet]. The New York Times;2014. 02. 04. cited 2014 Feb 5. Opinion page. Available from: http://www.nytimes.com/2014/02/05/opinion/overselling-testosterone-dangerously.html.28. Wolfe S, Carome M. Petition to the FDA on all testosterone products [Internet]. Public Citizen;2014. cited 2014 Feb 25. Available from: http://www.citizen.org/documents/2184.pdf.29. Woodcock. Citizen petition denial response from FDA CDER to public citizen [Internet]. Silber Spring (MD): U.S. Food and Drug Administration;2014. cited 2014 Aug 31. Available from: http://www.citizen.org/documents/2020_FDA%20Final%20Response%20to%20Petition.pdf.30. Quick study: testosterone supplement may have cardiovascular risks for older men [Internet]. The Washington Post;2010. 07. 13. cited 2016 Jul 15. Available from: http://www.washingtonpost.com/wp-dyn/content/article/2010/07/12/AR2010071204179.html.31. Testosterone treatments linked to heart risks [Internet]. USA TODAY;2013. 11. 05. cited 2014 Jan 29. Available from: http://www.usatoday.com/story/news/nation/2013/11/05/testosterone-heart-attacks/3448543/.32. Singer N. Selling that new-man feeling [Internet]. The New York Times;2013. 11. 23. cited 2016 Jul 15. Available from: http://www.nytimes.com/2013/11/24/business/selling-that-new-man-feeling.html.33. Silverman E. Doctors try to influence a medical journal poll on testosterone treatments [Internet]. The Wall Street Journal;2014. 12. 02. cited 2014 Dec 2. Available from: http://blogs.wsj.com/pharmalot/2014/12/02/doctors-try-to-influence-a-medical-journal-poll-on-testerone-treatments/.34. Beck M. In men's fight against aging, how much risk to take? The FDA is weighing whether testosterone-replacement therapy is safe. [Internet]. The Wall Street Journal;2014. 10. 27. cited 2014 Oct 27. Available from: http://www.wsj.com/articles/in-mens-fight-against-aging-how-much-risk-to-take-1414443065.35. Sifferlin A. Low-T drugs and heart risk: here's the latest [Internet]. Time;2015. 08. 11. cited 2015 Aug 11. Available from: http://time.com/3992444/testosterone-heart-disease/.36. Lester M. Are you man enough? the truth about low testosterone. Time;2014. 07. 31. cited 2016 Jul 15. Available from: http://time.com/3063213/low-testosterone/.37. Endocrine Society. Too many men take testosterone when they don't need it [Internet]. The Washington Post;2014. 01. 13. cited 2014 Jan 13. Available from: https://www.washingtonpost.com/national/health-science/too-many-men-take-testosterone-when-they-dont-need-it/2014/01/13/d2ecc700-7956-11e3-af7f-13bf0e9965f6_story.html.38. Glueck CJ, Wang P. Testosterone therapy, thrombosis, thrombophilia, cardiovascular events. Metabolism. 2014; 63:989–994.39. Nguyen CP, Hirsch MS, Moeny D, Kaul S, Mohamoud M, Joffe HV. Testosterone and "Age-Related Hypogonadism"--FDA Concerns. N Engl J Med. 2015; 373:689–691.40. Antonio L, Wu FC, O'Neill TW, Pye SR, Carter EL, Finn JD, et al. Associations between sex steroids and the development of metabolic syndrome: a longitudinal study in European men. J Clin Endocrinol Metab. 2015; 100:1396–1404.41. Traish AM, Zitzmann M. The complex and multifactorial relationship between testosterone deficiency (TD), obesity and vascular disease. Rev Endocr Metab Disord. 2015; 16:249–268.42. O'Connell MD, Tajar A, Roberts SA, Wu FC. Do androgens play any role in the physical frailty of ageing men? Int J Androl. 2011; 34:195–211.43. Albert SG, Morley JE. Testosterone therapy, association with age, initiation and mode of therapy with cardiovascular events: a systematic review. Clin Endocrinol (Oxf). 2016; 85:436–443.44. Corona G, Giagulli VA, Maseroli E, Vignozzi L, Aversa A, Zitzmann M, et al. Testosterone supplementation and body composition: results from a meta-analysis of observational studies. J Endocrinol Invest. 2016; 39:967–981.45. Aversa A, Bruzziches R, Francomano D, Rosano G, Isidori AM, Lenzi A, et al. Effects of testosterone undecanoate on cardiovascular risk factors and atherosclerosis in middle-aged men with late-onset hypogonadism and metabolic syndrome: results from a 24-month, randomized, double-blind, placebocontrolled study. J Sex Med. 2010; 7:3495–3503.46. Traish AM, Park K, Dhir V, Kim NN, Moreland RB, Goldstein I. Effects of castration and androgen replacement on erectile function in a rabbit model. Endocrinology. 1999; 140:1861–1868.47. Brock G, Heiselman D, Maggi M, Kim SW, Rodr SW, Rodr SW, et al. Effect of testosterone solution 2% on testosterone concentration, sex drive and energy in hypogonadal men: results of a placebo controlled study. J Urol. 2016; 195:699–705.48. Finkelstein JS, Lee H, Burnett-Bowie SA, Pallais JC, Yu EW, Borges LF, et al. Gonadal steroids and body composition, strength, and sexual function in men. N Engl J Med. 2013; 369:1011–1022.49. Traish AM. Testosterone and weight loss: the evidence. Curr Opin Endocrinol Diabetes Obes. 2014; 21:313–322.50. Page ST, Amory JK, Bowman FD, Anawalt BD, Matsumoto AM, Bremner WJ, et al. Exogenous testosterone (T) alone or with finasteride increases physical performance, grip strength, and lean body mass in older men with low serum T. J Clin Endocrinol Metab. 2005; 90:1502–1510.51. Morley JE. Pharmacologic options for the treatment of sarcopenia. Calcif Tissue Int. 2016; 98:319–333.52. Svartberg J, Agledahl I, Figenschau Y, Sildnes T, Waterloo K, Jorde R. Testosterone treatment in elderly men with subnormal testosterone levels improves body composition and BMD in the hip. Int J Impot Res. 2008; 20:378–387.53. Singh R, Artaza JN, Taylor WE, Braga M, Yuan X, Gonzalez-Cadavid NF, et al. Testosterone inhibits adipogenic differentiation in 3T3-L1 cells: nuclear translocation of androgen receptor complex with beta-catenin and T-cell factor 4 may bypass canonical Wnt signaling to down-regulate adipogenic transcription factors. Endocrinology. 2006; 147:141–154.54. Francomano D, Bruzziches R, Barbaro G, Lenzi A, Aversa A. Effects of testosterone undecanoate replacement and withdrawal on cardio-metabolic, hormonal and body composition outcomes in severely obese hypogonadal men: a pilot study. J Endocrinol Invest. 2014; 37:401–411.55. Amanatkar HR, Chibnall JT, Seo BW, Manepalli JN, Grossberg GT. Impact of exogenous testosterone on mood: a systematic review and meta-analysis of randomized placebo-controlled trials. Ann Clin Psychiatry. 2014; 26:19–32.56. Wang C, Cunningham G, Dobs A, Iranmanesh A, Matsumoto AM, Snyder PJ, et al. Long-term testosterone gel (AndroGel) treatment maintains beneficial effects on sexual function and mood, lean and fat mass, and bone mineral density in hypogonadal men. J Clin Endocrinol Metab. 2004; 89:2085–2098.57. Pexman-Fieth C, Behre HM, Morales A, Kan-Dobrosky N, Miller MG. A 6-month observational study of energy, sexual desire, and body proportions in hypogonadal men treated with a testosterone 1% gel. Aging Male. 2014; 17:1–11.58. Khera M, Bhattacharya RK, Blick G, Kushner H, Nguyen D, Miner MM. The effect of testosterone supplementation on depression symptoms in hypogonadal men from the Testim Registry in the US (TRiUS). Aging Male. 2012; 15:14–21.59. Kim C, Barrett-Connor E, Aroda VR, Mather KJ, Christophi CA, Horton ES, et al. Testosterone and depressive symptoms among men in the Diabetes Prevention Program. Psychoneuroendocrinology. 2016; 72:63–71.60. Westley CJ, Amdur RL, Irwig MS. High rates of depression and depressive symptoms among men referred for borderline testosterone levels. J Sex Med. 2015; 12:1753–1760.61. Wahjoepramono EJ, Asih PR, Aniwiyanti V, Taddei K, Dhaliwal SS, Fuller SJ, et al. The effects of testosterone supplementation on cognitive functioning in older men. CNS Neurol Disord Drug Targets. 2016; 15:337–343.62. Vignozzi L, Morelli A, Sarchielli E, Comeglio P, Filippi S, Cellai I, et al. Testosterone protects from metabolic syndrome-associated prostate inflammation: an experimental study in rabbit. J Endocrinol. 2012; 212:71–84.63. Kathrins M, Doersch K, Nimeh T, Canto A, Niederberger C, Seftel A. The relationship between testosterone-replacement therapy and lower urinary tract symptoms: a systematic review. Urology. 2016; 88:22–32.64. Meuleman EJ, Legros JJ, Bouloux PM, Johnson-Levonas AO, Kaspers MJ, Elbers JM, et al. Effects of long-term oral testosterone undecanoate therapy on urinary symptoms: data from a 1-year, placebo-controlled, dose-ranging trial in aging men with symptomatic hypogonadism. Aging Male. 2015; 18:157–163.65. Debruyne FM, Behre HM, Roehrborn CG, Maggi M, Wu FC, Schr Mag FH, et al. Testosterone treatment is not associated with increased risk of prostate cancer or worsening of lower urinary tract symptoms: prostate health outcomes in the Registry of Hypogonadism in Men. BJU Int. 2016; 07. 13. [Epub]. DOI: 10.1111/bju.13578.66. Kohn TP, Mata DA, Ramasamy R, Lipshultz LI. Effects of testosterone replacement therapy on lower urinary tract symptoms: a systematic review and meta-analysis. Eur Urol. 2016; 69:1083–1090.67. Shigehara K, Sugimoto K, Konaka H, Iijima M, Fukushima M, Maeda Y, et al. Androgen replacement therapy contributes to improving lower urinary tract symptoms in patients with hypogonadism and benign prostate hypertrophy: a randomised controlled study. Aging Male. 2011; 14:53–58.68. Ko YH, Moon du G, Moon KH. Testosterone replacement alone for testosterone deficiency syndrome improves moderate lower urinary tract symptoms: one year follow-up. World J Mens Health. 2013; 31:47–52.69. Okada K, Miyake H, Ishida T, Sumii K, Enatsu N, Chiba K, et al. Improved lower urinary tract symptoms associated with testosterone replacement therapy in japanese men with lateonset hypogonadism. Am J Mens Health. 2016; 06. 02. [Epub]. DOI: 10.1177/1557988316652843.70. Tomlinson BE, Irving D. The numbers of limb motor neurons in the human lumbosacral cord throughout life. J Neurol Sci. 1977; 34:213–219.71. Bhasin S. Testosterone supplementation for aging-associated sarcopenia. J Gerontol A Biol Sci Med Sci. 2003; 58:1002–1008.72. von Haehling S, Morley JE, Anker SD. From muscle wasting to sarcopenia and myopenia: update 2012. J Cachexia Sarcopenia Muscle. 2012; 3:213–217.73. Snyder PJ, Peachey H, Hannoush P, Berlin JA, Loh L, Holmes JH, et al. Effect of testosterone treatment on bone mineral density in men over 65 years of age. J Clin Endocrinol Metab. 1999; 84:1966–1972.74. Kenny AM, Kleppinger A, Annis K, Rathier M, Browner B, Judge JO, et al. Effects of transdermal testosterone on bone and muscle in older men with low bioavailable testosterone levels, low bone mass, and physical frailty. J Am Geriatr Soc. 2010; 58:1134–1143.75. Ferrando AA, Sheffield-Moore M, Yeckel CW, Gilkison C, Jiang J, Achacosa A, et al. Testosterone administration to older men improves muscle function: molecular and physiological mechanisms. Am J Physiol Endocrinol Metab. 2002; 282:E601–E607.76. Srinivas-Shankar U, Roberts SA, Connolly MJ, O'Connell MD, Adams JE, Oldham JA, et al. Effects of testosterone on muscle strength, physical function, body composition, and quality of life in intermediate-frail and frail elderly men: a randomized, double-blind, placebo-controlled study. J Clin Endocrinol Metab. 2010; 95:639–650.77. Caminiti G, Volterrani M, Iellamo F, Marazzi G, Massaro R, Miceli M, et al. Effect of long-acting testosterone treatment on functional exercise capacity, skeletal muscle performance, insulin resistance, and baroreflex sensitivity in elderly patients with chronic heart failure a double-blind, placebo-controlled, randomized study. J Am Coll Cardiol. 2009; 54:919–927.78. Sinclair M, Grossmann M, Hoermann R, Angus PW, Gow PJ. Testosterone therapy increases muscle mass in men with cirrhosis and low testosterone: a randomised controlled trial. J Hepatol. 2016; 65:906–913. DOI: 10.1016/j.jhep.2016.06.007.79. Bhasin S, Woodhouse L, Casaburi R, Singh AB, Mac RP, Lee M, et al. Older men are as responsive as young men to the anabolic effects of graded doses of testosterone on the skeletal muscle. J Clin Endocrinol Metab. 2005; 90:678–688.80. Eichholzer M, Barbir A, Basaria S, Dobs AS, Feinleib M, Guallar E, et al. Serum sex steroid hormones and frailty in older American men of the Third National Health and Nutrition Examination Survey (NHANES III). Aging Male. 2012; 15:208–215.81. Mohr BA, Bhasin S, Kupelian V, Araujo AB, O'Donnell AB, McKinlay JB. Testosterone, sex hormone-binding globulin, and frailty in older men. J Am Geriatr Soc. 2007; 55:548–555.82. Hyde Z, Flicker L, Almeida OP, Hankey GJ, McCaul KA, Chubb SA, et al. Low free testosterone predicts frailty in older men: the health in men study. J Clin Endocrinol Metab. 2010; 95:3165–3172.83. Tajar A, O'Connell MD, Mitnitski AB, O'Neill TW, Searle SD, Huhtaniemi IT, et al. Frailty in relation to variations in hormone levels of the hypothalamic-pituitary-testicular axis in older men: results from the European male aging study. J Am Geriatr Soc. 2011; 59:814–821.84. Araujo AB, Dixon JM, Suarez EA, Murad MH, Guey LT, Wittert GA. Clinical review: Endogenous testosterone and mortality in men: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2011; 96:3007–3019.85. Yeap BB, Alfonso H, Chubb SA, Handelsman DJ, Hankey GJ, Almeida OP, et al. In older men an optimal plasma testosterone is associated with reduced all-cause mortality and higher dihydrotestosterone with reduced ischemic heart disease mortality, while estradiol levels do not predict mortality. J Clin Endocrinol Metab. 2014; 99:E9–E18.86. Khera M. Male hormones and men's quality of life. Curr Opin Urol. 2016; 26:152–157.87. Nian Y, Ding M, Hu S, He H, Cheng S, Yi L, et al. Testosterone replacement therapy improves health-related quality of life for patients with late-onset hypogonadism: a meta-analysis of randomized controlled trials. Andrologia. 2016; 07. 08. [Epub]. DOI: 10.1111/and.12630/abstract;jsessionid=A784F440904F991C3EFA21E5E0DDD560.f02t02.88. Cohen A, Lapin B, Wang CH, Helfand B, Victorson D, Novakovic K. Variation in testosterone levels and health-related quality of life in men diagnosed with prostate cancer on active surveillance. Urology. 2016; 94:180–187.89. Brooke JC, Walter DJ, Kapoor D, Marsh H, Muraleedharan V, Jones TH. Testosterone deficiency and severity of erectile dysfunction are independently associated with reduced quality of life in men with type 2 diabetes. Andrology. 2014; 2:205–211.90. Simanainen U, Allan CM, Lim P, McPherson S, Jimenez M, Zajac JD, et al. Disruption of prostate epithelial androgen receptor impedes prostate lobe-specific growth and function. Endocrinology. 2007; 148:2264–2272.91. Endogenous Hormones and Prostate Cancer Collaborative Group. Roddam AW, Allen NE, Appleby P, Key TJ. Endogenous sex hormones and prostate cancer: a collaborative analysis of 18 prospective studies. J Natl Cancer Inst. 2008; 100:170–183.92. Baillargeon J, Kuo YF, Fang X, Shahinian VB. Long-term exposure to testosterone therapy and the risk of high grade prostate cancer. J Urol. 2015; 194:1612–1616.93. Haider A, Zitzmann M, Doros G, Isbarn H, Hammerer P, Yassin A. Incidence of prostate cancer in hypogonadal men receiving testosterone therapy: observations from 5-year median followup of 3 registries. J Urol. 2015; 193:80–86.94. Prehn RT. On the prevention and therapy of prostate cancer by androgen administration. Cancer Res. 1999; 59:4161–4164.95. Wu CT, Altuwaijri S, Ricke WA, Huang SP, Yeh S, Zhang C, et al. Increased prostate cell proliferation and loss of cell differentiation in mice lacking prostate epithelial androgen receptor. Proc Natl Acad Sci U S A. 2007; 104:12679–12684.96. Niu Y, Altuwaijri S, Lai KP, Wu CT, Ricke WA, Messing EM, et al. Androgen receptor is a tumor suppressor and proliferator in prostate cancer. Proc Natl Acad Sci U S A. 2008; 105:12182–12187.97. Bonaccorsi L, Muratori M, Carloni V, Marchiani S, Formigli L, Forti G, et al. The androgen receptor associates with the epidermal growth factor receptor in androgen-sensitive prostate cancer cells. Steroids. 2004; 69:549–552.98. Leotoing L, Manin M, MontM D, Baron S, Communal Y, Lours C, et al. Crosstalk between androgen receptor and epidermal growth factor receptor-signalling pathways: a molecular switch for epithelial cell differentiation. J Mol Endocrinol. 2007; 39:151–162.99. Fugh-Berman A. Should family physicians screen for testosterone deficiency in men? No: screening may be harmful, and benefits are unproven. Am Fam Physician. 2015; 91:226–228.100. Kloner RA. Testosterone replacement therapy: new data on efficacy and cardiovascular safety. J Cardiovasc Pharmacol Ther. 2016; 04. 28. [Epub]. DOI: 10.1177/1074248416646938.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Erratum: Correction of the references for Figures. Testosterone therapy in men with testosterone deficiency: Are we beyond the point of no return?
- Book Review: Androgen Deficiency and Testosterone Replacement: Current Controversies and Strategies
- Testosterone Replacement Therapy and Prostate Cancer Incidence
- Testosterone Deficiency Associated with Poor Glycemic Control in Korean Male Diabetics
- Testosterone Deficiency and Nocturia: A Review