Yonsei Med J.
2017 Jul;58(4):891-893. 10.3349/ymj.2017.58.4.891.
Protein-Losing Enteropathy as a Complication of the Ketogenic Diet
- Affiliations
-
- 1Division of Pediatric Neurology, Department of Pediatrics, Severance Children's Hospital, Yonsei University College of Medicine, Seoul, Korea. hdkimmd@yuhs.ac
- 2Department of Pediatrics, College of Medicine, Soonchunhyang University, Bucheon Hospital, Bucheon, Korea.
- KMID: 2419101
- DOI: http://doi.org/10.3349/ymj.2017.58.4.891
Abstract
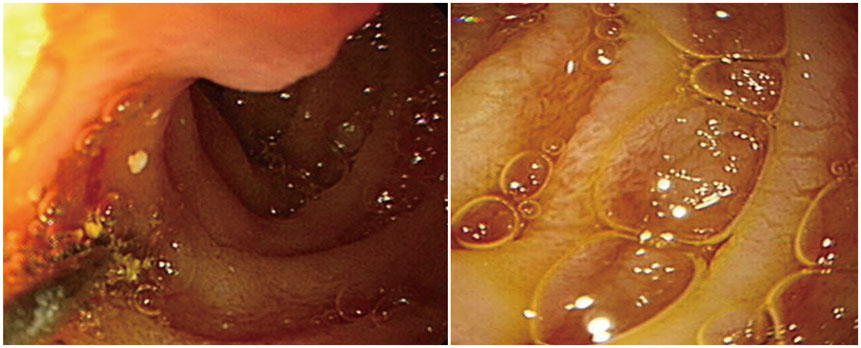
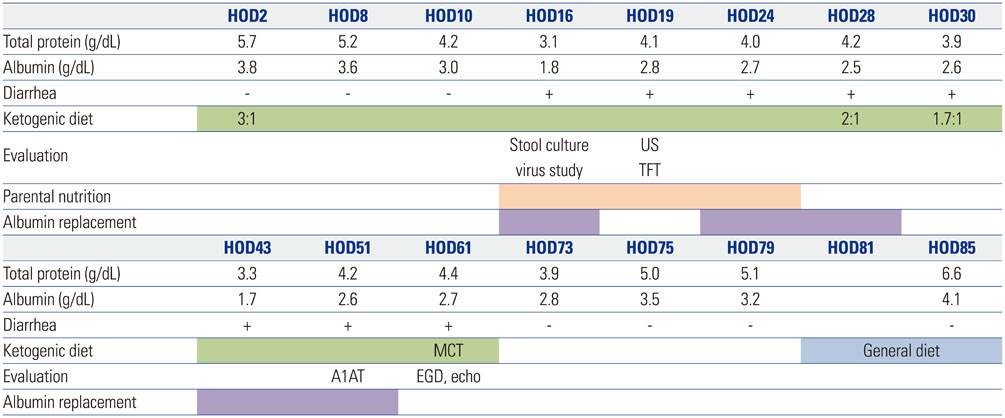
- The ketogenic diet is an effective treatment for the patients with intractable epilepsy, however, the diet therapy can sometimes be discontinued by complications. Protein-losing enteropathy is a rarely reported serious complication of the ketogenic diet. We present a 16-month-old Down syndrome baby with protein-losing enteropathy during the ketogenic diet as a treatment for West syndrome. He suffered from diarrhea, general edema and hypoalbuminemia which were not controlled by conservative care for over 1 month. Esophagogastroduodenoscopy and stool alpha-1 antitrypsin indicated protein-losing enteropathy. Related symptoms were relieved after cessation of the ketogenic diet. Unexplained hypoalbuminemia combined with edema and diarrhea during ketogenic suggests the possibility of protein-losing enteropathy, and proper evaluation is recommended in order to expeditiously detect it and to act accordingly.
MeSH Terms
Figure
Reference
-
1. DiMario FJ Jr, Holland J. The ketogenic diet: a review of the experience at Connecticut Children's Medical Center. Pediatr Neurol. 2002; 26:288–292.
Article2. Kang HC, Kim YJ, Kim DW, Kim HD. Efficacy and safety of the ketogenic diet for intractable childhood epilepsy: Korean multicentric experience. Epilepsia. 2005; 46:272–279.
Article3. Suo C, Liao J, Lu X, Fang K, Hu Y, Chen L, et al. Efficacy and safety of the ketogenic diet in Chinese children. Seizure. 2013; 22:174–178.
Article4. Kang HC, Chung DE, Kim DW, Kim HD. Early- and late-onset complications of the ketogenic diet for intractable epilepsy. Epilepsia. 2004; 45:1116–1123.
Article5. Moriyama K, Watanabe M, Yamada Y, Shiihara T. Protein-losing enteropathy as a rare complication of the ketogenic diet. Pediatr Neurol. 2015; 52:526–528.
Article6. Ballaban-Gil K, Callahan C, O'Dell C, Pappo M, Moshé S, Shinnar S. Complications of the ketogenic diet. Epilepsia. 1998; 39:744–748.
Article7. Nanjo S, Nishikawa J, Miwa S, Mihara H, Fujinami H, Yoshita H, et al. Immune-mediated protein-losing enteropathy with Down syndrome. Intern Med. 2014; 53:2301–2305.
Article8. Dinari G, Rosenbach Y, Zahavi I, Sivan Y, Nitzan M. Random fecal alpha 1-antitrypsin excretion in children with intestinal disorders. Am J Dis Child. 1984; 138:971–973.
Article9. Wang SJ, Tsai SC, Lan JL. Tc-99m albumin scintigraphy to monitor the effect of treatment in protein-losing gastroenteropathy. Clin Nucl Med. 2000; 25:197–199.
Article10. Braamskamp MJ, Dolman KM, Tabbers MM. Clinical practice. Protein-losing enteropathy in children. Eur J Pediatr. 2010; 169:1179–1185.11. van de Ven AA, Hoytema van Konijnenburg DP, Wensing AM, van Montfrans JM. The role of prolonged viral gastrointestinal infections in the development of immunodeficiency-related enteropathy. Clin Rev Allergy Immunol. 2012; 42:79–91.
Article12. Khan RR, Lawson AD, Minnich LL, Martin K, Nasir A, Emmett MK, et al. Gastrointestinal norovirus infection associated with exacerbation of inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2009; 48:328–333.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Primary Sjogren's Syndrome with Protein-losing Enteropathy
- A case of systemic lupus erythematosus with chylothorax, chronic interstitial cystitis and protein-losing enteropathy
- Treatment of Protein-losing Enteropathy After Fontan Procedure by Conversion to the Total Cavopulmonary Connection with Fenestration
- A Case of Protein-losing Enteropathy in Congestive Heart Failure : Resolution with Prednisolone
- A case of constrictive pericarditis presenting with protein-losing enteropathy