J Dent Anesth Pain Med.
2018 Aug;18(4):245-254. 10.17245/jdapm.2018.18.4.245.
Analysis of the effect of oral midazolam and triazolam premedication before general anesthesia in patients with disabilities with difficulty in cooperation
- Affiliations
-
- 1Department of Dental Anesthesiology, Seoul National University, School of Dentistry, Seoul, Korea. stone90@snu.ac.kr
- 2Department of Dental Anesthesiology, Seoul National University Dental Hospital, Seoul, Korea.
- 3Special Care Clinic, Seoul National University Dental Hospital, Seoul, Korea.
- 4Department of Oral and Maxillofacial Surgery, Seoul National University Dental Hospital, Seoul, Korea.
- KMID: 2419066
- DOI: http://doi.org/10.17245/jdapm.2018.18.4.245
Abstract
- BACKGROUND
When performing dental treatment under general anesthesia in adult patients who have difficulty cooperating due to intellectual disabilities, anesthesia induction may be difficult as well. In particular, patients who refuse to come into the dental office or sit in the dental chair may have to be forced to do so. However, for adult patients with a large physique, physical restraint may be difficult, while oral sedatives as premedication may be helpful. Here, a retrospective analysis was performed to investigate the effect of oral sedatives.
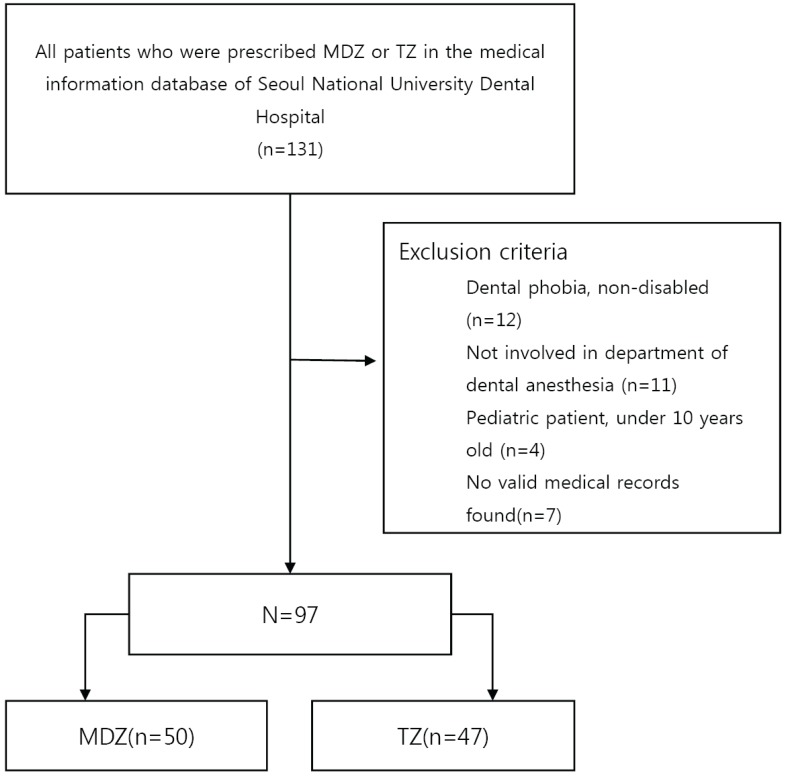
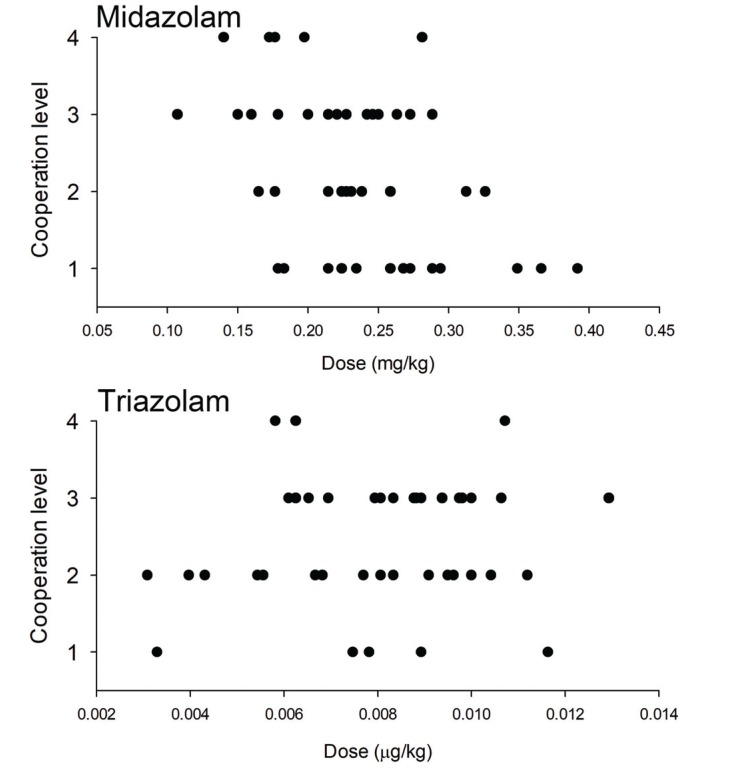
METHODS
A hospital-based medical information database was searched for patients who were prescribed oral midazolam or triazolam between January 2009 and December 2017. Pre-anesthesia evaluation, anesthesia, and anesthesia recovery records of all patients were analyzed, and information on disability type, reason for prescribing oral sedatives, prescribed medication and dose, cooperation level during anesthesia induction, anesthesia duration, length of recovery room stay, and complications was retrieved.
RESULTS
A total of 97 patients were identified, of whom 50 and 47 received midazolam and triazolam, respectively. The major types of disability were intellectual disabilities, autism, Down syndrome, blindness, cerebral palsy, and epilepsy. Analyses of changes in cooperation levels after drug administration showed that anesthesia induction without physical restraint was possible in 56.0% of patients in the midazolam group and in 46.8% of patients in the triazolam group (P = 0.312).
CONCLUSIONS
With administration of oral midazolam or triazolam, general anesthesia induction without any physical restraint was possible in approximately 50% of patients, with no difference between the drugs.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Difficult intubation caused by an immature upper airway in a patient with cri-du-chat syndrome: a case report
Eunsun So, Seungoh Kim
J Dent Anesth Pain Med. 2020;20(1):49-53. doi: 10.17245/jdapm.2020.20.1.49.
Reference
-
1. Lim M, Borromeo GL. The use of general anesthesia to facilitate dental treatment in adult patients with special needs. J Dent Anesth Pain Med. 2017; 17:91–103. PMID: 28879336.
Article2. Haywood PT, Karalliedde LD. General anesthesia for disabled patients in dental practice. Anesth Prog. 1998; 45:134–138. PMID: 10483384.3. Seo KS, Shin TJ, Kim HJ, Han HJ, Han JH, Kim HJ, et al. Clinico-statistical analysis of cooperation and anesthetic induction method of dental patients with special needs. J Korean Dent Soc Anesthesiol. 2009; 9:9–16.
Article4. Christiansen E, Chambers N. Induction of anesthesia in a combative child; management and issues. Paediatr Anaesth. 2005; 15:421–425. PMID: 15828995.
Article5. American Dental Association. Guidelines for the use of sedation and general anesthesia by dentists 2007.6. Hanamoto H, Boku A, Sugimura M, Oyamaguchi A, Inoue M, Niwa H. Premedication with midazolam in intellectually disabled dental patients: Intramuscular or oral administration? A retrospective study. Med Oral Patol Oral Cir Bucal. 2016; 21:e470–e476. PMID: 27031068.
Article7. Horacek J, Palenicek T, Malek J, Scigel V, Kurzova A, Hess L. The influence of clonidine on oral ketaminemidazolam premedication in intellectually disabled patients indicated for dental procedures: Double-blind comparison of two sedation regimes. Neuro Endocrinol Lett. 2012; 33:380–384. PMID: 22936266.8. Lee Y, Kim J, Kim S, Kim J. Intranasal administration of dexmedetomidine (dex) as a premedication for pediatric patients undergoing general anesthesia for dental treatment. J Dent Anesth Pain Med. 2016; 16:25–29. PMID: 28879292.
Article9. Koh GH, Kim SH, Son HJ, Jo JY, Choi SS, Park SU, et al. Pulmonary aspiration during intubation in a high-risk patient: A video clip and clinical implications. J Dent Anesth Pain Med. 2018; 18:111–114. PMID: 29744386.
Article10. Son YG, Shin J, Ryu HG. Pneumonitis and pneumonia after aspiration. J Dent Anesth Pain Med. 2017; 17:1–12. PMID: 28879323.
Article11. Higgins M. Dental anesthesiology--an access to care issue. Alpha Omegan. 2006; 99:56–63. PMID: 17042443.12. Boyle CA, Manley MC, Fleming GJ. Oral midazolam for adults with learning disabilities. Dent Update. 2000; 27:190–192. PMID: 11218455.
Article13. Lee BS, Seo KS, Shin TJ, Kim HJ, Han HJ, Chang J. Premedication of oral midazolam for smooth anesthesia induction of uncooperative patients. J Korean Dent Soc Anesthesiol. 2011; 11:125–132.
Article14. Lieblich SE, Horswell B. Attenuation of anxiety in ambulatory oral surgery patients with oral triazolam. J Oral Maxillofac Surg. 1991; 49:792–796. PMID: 2072190.
Article15. Solomon A. Indications for dental anesthesia. Dent Clin North Am. 1987; 31:75–80. PMID: 2948844.16. Peretz B, Gluck GM. The use of restraint in the treatment of paediatric dental patients: Old and new insights. Int J Paediatr Dent. 2002; 12:392–397. PMID: 12452979.
Article17. Mitchell A, Clegg J. Is post-traumatic stress disorder a helpful concept for adults with intellectual disability? J Intellect Disabil Res. 2005; 49:552–559. PMID: 15966963.
Article18. Luiselli JK, Pace GM, Dunn EK. Antecedent analysis of therapeutic restraint in children and adolescents with acquired brain injury: A descriptive study of four cases. Brain Inj. 2003; 17:255–264. PMID: 12623502.
Article19. Holm-Knudsen RJ, Carlin JB, McKenzie IM. Distress at induction of anaesthesia in children. A survey of incidence, associated factors and recovery characteristics. Paediatr Anaesth. 1998; 8:383–392. PMID: 9742532.20. Tripi PA, Palermo TM, Thomas S, Goldfinger MM, Florentino-Pineda I. Assessment of risk factors for emergence distress and postoperative behavioural changes in children following general anaesthesia. Paediatr Anaesth. 2004; 14:235–240. PMID: 14996262.
Article21. Bozkurt P. Premedication of the pediatric patient-anesthesia for the uncooperative child. Curr Opin Anaesthesiol. 2007; 20:211–215. PMID: 17479023.22. Cote CJ, Cohen IT, Suresh S, Rabb M, Rose JB, Weldon BC, et al. Acomparison of three doses of a commercially prepared oral midazolam syrup in children. Anesth Analg. 2002; 94:37–43. PMID: 11772797.23. Levine MF, Spahr-Schopfer IA, Hartley E, Lerman J, MacPherson B. Oral midazolam premedication in children: The minimum time interval for separation from parents. Can J Anaesth. 1993; 40:726–729. PMID: 8403157.
Article24. Stopperich PS, Moore PA, Finder RL, McGirl BE, Weyant RJ. Oral triazolam pretreatment for intravenous sedation. Anesth Prog. 1993; 40:117–121. PMID: 7943920.25. Kinirons MT, Lang CC, He HB, Ghebreselasie K, Shay S, Robin DW, et al. Triazolam pharmacokinetics and pharmacodynamics in caucasians and southern asians: Ethnicity and cyp3a activity. Br J Clin Pharmacol. 1996; 41:69–72. PMID: 8824695.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Use of triazolam and alprazolam as premedication for general anesthesia
- Premedication of Oral Midazolam for Smooth Anesthesia Induction of Uncooperative Patients
- The effect of triazolam premedication on anxiety, sedation, and amnesia in general anesthesia
- Dental treatment under general anesthesia for patients with severe disabilities
- Prevention of Hypokalemia before Induction of Anesthesia by Clonidine or Midazolam