Intest Res.
2018 Jul;16(3):458-466. 10.5217/ir.2018.16.3.458.
Risk factors for severity of colonic diverticular hemorrhage
- Affiliations
-
- 1Department of Gastroenterology, Fukuoka University Chikushi Hospital, Chikushino, Japan. matsui@fukuoka-u.ac.jp
- 2Department of Endoscopy, Fukuoka University Chikushi Hospital, Chikushino, Japan.
- 3Department of Community Health and Clinical Epidemiology, St. Mary's College, Kurume, Japan.
- KMID: 2417658
- DOI: http://doi.org/10.5217/ir.2018.16.3.458
Abstract
- BACKGROUND/AIMS
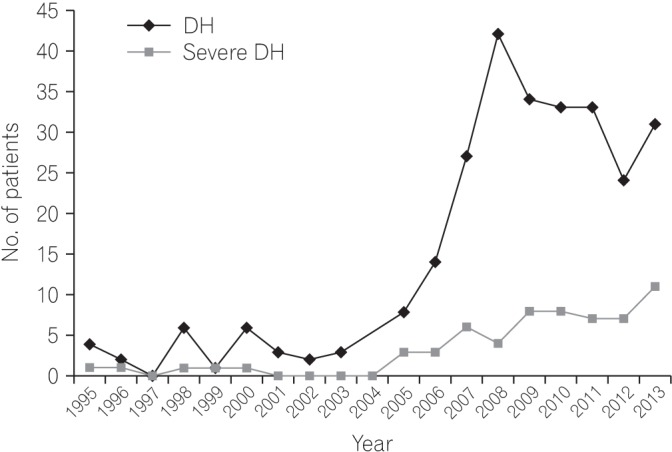
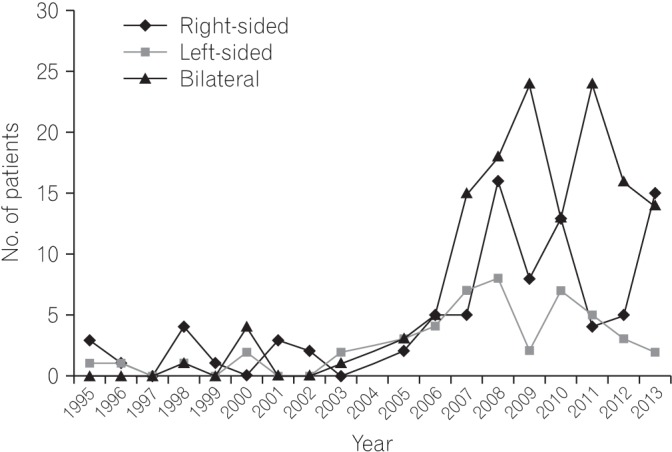
Colonic diverticular hemorrhage (DH) was a rare disease until the 1990s, and its incidence has increased rapidly since 2000 in Japan. In recent years, colonic DH has been the most frequent cause of lower gastrointestinal bleeding (LGIB). Nearly all cases of DH are mild, with the bleeding often stopping spontaneously. Some cases, however, require surgery or arterial embolization. In this study, using a cohort at Fukuoka University Chikushi Hospital, we investigated factors associated with severe colonic DH.
METHODS
Among patients with LGIB who underwent colonoscopy at our hospital between 1995 and 2013, DH was identified in 273 patients. Among them, 62 patients (22.7%) were defined as having severe colonic DH according to recurrence of bleeding in a short period, and/or the necessity of transfusion, arterial embolization, or surgery. We then evaluated risk factors for severe DH among DH patients in this retrospective cohort.
RESULTS
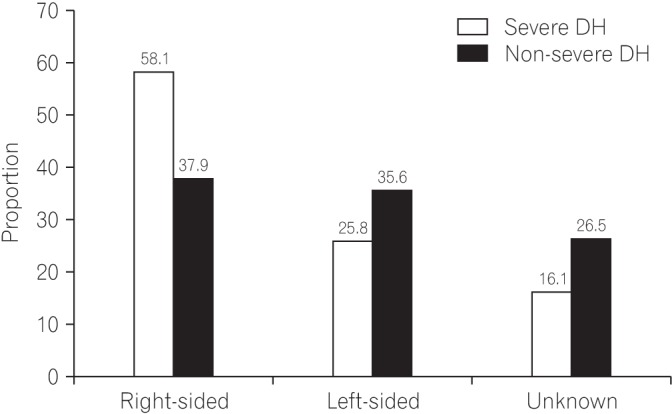
Among the 273 patients with DH, use of non-steroidal anti-inflammatory drugs (NSAIDs) (odds ratio [OR], 2.801; 95% confidence interval [CI], 1.164-6.742), Charlson Risk Index (CRI) ≥2 (OR, 3.336; 95% CI, 1.154-7.353), right-sided colonic DH (OR, 3.873; 95% CI, 1.554-9.653), and symptoms of cerebral hypoperfusion (such as light-headedness, dizziness, or syncope) (OR, 2.926; 95% CI, 1.310-6.535) showed an increased risk of severe DH even after controlling for other factors.
CONCLUSIONS
Severe DH occurred in 23% of DH patients, and NSAID use, CRI ≥2, right-sided colonic DH, and symptoms of cerebral hypoperfusion are suggested to be predictors of severe DH.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Diagnosis and Treatment of Colonic Diverticular Disease
You Sun Kim
Korean J Gastroenterol. 2022;79(6):233-243. doi: 10.4166/kjg.2022.072.Vegetarianism as a protective factor for asymptomatic colonic diverticulosis in Asians: a retrospective cross-sectional and case-control study
Jihun Bong, Hyoun Woo Kang, Hyeki Cho, Ji Hyung Nam, Dong Kee Jang, Jae Hak Kim, Jun Kyu Lee, Yun Jeong Lim, Moon-Soo Koh, Jin Ho Lee
Intest Res. 2020;18(1):121-129. doi: 10.5217/ir.2019.00106.
Reference
-
1. Kinjo K, Matsui T, Hisabe T, et al. Increase in colonic diverticular hemorrhage and confounding factors. World J Gastrointest Pharmacol Ther. 2016; 7:440–446. PMID: 27602246.
Article2. Nagata N, Niikura R, Aoki T, et al. Lower GI bleeding risk of nonsteroidal anti-inflammatory drugs and antiplatelet drug use alone and the effect of combined therapy. Gastrointest Endosc. 2014; 80:1124–1131. PMID: 25088922.
Article3. Hreinsson JP, Gumundsson S, Kalaitzakis E, Björnsson ES. Lower gastrointestinal bleeding: incidence, etiology, and outcomes in a population-based setting. Eur J Gastroenterol Hepatol. 2013; 25:37–43. PMID: 23013623.4. Lanas A, García-Rodríguez LA, Polo-Tomás M, et al. Time trends and impact of upper and lower gastrointestinal bleeding and perforation in clinical practice. Am J Gastroenterol. 2009; 104:1633–1641. PMID: 19574968.
Article5. Stollman N, Raskin JB. Diverticular disease of the colon. Lancet. 2004; 363:631–639. PMID: 14987890.
Article6. Tsuruoka N, Iwakiri R, Hara M, et al. NSAIDs are a significant risk factor for colonic diverticular hemorrhage in elder patients: evaluation by a case-control study. J Gastroenterol Hepatol. 2011; 26:1047–1052. PMID: 21198829.
Article7. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987; 40:373–383. PMID: 3558716.
Article8. Jensen DM, Machicado GA, Jutabha R, Kovacs TO. Urgent colonoscopy for the diagnosis and treatment of severe diverticular hemorrhage. N Engl J Med. 2000; 342:78–82. PMID: 10631275.
Article9. Yamada A, Sugimoto T, Kondo S, et al. Assessment of the risk factors for colonic diverticular hemorrhage. Dis Colon Rectum. 2008; 51:116–120. PMID: 18085336.
Article10. Okamoto T, Watabe H, Yamada A, Hirata Y, Yoshida H, Koike K. The association between arteriosclerosis related diseases and diverticular bleeding. Int J Colorectal Dis. 2012; 27:1161–1166. PMID: 22584295.
Article11. Niikura R, Nagata N, Shimbo T, et al. Natural history of bleeding risk in colonic diverticulosis patients: a long-term colonoscopy-based cohort study. Aliment Pharmacol Ther. 2015; 41:888–894. PMID: 25715746.
Article12. McGuire HH Jr. Bleeding colonic diverticula: a reappraisal of natural history and management. Ann Surg. 1994; 220:653–656. PMID: 7979613.
Article13. Poncet G, Heluwaert F, Voirin D, Bonaz B, Faucheron JL. Natural history of acute colonic diverticular bleeding: a prospective study in 133 consecutive patients. Aliment Pharmacol Ther. 2010; 32:466–471. PMID: 20491745.
Article14. Nagata N, Niikura R, Aoki T, et al. Impact of discontinuing non-steroidal antiinflammatory drugs on long-term recurrence in colonic diverticular bleeding. World J Gastroenterol. 2015; 21:1292–1298. PMID: 25632204.
Article15. Niikura R, Nagata N, Yamada A, Akiyama J, Shimbo T, Uemura N. Recurrence of colonic diverticular bleeding and associated risk factors. Colorectal Dis. 2012; 14:302–305. PMID: 21692963.
Article16. Niikura R, Nagata N, Akiyama J, Shimbo T, Uemura N. Hypertension and concomitant arteriosclerotic diseases are risk factors for colonic diverticular bleeding: a case-control study. Int J Colorectal Dis. 2012; 27:1137–1143. PMID: 22354135.
Article17. Aldoori WH, Giovannucci EL, Rimm EB, Wing AL, Willett WC. Use of acetaminophen and nonsteroidal anti-inflammatory drugs: a prospective study and the risk of symptomatic diverticular disease in men. Arch Fam Med. 1998; 7:255–260. PMID: 9596460.
Article18. Meyers MA, Alonso DR, Baer JW. Pathogenesis of massively bleeding colonic diverticulosis: new observations. AJR Am J Roentgenol. 1976; 127:901–908. PMID: 1087123.
Article19. Hussain A, Mahmood H, Subhas G, El-Hasani S. Complicated diverticular disease of the colon, do we need to change the classical approach, a retrospective study of 110 patients in southeast England. World J Emerg Surg. 2008; 3:5. PMID: 18218109.
Article20. Chen CY, Wu CC, Jao SW, Pai L, Hsiao CW. Colonic diverticular bleeding with comorbid diseases may need elective colectomy. J Gastrointest Surg. 2009; 13:516–520. PMID: 19005733.
Article21. Nagata N, Niikura R, Aoki T, et al. Increase in colonic diverticulosis and diverticular hemorrhage in an aging society: lessons from a 9-year colonoscopic study of 28,192 patients in Japan. Int J Colorectal Dis. 2014; 29:379–385. PMID: 24317937.
Article22. Wong SK, Ho YH, Leong AP, Seow-Choen F. Clinical behavior of complicated right-sided and left-sided diverticulosis. Dis Colon Rectum. 1997; 40:344–348. PMID: 9118752.
Article23. García Rodríguez LA, Jick H. Risk of upper gastrointestinal bleeding and perforation associated with individual non-steroidal anti-inflammatory drugs. Lancet. 1994; 343:769–772. PMID: 7907735.
Article24. Geramizadeh B, Taghavi A, Banan B. Clinical, endoscopic and pathologic spectrum of non-steroidal anti-inflammatory drug-induced colitis. Indian J Gastroenterol. 2009; 28:150–153. PMID: 19937416.
Article25. Masannat YA, Harron M, Harinath G. Nonsteroidal anti-inflammatory drugs-associated colopathy. ANZ J Surg. 2010; 80:96–99. PMID: 20575887.
Article26. Halter F, Weber B, Huber T, Eigenmann F, Frey MP, Ruchti C. Diaphragm disease of the ascending colon. Association with sustained-release diclofenac. J Clin Gastroenterol. 1993; 16:74–80. PMID: 8421154.27. Lee KK, Shah SM, Moser MA. Risk factors predictive of severe diverticular hemorrhage. Int J Surg. 2011; 9:83–85. PMID: 20937418.
Article28. Pilichos C, Bobotis E. Role of endoscopy in the management of acute diverticular bleeding. World J Gastroenterol. 2008; 14:1981–1983. PMID: 18395895.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnosis and Treatment of Colonic Diverticular Disease
- Analysis of Risk Factors for Colonic Diverticular Bleeding: A Matched Case-Control Study
- The Risk Factors for Colonic Diverticular Bleeding
- Clinical Characteristics of Colonic Diverticular Disease Diagnosed with Colonoscopy
- Predictive Factors for Colonic Diverticular Rebleeding: A Retrospective Analysis of the Clinical and Colonoscopic Features of 111 Patients