Korean J Gastroenterol.
2022 Jun;79(6):233-243. 10.4166/kjg.2022.072.
Diagnosis and Treatment of Colonic Diverticular Disease
- Affiliations
-
- 1Department of Internal Medicine, Seoul Paik Hospital, Inje University College of Medicine, Seoul, Korea
- KMID: 2530696
- DOI: http://doi.org/10.4166/kjg.2022.072
Abstract
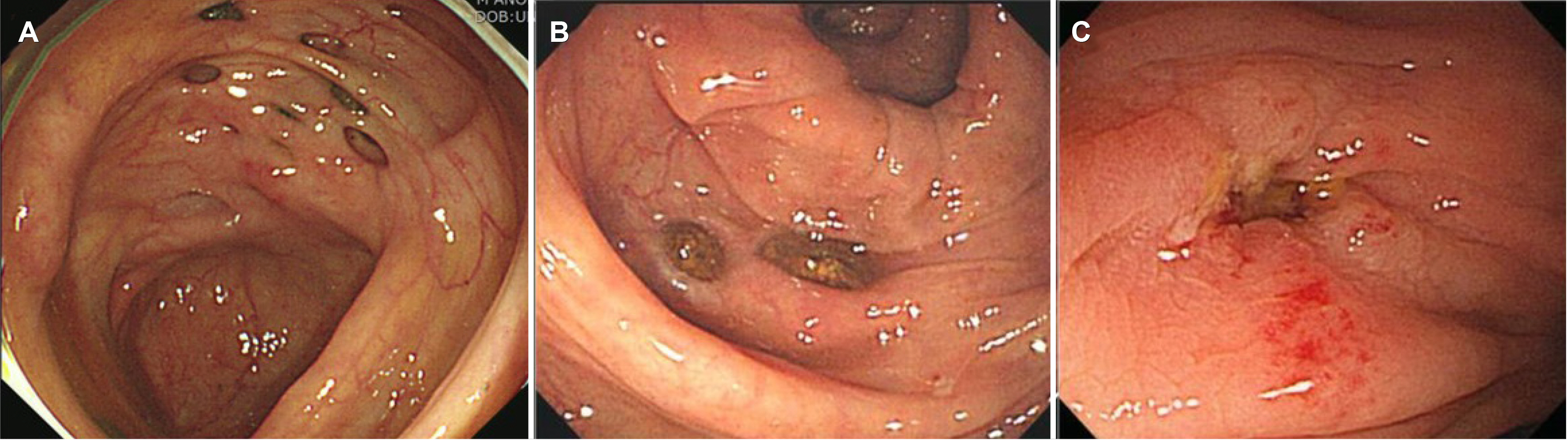
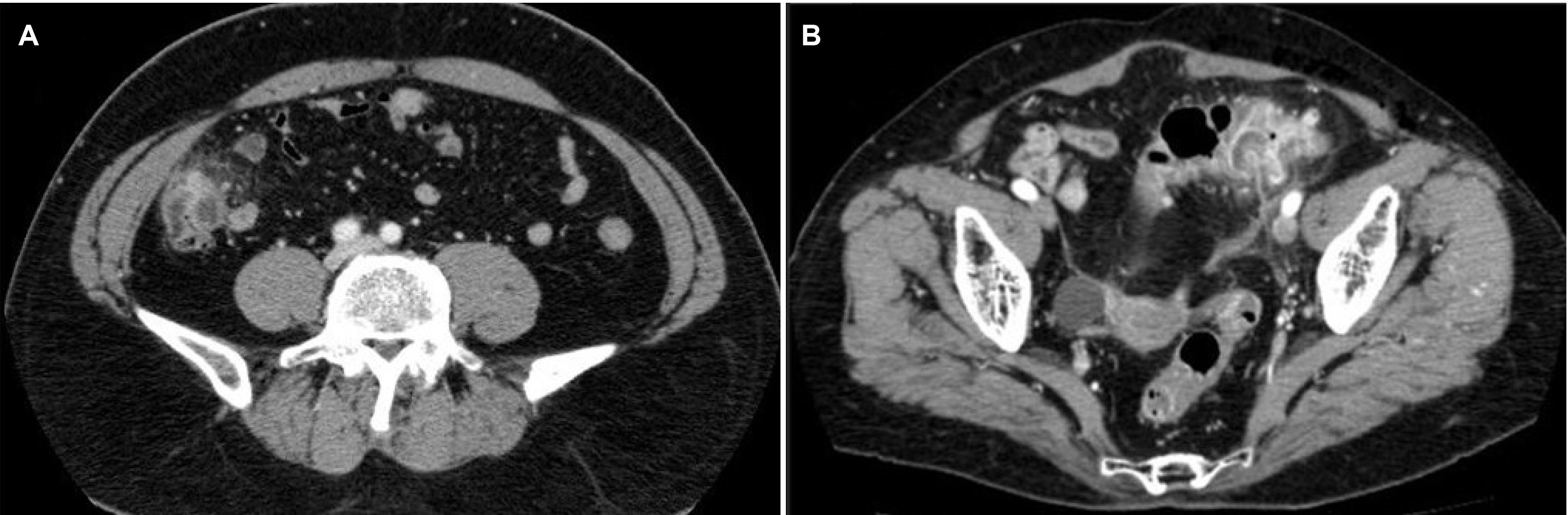
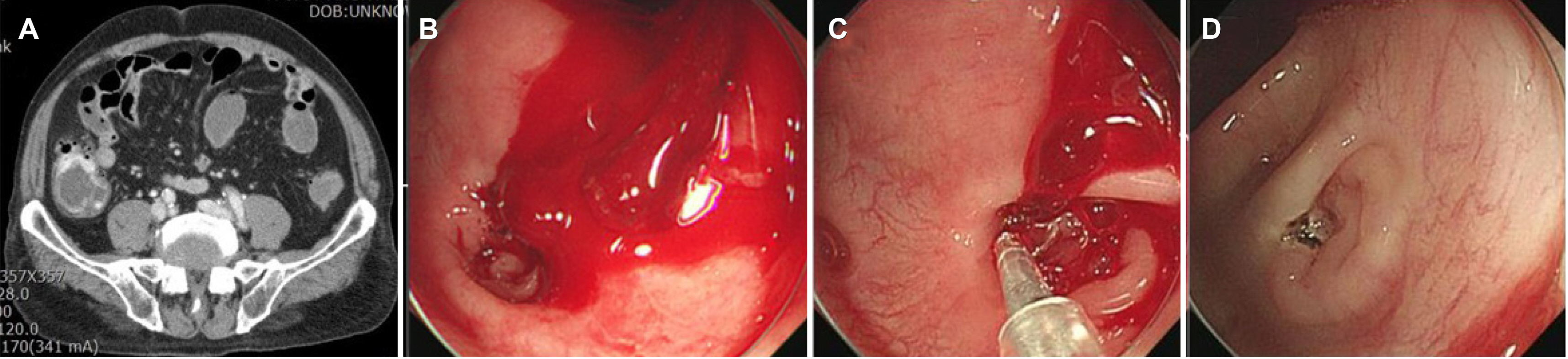
- Colonic diverticulosis is one of the most common conditions of the digestive system and patients generally remain asymptomatic. However, about 20% of patients develop symptomatic diverticular disease such as acute diverticulitis or diverticular hemorrhage, and these have become a huge burden on healthcare systems worldwide. Recent understanding of the pathophysiology of diverticulosis and diverticular disease suggests the role of multiple factors including genetic and environment. Based on this understanding, a preventive strategy to reduce the risk factors of diverticulosis and diverticular disease is highly recommended. The diagnosis of the acute diverticulitis relies on imaging modalities such as an abdominal-pelvic CT scan together with symptoms and signs. Treatment of diverticular disease should be individualized and include modification of lifestyle, use of antibiotics, and surgery. Recent guidelines recommend pursuing less aggressive treatment for patients with acute diverticulitis. This review will provide an overview of both the existing and evolving understanding regarding colonic diverticulosis and diverticular disease and can help clinicians in the management of their patients with diverticular disease.
Keyword
Figure
Reference
-
1. Commane DM, Arasaradnam RP, Mills S, Mathers JC, Bradburn M. 2009; Diet, ageing and genetic factors in the pathogenesis of diverticular disease. World J Gastroenterol. 15:2479–2488. DOI: 10.3748/wjg.15.2479. PMID: 19468998. PMCID: PMC2686906.
Article2. Peery AF, Crockett SD, Barritt AS, et al. 2015; Burden of gastrointestinal, liver, and pancreatic diseases in the United States. Gastroenterology. 149:1731–1741.e3. DOI: 10.1053/j.gastro.2015.08.045. PMID: 26327134. PMCID: PMC4663148.
Article3. Rezapour M, Ali S, Stollman N. 2018; Diverticular disease: an update on pathogenesis and management. Gut Liver. 12:125–132. DOI: 10.5009/gnl16552. PMID: 28494576. PMCID: PMC5832336.
Article4. Fong SS, Tan EY, Foo A, Sim R, Cheong DM. 2011; The changing trend of diverticular disease in a developing nation. Colorectal Dis. 13:312–316. DOI: 10.1111/j.1463-1318.2009.02121.x. PMID: 19906060.
Article5. Song JH, Kim YS, Lee JH, et al. 2010; Clinical characteristics of colonic diverticulosis in Korea: a prospective study. Korean J Intern Med. 25:140–146. DOI: 10.3904/kjim.2010.25.2.140. PMID: 20526386. PMCID: PMC2880686.
Article6. Choe EK, Lee JE, Chung SJ, et al. 2019; Genome-wide association study of right-sided colonic diverticulosis in a Korean population. Sci Rep. 9:7360. DOI: 10.1038/s41598-019-43692-8. PMID: 31089239. PMCID: PMC6517584.
Article7. Tursi A, Scarpignato C, Strate LL, et al. 2020; Colonic diverticular disease. Nat Rev Dis Primers. 6:20. DOI: 10.1038/s41572-020-0153-5. PMID: 32218442. PMCID: PMC7486966.
Article8. Nagata N, Niikura R, Aoki T, et al. 2014; Increase in colonic diverticulosis and diverticular hemorrhage in an aging society: lessons from a 9-year colonoscopic study of 28,192 patients in Japan. Int J Colorectal Dis. 29:379–385. DOI: 10.1007/s00384-013-1808-4. PMID: 24317937.
Article9. Bharucha AE, Parthasarathy G, Ditah I, et al. 2015; Temporal trends in the incidence and natural history of diverticulitis: a population-based study. Am J Gastroenterol. 110:1589–1596. DOI: 10.1038/ajg.2015.302. PMID: 26416187. PMCID: PMC4676761.
Article10. Yamada E, Ohkubo H, Higurashi T, et al. 2013; Visceral obesity as a risk factor for left-sided diverticulitis in Japan: a multicenter retrospective study. Gut Liver. 7:532–538. DOI: 10.5009/gnl.2013.7.5.532. PMID: 24073310. PMCID: PMC3782667.
Article11. Lee JH, Ahn BK, Lee KH. 2021; Conservative treatment of uncomplicated right-sided diverticulitis: a systematic review and meta-analysis. Int J Colorectal Dis. 36:1791–1799. DOI: 10.1007/s00384-021-03913-x. PMID: 33765173.
Article12. Qaseem A, Etxeandia-Ikobaltzeta I, Lin JS, et al. 2022; Diagnosis and management of acute left-sided colonic diverticulitis: a clinical guideline from the American College of Physicians. Ann Intern Med. 175:399–415. DOI: 10.7326/M21-2710. PMID: 35038273.
Article13. Stollman N, Smalley W, Hirano I. AGA Institute Clinical Guidelines Committee. 2015; American Gastroenterological Association institute guideline on the management of acute diverticulitis. Gastroenterology. 149:1944–1949. DOI: 10.1053/j.gastro.2015.10.003. PMID: 26453777.
Article14. Kruis W, Germer CT, Leifeld L. German Society for Gastroenterology, Digestive and Metabolic Diseases and The German Society for General and Visceral Surgery. 2014; Diverticular disease: guidelines of the german society for gastroenterology, digestive and metabolic diseases and the german society for general and visceral surgery. Digestion. 90:190–207. DOI: 10.1159/000367625. PMID: 25413249.
Article15. Peery AF, Keku TO, Martin CF, et al. 2016; Distribution and characteristics of colonic diverticula in a United States screening population. Clin Gastroenterol Hepatol. 14:980–985.e1. DOI: 10.1016/j.cgh.2016.01.020. PMID: 26872402. PMCID: PMC4912930.
Article16. Martel J, Raskin JB. NDSG. 2008; History, incidence, and epidemiology of diverticulosis. J Clin Gastroenterol. 42:1125–1127. DOI: 10.1097/MCG.0b013e3181865f18. PMID: 18936648.
Article17. Stollman N, Raskin JB. 2004; Diverticular disease of the colon. Lancet. 363:631–639. DOI: 10.1016/S0140-6736(04)15597-9. PMID: 14987890.
Article18. Kim KS, Lee KS, Choi SS, Song IS. 1984; Recent changes of colonic diverticulosis in Korea. J Korean Radiol Soc. 20:632–638. DOI: 10.3348/jkrs.1984.20.3.632.
Article19. Ko JK, Lee JK, Yun EJ, Moon HJ, Shin HJ. 1997; Colonic diverticulosis: evaluation wth double contrast barium enema. J Korean Radiol Soc. 36:285–289. DOI: 10.3348/jkrs.1997.36.2.285.
Article20. Son MY, Chang JC, Hwang MS, Kim SY, Park BH, Sim MC. 1990; Radiologic analysis of developmental pattern in colonic diverticulosis. Korean J Gastroenterol. 22:94–99.21. Choi CS, Cho EY, Kweon JH, et al. 2007; The prevalence and clinical features of colonic diverticulosis diagnosed with colonscopy. Clin Endosc. 35:146–151.22. Kim KO, Jang BI, Kim TN, Moon HJ. 2008; Overview of the annual frequency and clinical manifestations of colonic diverticulosis. Intest Res. 6:116–120.23. Lee SJ, Kim SA, Ku BH, et al. 2012; Association between colorectal cancer and colonic diverticulosis: case-control study based on computed tomographic colonography. Abdom Imaging. 37:70–73. DOI: 10.1007/s00261-011-9743-8. PMID: 21516446.
Article24. Simpson J, Scholefield JH, Spiller RC. 2002; Pathogenesis of colonic diverticula. Br J Surg. 89:546–554. DOI: 10.1046/j.1365-2168.2002.02076.x. PMID: 11972543.
Article25. Weinreich J, Möller SH, Andersen D. 1977; Colonic haustral pattern in relation to pressure activity and presence of diverticula. Scand J Gastroenterol. 12:857–864. DOI: 10.3109/00365527709181730. PMID: 594654.
Article26. Peery AF, Sandler RS, Ahnen DJ, et al. 2013; Constipation and a low-fiber diet are not associated with diverticulosis. Clin Gastroenterol Hepatol. 11:1622–1627. DOI: 10.1016/j.cgh.2013.06.033. PMID: 23891924. PMCID: PMC3840096.
Article27. Bong J, Kang HW, Cho H, et al. 2020; Vegetarianism as a protective factor for asymptomatic colonic diverticulosis in Asians: a retrospective cross-sectional and case-control study. Intest Res. 18:121–129. DOI: 10.5217/ir.2019.00106. PMID: 31661949. PMCID: PMC7000646.
Article28. Strate LL, Erichsen R, Baron JA, et al. 2013; Heritability and familial aggregation of diverticular disease: a population-based study of twins and siblings. Gastroenterology. 144:736–e14. DOI: 10.1053/j.gastro.2013.02.011. PMID: 23313967.
Article29. Granlund J, Svensson T, Olén O, et al. 2012; The genetic influence on diverticular disease--a twin study. Aliment Pharmacol Ther. 35:1103–1107. DOI: 10.1111/j.1365-2036.2012.05069.x. PMID: 22432696.30. Kim SY, Kim YS, Kim HT, et al. 2013; A prospective study of factors influencing on the clinical characteristics of colonic diverticulosis. Korean J Gastroenterol. 62:97–103. DOI: 10.4166/kjg.2013.62.2.97. PMID: 23981943.
Article31. Turner GA, O'Grady MJ, Purcell RV, Frizelle FA. 2021; The epidemiology and etiology of right-sided colonic diverticulosis: a review. Ann Coloproctol. 37:196–203. DOI: 10.3393/ac.2021.00192.0027. PMID: 34284562. PMCID: PMC8391037.
Article32. Dore MP, Pes GM, Marras G, et al. 2016; Risk factors associated with colonic diverticulosis among patients from a defined geographic area. Tech Coloproctol. 20:177–183. DOI: 10.1007/s10151-015-1401-7. PMID: 26568053.
Article33. Takano M, Yamada K, Sato K. 2005; An analysis of the development of colonic diverticulosis in the Japanese. Dis Colon Rectum. 48:2111–2116. DOI: 10.1007/s10350-005-0111-z. PMID: 16228844.
Article34. Lim JH, Kim YS, Lee JE, et al. 2021; Dietary pattern and its association with right-colonic diverticulosis. J Gastroenterol Hepatol. 36:144–150. DOI: 10.1111/jgh.15145. PMID: 32525584.
Article35. Strate LL, Morris AM. 2019; Epidemiology, pathophysiology, and treatment of diverticulitis. Gastroenterology. 156:1282–1298. e1. DOI: 10.1053/j.gastro.2018.12.033. PMID: 30660732. PMCID: PMC6716971.
Article36. Spiller R. 2012; Is it diverticular disease or is it irritable bowel syndrome? Dig Dis. 30:64–69. DOI: 10.1159/000335721. PMID: 22572688.
Article37. Strate LL, Modi R, Cohen E, Spiegel BM. 2012; Diverticular disease as a chronic illness: evolving epidemiologic and clinical insights. Am J Gastroenterol. 107:1486–1493. DOI: 10.1038/ajg.2012.194. PMID: 22777341.
Article38. Yamamichi N, Shimamoto T, Takahashi Y, et al. 2015; Trend and risk factors of diverticulosis in Japan: age, gender, and lifestyle/metabolic-related factors may cooperatively affect on the colorectal diverticula formation. PLoS One. 10:e0123688. DOI: 10.1371/journal.pone.0123688. PMID: 25860671. PMCID: PMC4393308.
Article39. Shahedi K, Fuller G, Bolus R, et al. 2013; Long-term risk of acute diverticulitis among patients with incidental diverticulosis found during colonoscopy. Clin Gastroenterol Hepatol. 11:1609–1613. DOI: 10.1016/j.cgh.2013.06.020. PMID: 23856358. PMCID: PMC5731451.
Article40. Hjern F, Wolk A, Håkansson N. 2012; Obesity, physical inactivity, and colonic diverticular disease requiring hospitalization in women: a prospective cohort study. Am J Gastroenterol. 107:296–302. DOI: 10.1038/ajg.2011.352. PMID: 22008890.
Article41. Aune D, Sen A, Leitzmann MF, Norat T, Tonstad S, Vatten LJ. 2017; Body mass index and physical activity and the risk of diverticular disease: a systematic review and meta-analysis of prospective studies. Eur J Nutr. 56:2423–2438. DOI: 10.1007/s00394-017-1443-x. PMID: 28393286. PMCID: PMC5682875.
Article42. Bae HJ, Kim ST, Hong SG, et al. 2019; Risk factors for asymptomatic colon diverticulosis. Korean J Gastroenterol. 74:142–148. DOI: 10.4166/kjg.2019.74.3.142. PMID: 31554029.
Article43. Strate LL, Keeley BR, Cao Y, Wu K, Giovannucci EL, Chan AT. 2017; Western dietary pattern increases, and prudent dietary pattern decreases, risk of incident diverticulitis in a prospective cohort study. Gastroenterology. 152:1023–1030.e2. DOI: 10.1053/j.gastro.2016.12.038. PMID: 28065788. PMCID: PMC5367955.
Article44. Strate LL, Liu YL, Aldoori WH, Syngal S, Giovannucci EL. 2009; Obesity increases the risks of diverticulitis and diverticular bleeding. Gastroenterology. 136:115–122.e1. DOI: 10.1053/j.gastro.2008.09.025. PMID: 18996378. PMCID: PMC2643271.
Article45. Humes DJ, Ludvigsson JF, Jarvholm B. 2016; Smoking and the risk of hospitalization for symptomatic diverticular disease: a population-based cohort study from Sweden. Dis Colon Rectum. 59:110–114. DOI: 10.1097/DCR.0000000000000515. PMID: 26734968.
Article46. Liu PH, Cao Y, Keeley BR, et al. 2017; Adherence to a healthy lifestyle is associated with a lower risk of diverticulitis among men. Am J Gastroenterol. 112:1868–1876. DOI: 10.1038/ajg.2017.398. PMID: 29112202. PMCID: PMC5736501.
Article47. Humes DJ, Fleming KM, Spiller RC, West J. 2011; Concurrent drug use and the risk of perforated colonic diverticular disease: a population-based case-control study. Gut. 60:219–224. DOI: 10.1136/gut.2010.217281. PMID: 20940283.
Article48. Kvasnovsky CL, Papagrigoriadis S, Bjarnason I. 2014; Increased diverticular complications with nonsteriodal anti-inflammatory drugs and other medications: a systematic review and meta-analysis. Colorectal Dis. 16:O189–O196. DOI: 10.1111/codi.12516. PMID: 24320820.
Article49. Suh S, Seo PJ, Park H, et al. 2012; The risk factors for colonic diverticular bleeding. Korean J Gastroenterol. 60:349–354. DOI: 10.4166/kjg.2012.60.6.349. PMID: 23242017.
Article50. Andeweg CS, Wegdam JA, Groenewoud J, van der Wilt GJ, van Goor H, Bleichrodt RP. 2014; Toward an evidence-based step-up approach in diagnosing diverticulitis. Scand J Gastroenterol. 49:775–784. DOI: 10.3109/00365521.2014.908475. PMID: 24874087.
Article51. Chabok A, Påhlman L, Hjern F, Haapaniemi S, Smedh K. AVOD Study Group. 2012; Randomized clinical trial of antibiotics in acute uncomplicated diverticulitis. Br J Surg. 99:532–539. DOI: 10.1002/bjs.8688. PMID: 22290281.52. Daniels L, Ünlü Ç, de Korte N, et al. 2017; Randomized clinical trial of observational versus antibiotic treatment for a first episode of CT-proven uncomplicated acute diverticulitis. Br J Surg. 104:52–61. DOI: 10.1002/bjs.10309. PMID: 27686365.53. Qaseem A, Etxeandia-Ikobaltzeta I, Lin JS, et al. 2022; Colonoscopy for diagnostic evaluation and interventions to prevent recurrence after acute left-sided colonic diverticulitis: a clinical guideline from the American College of Physicians. Ann Intern Med. 175:416–431. DOI: 10.7326/M21-2711. PMID: 35038270.
Article54. Kim HU, Kim YH, Choe WH, et al. 2003; Clinical characteristics of colonic diverticulitis in Koreans. Korean J Gastroenterol. 42:363–368. PMID: 14646572.55. Kim MJ, Woo YS, Kim ER, et al. 2014; Is colonoscopy necessary after computed tomography diagnosis of acute diverticulitis? Intest Res. 12:221–228. DOI: 10.5217/ir.2014.12.3.221. PMID: 25349596. PMCID: PMC4204723.
Article56. Oh HK, Han EC, Ha HK, et al. 2014; Surgical management of colonic diverticular disease: discrepancy between right- and left-sided diseases. World J Gastroenterol. 20:10115–10120. DOI: 10.3748/wjg.v20.i29.10115. PMID: 25110438. PMCID: PMC4123340.
Article57. Regenbogen SE, Hardiman KM, Hendren S, Morris AM. 2014; Surgery for diverticulitis in the 21st century: a systematic review. JAMA Surg. 149:292–303. DOI: 10.1001/jamasurg.2013.5477. PMID: 24430164.58. El-Sayed C, Radley S, Mytton J, Evison F, Ward ST. 2018; Risk of recurrent disease and surgery following an admission for acute diverticulitis. Dis Colon Rectum. 61:382–389. DOI: 10.1097/DCR.0000000000000939. PMID: 29420430.
Article59. Hall JF, Roberts PL, Ricciardi R, et al. 2011; Long-term follow-up after an initial episode of diverticulitis: what are the predictors of recurrence? Dis Colon Rectum. 54:283–288. DOI: 10.1007/DCR.0b013e3182028576. PMID: 21304297.
Article60. Kaiser AM, Jiang JK, Lake JP, et al. 2005; The management of complicated diverticulitis and the role of computed tomography. Am J Gastroenterol. 100:910–917. DOI: 10.1111/j.1572-0241.2005.41154.x. PMID: 15784040.
Article61. Choi KS, Byeon JS, Yoon SM, et al. 2008; Diverticulitis: focused on clinical course and relapse. Intest Res. 6:37–44.62. Kruis W, Kardalinos V, Eisenbach T, et al. 2017; Randomised clinical trial: mesalazine versus placebo in the prevention of diverticulitis recurrence. Aliment Pharmacol Ther. 46:282–291. DOI: 10.1111/apt.14152. PMID: 28543263. PMCID: PMC5518301.
Article63. Raskin JB, Kamm MA, Jamal MM, et al. 2014; Mesalamine did not prevent recurrent diverticulitis in phase 3 controlled trials. Gastroenterology. 147:793–802. DOI: 10.1053/j.gastro.2014.07.004. PMID: 25038431.
Article64. Kinjo K, Matsui T, Hisabe T, et al. 2016; Increase in colonic diverticular hemorrhage and confounding factors. World J Gastrointest Pharmacol Ther. 7:440–446. DOI: 10.4292/wjgpt.v7.i3.440. PMID: 27602246. PMCID: PMC4986401.
Article65. Longstreth GF. 1997; Epidemiology and outcome of patients hospitalized with acute lower gastrointestinal hemorrhage: a population-based study. Am J Gastroenterol. 92:419–424. PMID: 9068461.66. Wong SK, Ho YH, Leong AP, Seow-Choen F. 1997; Clinical behavior of complicated right-sided and left-sided diverticulosis. Dis Colon Rectum. 40:344–348. DOI: 10.1007/BF02050427. PMID: 9118752.
Article67. Poncet G, Heluwaert F, Voirin D, Bonaz B, Faucheron JL. 2010; Natural history of acute colonic diverticular bleeding: a prospective study in 133 consecutive patients. Aliment Pharmacol Ther. 32:466–471. DOI: 10.1111/j.1365-2036.2010.04362.x. PMID: 20491745.
Article68. Nagata N, Niikura R, Aoki T, et al. 2015; Impact of discontinuing non-steroidal antiinflammatory drugs on long-term recurrence in colonic diverticular bleeding. World J Gastroenterol. 21:1292–1298. DOI: 10.3748/wjg.v21.i4.1292. PMID: 25632204. PMCID: PMC4306175.
Article69. Kinjo K, Matsui T, Hisabe T, et al. 2018; Risk factors for severity of colonic diverticular hemorrhage. Intest Res. 16:458–466. DOI: 10.5217/ir.2018.16.3.458. PMID: 30090045. PMCID: PMC6077309.
Article70. Nagata N, Niikura R, Aoki T, et al. 2015; Risk factors for adverse in-hospital outcomes in acute colonic diverticular hemorrhage. World J Gastroenterol. 21:10697–10703. DOI: 10.3748/wjg.v21.i37.10697. PMID: 26457031. PMCID: PMC4588093.
Article71. Kato M. 2019; Endoscopic therapy for acute diverticular bleeding. Clin Endosc. 52:419–425. DOI: 10.5946/ce.2019.078. PMID: 31426626. PMCID: PMC6785408.
Article72. Okamoto N, Tominaga N, Sakata Y, et al. 2019; Lower rebleeding rate after endoscopic band ligation than endoscopic clipping of the same colonic diverticular hemorrhagic lesion: a historical multicenter trial in Saga, Japan. Intern Med. 58:633–638. DOI: 10.2169/internalmedicine.1473-18. PMID: 30333407. PMCID: PMC6443565.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Retrospective Study Comparing Clinical Characteristics between
- Clinical Characteristics of Colonic Diverticular Disease Diagnosed with Colonoscopy
- Recent updates on classification and unsolved issues of diverticular disease: a narrative review
- Surgical Treatment for Diverticular Disease of the Colon
- Diagnosis and Treatment of Colon Diverticulitis