J Korean Med Sci.
2017 Jan;32(1):102-107. 10.3346/jkms.2017.32.1.102.
Therapeutic Response for Functional Abdominal Pain in Children with Occult Constipation: Laxatives versus Prokinetic Drugs
- Affiliations
-
- 1Department of Pediatrics, CHA Bundang Medical Center, CHA University, Seongnam, Korea. jinped@cha.ac.kr
- KMID: 2417591
- DOI: http://doi.org/10.3346/jkms.2017.32.1.102
Abstract
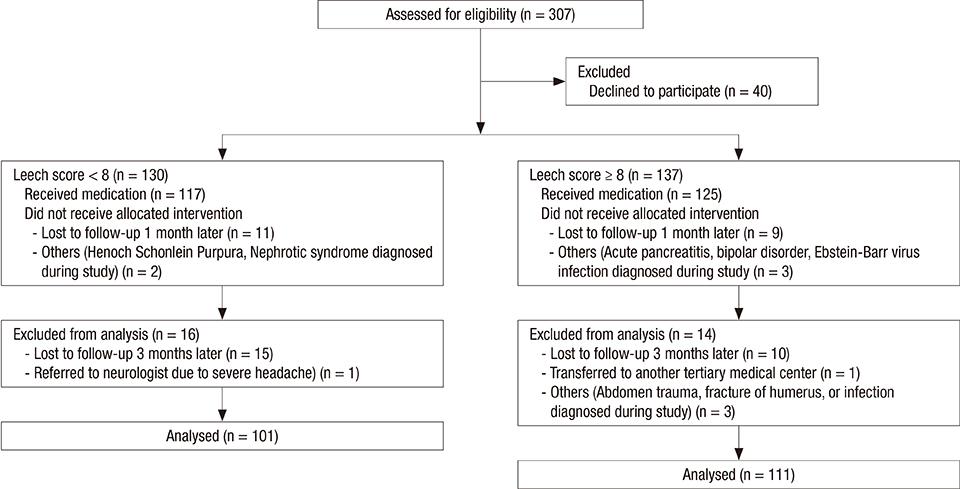
- The relationship between functional abdominal pain (FAP) and occult constipation (OC) in children who did not meet the Rome III criteria for constipation has rarely been reported. This study aimed to estimate the prevalence of OC in patients with FAP and to compare the effectiveness of prokinetic drugs and laxatives for FAP and OC. Pediatric outpatients (n = 212; aged 4-15 years) who satisfied the Rome III criteria for childhood FAP were divided into 2 groups based on Leech scores: group 1 < 8; group 2 ≥ 8. Group 2 received either prokinetic drugs or laxatives and pain severity was assessed after 2 weeks, 1 month, and 3 months. A total 52.4% (111/212) of patients had OC in this study. More patients who received laxatives had reduced pain scores compared with those who received prokinetic drugs. Those treated with laxatives in group 2 had a better response than those treated with prokinetic drugs throughout the study period (P < 0.001, P < 0.001, and P = 0.002 after 2 weeks, 1 month, and 3 months, respectively). OC was frequently encountered in children with FAP. Laxatives can be more effective than prokinetic drugs for relieving symptoms of FAP in children with a Leech score ≥ 8 and suspected OC.
Keyword
MeSH Terms
Figure
Reference
-
1. Hoekman DR, Rutten JM, Vlieger AM, Benninga MA, Dijkgraaf MG. Annual costs of care for pediatric irritable bowel syndrome, functional abdominal pain, and functional abdominal pain syndrome. J Pediatr. 2015; 167:1103–1108.e2.2. Bufler P, Gross M, Uhlig HH. Recurrent abdominal pain in childhood. Dtsch Arztebl Int. 2011; 108:295–304.3. Chiou FK, How CH, Ong C. Recurrent abdominal pain in childhood. Singapore Med J. 2013; 54:195–199.4. Chitkara DK, Rawat DJ, Talley NJ. The epidemiology of childhood recurrent abdominal pain in Western countries: a systematic review. Am J Gastroenterol. 2005; 100:1868–1875.5. Eidlitz-Markus T, Mimouni M, Zeharia A, Nussinovitch M, Amir J. Occult constipation: a common cause of recurrent abdominal pain in childhood. Isr Med Assoc J. 2004; 6:677–680.6. Freedman SB, Thull-Freedman J, Manson D, Rowe MF, Rumantir M, Eltorki M, Schuh S. Pediatric abdominal radiograph use, constipation, and significant misdiagnoses. J Pediatr. 2014; 164:83–88.e2.7. Gijsbers CF, Kneepkens CM, Schweizer JJ, Benninga MA, Büller HA. Recurrent abdominal pain in 200 children: somatic causes and diagnostic criteria. Acta Paediatr. 2011; 100:e208–14.8. Drossman DA. The functional gastrointestinal disorders and the Rome III process. Gastroenterology. 2006; 130:1377–1390.9. Jones MP, Dilley JB, Drossman D, Crowell MD. Brain-gut connections in functional GI disorders: anatomic and physiologic relationships. Neurogastroenterol Motil. 2006; 18:91–103.10. Levy RL, Olden KW, Naliboff BD, Bradley LA, Francisconi C, Drossman DA, Creed F. Psychosocial aspects of the functional gastrointestinal disorders. Gastroenterology. 2006; 130:1447–1458.11. Le Pluart D, Sabaté JM, Bouchoucha M, Hercberg S, Benamouzig R, Julia C. Functional gastrointestinal disorders in 35,447 adults and their association with body mass index. Aliment Pharmacol Ther. 2015; 41:758–767.12. Chang SH, Park KY, Kang SK, Kang KS, Na SY, Yang HR, Uhm JH, Ryoo E. Prevalence, clinical characteristics, and management of functional constipation at pediatric gastroenterology clinics. J Korean Med Sci. 2013; 28:1356–1361.13. Korterink JJ, Rutten JM, Venmans L, Benninga MA, Tabbers MM. Pharmacologic treatment in pediatric functional abdominal pain disorders: a systematic review. J Pediatr. 2015; 166:424–431.e6.14. Levy RL, van Tilburg MA. Functional abdominal pain in childhood: background studies and recent research trends. Pain Res Manag. 2012; 17:413–417.15. Gijsbers CF, Kneepkens CM, Vergouwe Y, Büller HA. Occult constipation: faecal retention as a cause of recurrent abdominal pain in children. Eur J Pediatr. 2014; 173:781–785.16. Treepongkaruna S, Simakachorn N, Pienvichit P, Varavithya W, Tongpenyai Y, Garnier P, Mathiex-Fortunet H. A randomised, double-blind study of polyethylene glycol 4000 and lactulose in the treatment of constipation in children. BMC Pediatr. 2014; 14:153.17. Leech SC, McHugh K, Sullivan PB. Evaluation of a method of assessing faecal loading on plain abdominal radiographs in children. Pediatr Radiol. 1999; 29:255–258.18. Tomlinson D, von Baeyer CL, Stinson JN, Sung L. A systematic review of faces scales for the self-report of pain intensity in children. Pediatrics. 2010; 126:e1168–98.19. Loening-Baucke V, Swidsinski A. Constipation as cause of acute abdominal pain in children. J Pediatr. 2007; 151:666–669.20. Koh H, Lee MJ, Kim MJ, Shin JI, Chung KS. Simple diagnostic approach to childhood fecal retention using the Leech score and Bristol stool form scale in medical practice. J Gastroenterol Hepatol. 2010; 25:334–338.21. van den Bosch M, Graafmans D, Nievelstein R, Beek E. Systematic assessment of constipation on plain abdominal radiographs in children. Pediatr Radiol. 2006; 36:224–226.22. Thompson WG, Longstreth GF, Drossman DA, Heaton KW, Irvine EJ, Müller-Lissner SA. Functional bowel disorders and functional abdominal pain. Gut. 1999; 45:Suppl 2. II43–7.23. Gieteling MJ, Bierma-Zeinstra SM, Passchier J, Berger MY. Prognosis of chronic or recurrent abdominal pain in children. J Pediatr Gastroenterol Nutr. 2008; 47:316–326.24. Burgers RE, Mugie SM, Chase J, Cooper CS, von Gontard A, Rittig CS, Homsy Y, Bauer SB, Benninga MA. Management of functional constipation in children with lower urinary tract symptoms: report from the Standardization Committee of the International Children’s Continence Society. J Urol. 2013; 190:29–36.25. Longo WE, Vernava AM 3rd. Prokinetic agents for lower gastrointestinal motility disorders. Dis Colon Rectum. 1993; 36:696–708.26. Raahave D. Faecal retention: a common cause in functional bowel disorders, appendicitis and haemorrhoids--with medical and surgical therapy. Dan Med J. 2015; 62:1–42.27. Mt-Isa S, Tomlin S, Sutcliffe A, Underwood M, Williamson P, Croft NM, Ashby D. Prokinetics prescribing in paediatrics: evidence on cisapride, domperidone, and metoclopramide. J Pediatr Gastroenterol Nutr. 2015; 60:508–514.28. Jeong SJ. Fecal retention in overactive bladder (OAB) in children: perspective of a pediatric gastroenterologist. Child Kidney Dis. 2015; 19:1–7.29. Burgers R, Liem O, Canon S, Mousa H, Benninga MA, Di Lorenzo C, Koff SA. Effect of rectal distention on lower urinary tract function in children. J Urol. 2010; 184:1680–1685.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pharmacological Management of Chronic Functional Constipation
- Comparison of polyethylene glycol 4000 and lactulose for treatment of chronic functional constipation in children
- Pharmacological treatment of chronic constipation: focused on oral laxatives
- Drug Therapy of Irritable Bowel Syndrome
- Treatment of Constipation