J Korean Neurosurg Soc.
2018 May;61(3):415-423. 10.3340/jkns.2017.0505.002.
Instrumentation Failure after Partial Corpectomy with Instrumentation of a Metastatic Spine
- Affiliations
-
- 1Department of Neurosurgery, Seoul National University Boramae Medical Center, Seoul, Korea.
- 2Department of Neurosurgery, Spine Center, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea.
- 3Department of Biostatistics, Seoul National University Boramae Medical Center, Seoul, Korea.
- 4Department of Neurosurgery, Seoul National University College of Medicine, Seoul, Korea. chungc@snu.ac.kr
- 5Clinical Research Institute, Seoul National University Hospital, Seoul, Korea.
- 6Neuroscience Research Institute, Seoul National University Medical Research Center, Seoul, Korea.
- 7Department of Brain and Cognitive Sciences, Seoul National University College of Natural Sciences, Seoul, Korea.
- KMID: 2417367
- DOI: http://doi.org/10.3340/jkns.2017.0505.002
Abstract
OBJECTIVE
To identify the perioperative factors associated with instrument failure in patients undergoing a partial corpectomy with instrumentation (PCI) for spinal metastasis.
METHODS
We assessed the one hundred twenty-four patients with who underwent PCI for a metastatic spine from 1987 to 2011. Outcome measure was the risk factor related to implantation failure. The preoperative factors analyzed were age, sex, ambulation, American Spinal Injury Association grade, bone mineral density, use of steroid, primary tumor site, number of vertebrae with metastasis, extra-bone metastasis, preoperative adjuvant chemotherapy, and preoperative spinal radiotherapy. The intraoperative factors were the number of fixed vertebrae, fixation in osteolytic vertebrae, bone grafting, and type of surgical approach. The postoperative factors included postoperative adjuvant chemotherapy and spinal radiotherapy. This study was supported by the National Research Foundation grant funded by government. There were no study-specific biases related to conflicts of interest.
RESULTS
There were 15 instrumentation failures (15/124, 12.1%). Preoperative ambulatory status and primary tumor site were not significantly related to the development of implant failure. There were no significant associations between insertion of a bone graft into the partial corpectomy site and instrumentation failure. The preoperative and operative factors analyzed were not significantly related to instrumentation failure. In univariable and multivariable analyses, postoperative spinal radiotherapy was the only significant variable related to instrumentation failure (p=0.049 and 0.050, respectively).
CONCLUSION
When performing PCI in patients with spinal metastasis followed by postoperative spinal radiotherapy, the surgeon may consider the possibility of instrumentation failure and find other strategies for augmentation than the use of a bone graft for fusion.
Keyword
MeSH Terms
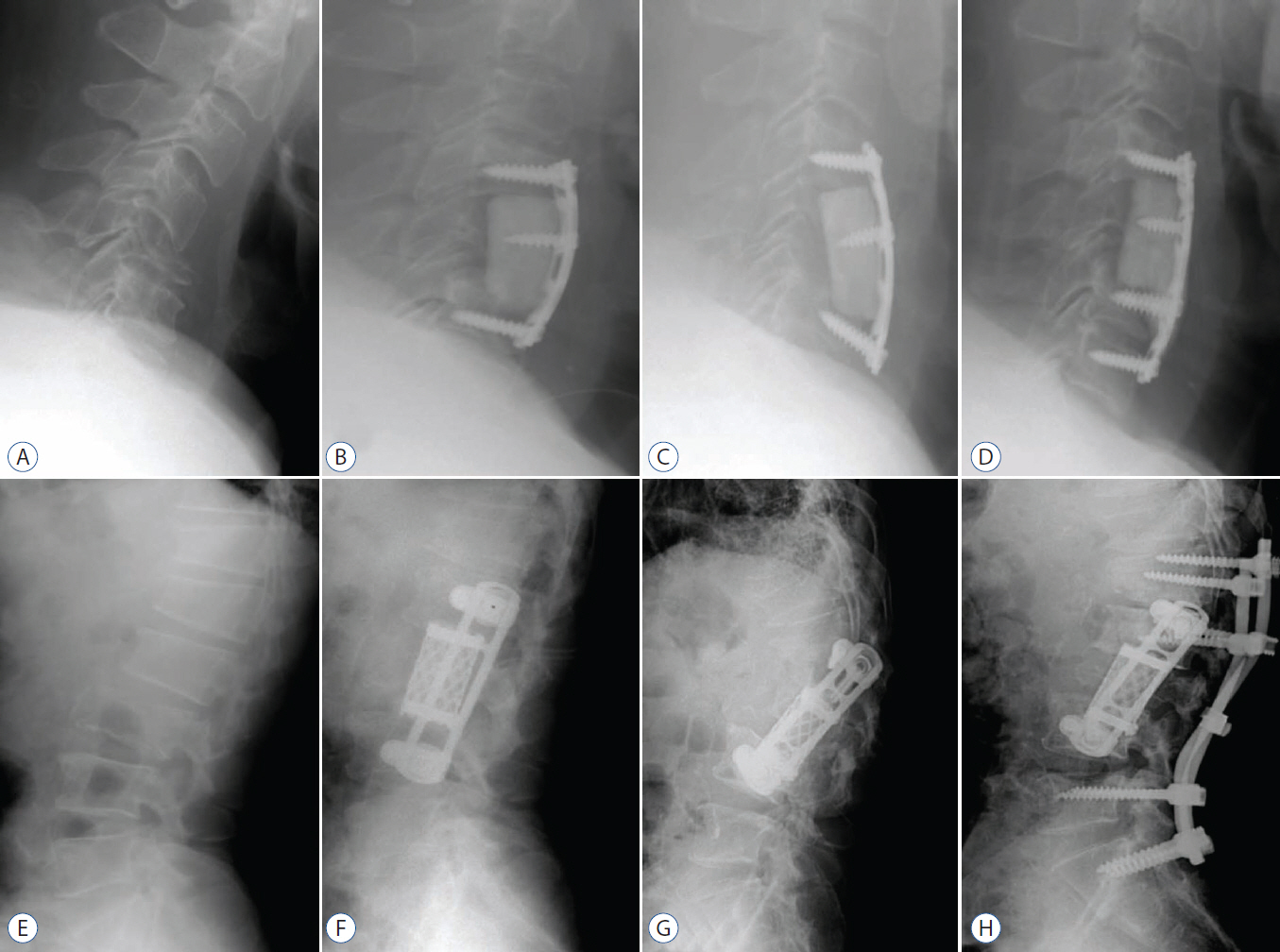
Figure
Reference
-
References
1. Bilsky MH, Laufer I, Burch S. Shifting paradigms in the treatment of metastatic spine disease. Spine (Phila Pa 1976). 34(22 Suppl):S101–S107. 2009.
Article2. Binning MJ, Gottfried ON, Klimo P Jr, Schmidt MH. Minimally invasive treatments for metastatic tumors of the spine. Neurosurg Clin N Am. 15:459–465. 2004.
Article3. Bouchard JA, Koka A, Bensusan JS, Stevenson S, Emery SE. Effects of irradiation on posterior spinal fusions. A rabbit model. Spine (Phila Pa 1976). 19:1836–1841. 1994.
Article4. Coleman RE, Rubens RD. The clinical course of bone metastases from breast cancer. Br J cancer. 55:61–66. 1987.
Article5. Emery SE, Brazinski MS, Koka A, Bensusan JS, Stevenson S. The biological and biomechanical effects of irradiation on anterior spinal bone grafts in a canine model. J Bone Joint Surg Am. 76:540–548. 1994.
Article6. Emery SE, Hughes SS, Junglas WA, Herrington SJ, Pathria MN. The fate of anterior vertebral bone grafts in patients irradiated for neoplasm. Clin Orthop Relat Res. (300):207–212. 1994.
Article7. Firth D. Bias reduction of maximum likelihood estimates. Biometrika. 80:27–38. 1993.
Article8. Gerszten PC, Welch WC. Current surgical management of metastatic spinal disease. Oncology (Williston Park). 14:1013–1024. discussion 1024, 1029-1030. 2000.9. Grant R, Papadopoulos SM, Greenberg HS. Metastatic epidural spinal cord compression. Neurol Clin. 9:825–841. 1991.
Article10. Harel R, Chao S, Krishnaney A, Emch T, Benzel EC, Angelov L. Spine instrumentation failure after spine tumor resection and radiation: comparing conventional radiotherapy with stereotactic radiosurgery outcomes. World Neurosurg. 74:517–522. 2010.
Article11. Hatrick NC, Lucas JD, Timothy AR, Smith MA. The surgical treatment of metastatic disease of the spine. Radiother Oncol. 56:335–339. 2000.
Article12. Jacobs WB, Perrin RG. Evaluation and treatment of spinal metastases: an overview. Neurosurg Focus. 11:e10. 2001.
Article13. Jung KW, Park S, Kong HJ, Won YJ, Lee JY, Park EC, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2008. Cancer Res Treat. 43:1–11. 2011.
Article14. Kim CH, Chung CK, Sohn S, Lee S, Park SB. Less invasive palliative surgery for spinal metastases. J Surg Oncol. 108:499–503. 2013.
Article15. Kim JM, Losina E, Bono CM, Schoenfeld AJ, Collins JE, Katz JN, et al. Clinical outcome of metastatic spinal cord compression treated with surgical excision ± radiation versus radiation therapy alone: a systematic review of literature. Spine (Phila Pa 1976). 37:78–84. 2012.
Article16. Klimo P Jr, Thompson CJ, Kestle JR, Schmidt MH. A meta-analysis of surgery versus conventional radiotherapy for the treatment of metastatic spinal epidural disease. Neuro Oncol. 7:64–76. 2005.
Article17. Kwok Y, Tibbs PA, Patchell RA. Clinical approach to metastatic epidural spinal cord compression. Hematol Oncol Clin North Am. 20:1297–1305. 2006.
Article18. Mantravadi RV, Skolnik EM, Applebaum EL. Complicationsof postoperative and preoperative radiation therapy in head and neck cancers. A comparative study. Arch Otolaryngol. 107:690–693. 1981.
Article19. Maranzano E, Trippa F, Chirico L, Basagni ML, Rossi R. Management of metastatic spinal cord compression. Tumori. 89:469–475. 2003.
Article20. Miller DJ, Lang FF, Walsh GL, Abi-Said D, Wildrick DM, Gokaslan ZL. Coaxial double-lumen methylmethacrylate reconstruction in the anterior cervical and upper thoracic spine after tumor resection. J Neurosurg. 92(2 Suppl):181–190. 2000.
Article21. Riseborough EJ. Irradiation induced kyphosis. Clin Orthop Relat Res. (128):101–106. 1977.
Article22. Roodman GD. Mechanisms of bone metastasis. N Engl J Med. 350:1655–1664. 2004.
Article23. Sohn S, Kim J, Chung CK, Lee NR, Park E, Chang UK, et al. A nationwide epidemiological study of newly diagnosed spine metastasis in the adult Korean population. Spine J. 16:937–945. 2016.
Article24. Sugimoto M, Takahashi S, Toguchida J, Kotoura Y, Shibamoto Y, Yamamuro T. Changes in bone after high-dose irradiation. Biomechanics and histomorphology. J Bone Joint Surg Br. 73:492–497. 1991.
Article25. Tomita K, Kawahara N, Kobayashi T, Yoshida A, Murakami H, Akamaru T. Surgical strategy for spinal metastases. Spine (Phila Pa 1976). 26:298–306. 2001.
Article26. Vrionis FD, Small J. Surgical management of metastatic spinal neoplasms. Neurosurg Focus. 15:E12. 2003.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of Unstable Fracture of the Thoracolumbar Spine Using Kaneda Instrumentation
- Segmental Spinal Instrumentation in the Management of Fracture and Fracture-Dislocation of the Thoraco-Lumbar Spine
- Pedicle Screw Nut Loosening: Potentially Avoidable Causes of Spine Instrumentation Failure
- Posterior Instrumentation of Thoracolumbar Fracture
- Harrington Instrumentation