J Korean Acad Prosthodont.
2018 Jul;56(3):199-205. 10.4047/jkap.2018.56.3.199.
Nonthermal plasma on the shear bond strength of relining resin to thermoplastic denture base resin
- Affiliations
-
- 1Institute for Clinical Dental Research, Korea University Guro Hospital, Seoul, Republic of Korea. wddc@korea.ac.kr
- KMID: 2416811
- DOI: http://doi.org/10.4047/jkap.2018.56.3.199
Abstract
- PURPOSE
This study evaluated the effect of nonthermal plasma treatment on the bond strength of autopolymerizing relining resin to the injection molded thermoplastic denture base resins (TDBRs) with different surface treatments.
MATERIALS AND METHODS
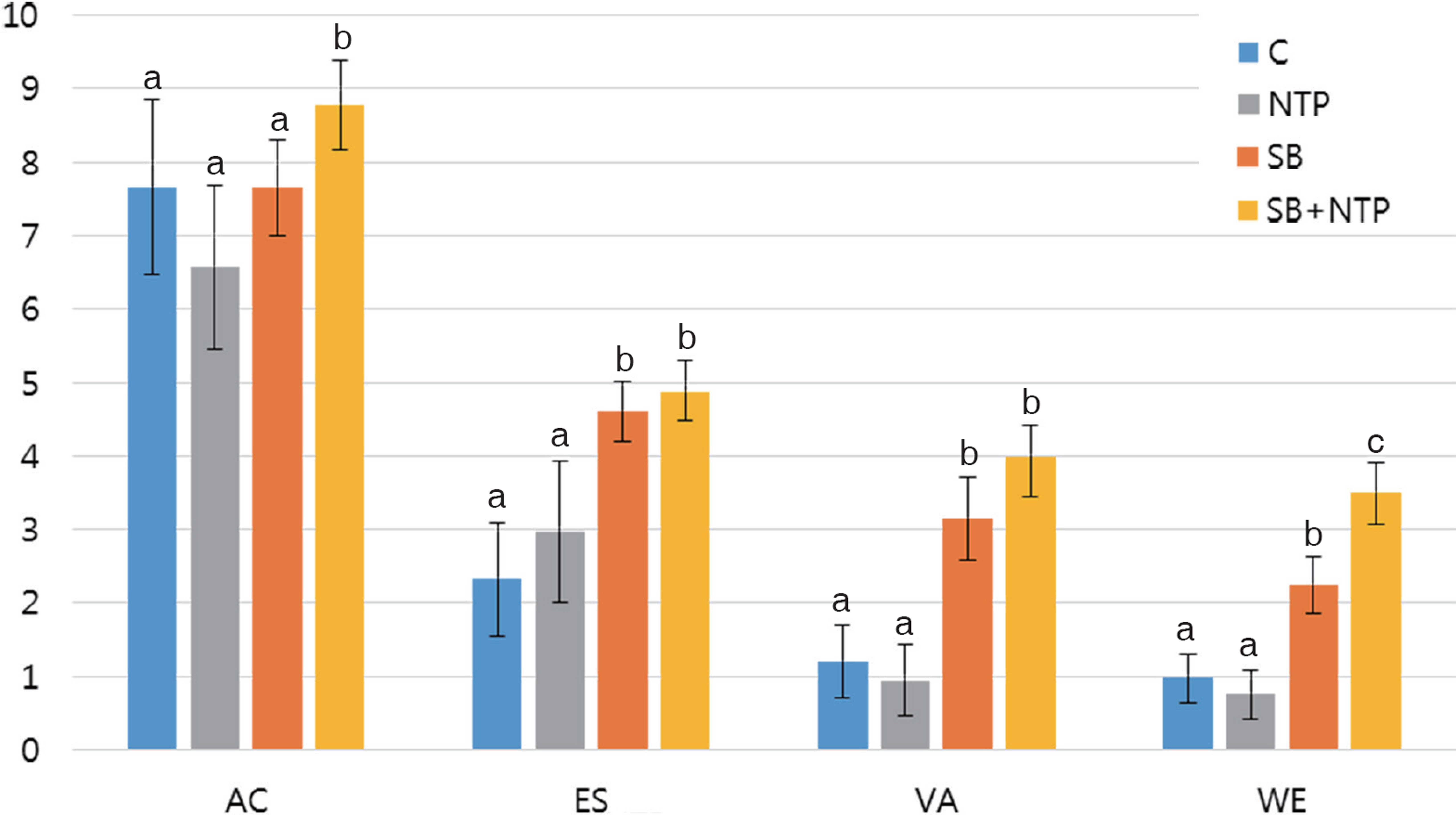
Acrylic Resin (Acrytone), Polyester (Estheshot-Bright), Polyamide (Valplast) and Polypropylene (Weldenz) were subjected to various surface treatments: No treatment, Nonthermal plasma, Sandblasting, Sandblasting and nonthermal plasma. Specimens were bonded using an autopolymerizing relining resin. Shear bond strength was tested using universal testing machine with crosshead speed of 1 mm/min. Statistical analysis by two-way analysis of variance with Tukey's test post hoc was used.
RESULTS
Acrytone showed significantly higher shear bond strength value among other TDBR group while Weldenz had the lowest. The sandblasting and nonthermal plasma condition had significantly higher shear bond strength value in all of the resin groups (P < .05).
CONCLUSION
The use of nonthermal plasma treatment showed limited effect on the shear bond strength between TDBRs and relining resin, and combination of nonthermal plasma and sandblasting improved the shear bond strength between TDBR and reline material.
Keyword
MeSH Terms
Figure
Reference
-
1.Fueki K., Ohkubo C., Yatabe M., Arakawa I., Arita M., Ino S., Kanamori T., Kawai Y., Kawara M., Komiyama O., Suzuki T., Nagata K., Hosoki M., Masumi S., Yamauchi M., Aita H., Ono T., Kondo H., Tamaki K., Matsuka Y., Tsukasaki H., Fujisawa M., Baba K., Koyano K., Yatani H. Clinical application of removable partial dentures using thermoplastic resin. Part II: Material properties and clinical features of non-metal clasp dentures. J Prosthodont Res. 2014. 58:71–84.
Article2.Takabayashi Y. Characteristics of denture thermoplastic resins for non-metal clasp dentures. Dent Mater J. 2010. 29:353–61.
Article3.Hamanaka I., Shimizu H., Takahashi Y. Bond strength of a chairside autopolymerizing reline resin to injection-molded thermoplastic denture base resins. J Prosthodont Res. 2017. 61:67–72.
Article4.Hargreaves AS. Nylon as a denture-base material. Dent Pract Dent Rec. 1971. 22:122–8.5.Stafford GD., Huggett R., MacGregor AR., Graham J. The use of nylon as a denture-base material. J Dent. 1986. 14:18–22.
Article6.Parvizi A., Lindquist T., Schneider R., Williamson D., Boyer D., Dawson DV. Comparison of the dimensional accuracy of injection-molded denture base materials to that of conventional pressure-pack acrylic resin. J Prosthodont. 2004. 13:83–9.
Article7.Yunus N., Rashid AA., Azmi LL., Abu-Hassan MI. Some ‡ex-ural properties of a nylon denture base polymer. J Oral Rehabil. 2005. 32:65–71.8.Katsumata Y., Hojo S., Ino S., Hamano N., Watanabe T., Suzuki Y., Ikeya H., Morino T., Toyoda M. Mechanical characterization of a ‡exible nylon denture base material. Bull Kanagawa Dent Col. 2007. 35:177–82.9.Koodaryan R., Hafezeqoran A. Effect of surface treatment methods on the shear bond strength of auto-polymerized resin to thermoplastic denture base polymer. J Adv Prosthodont. 2016. 8:504–10.
Article10.Kim JH., Choe HC., Son MK. Evaluation of adhesion of reline resins to the thermoplastic denture base resin for non-metal clasp denture. Dent Mater J. 2014. 33:32–8.
Article11.Brown HR. Adhesion of polymers. MRS Bull. 1996. 21:24–7.
Article12.Katsumata Y., Hojo S., Hamano N., Watanabe T., Yamaguchi H., Okada S., Teranaka T., Ino S. Bonding strength of autopolymerizing resin to nylon denture base polymer. Dent Mater J. 2009. 28:409–18.
Article13.Nishigawa G., Maruo Y., Oka M., Oki K., Minagi S., Okamoto M. Plasma treatment increased shear bond strength between heat cured acrylic resin and self-curing acrylic resin. J Oral Rehabil. 2003. 30:1081–4.
Article14.Hoffmann C., Berganza C., Zhang J. Cold Atmospheric Plasma: methods of production and application in dentistry and oncology. Med Gas Res. 2013. 3:21.
Article15.Chen M., Zhang Y., Sky Driver M., Caruso AN., Yu Q., Wang Y. Surface modification of several dental substrates by nonthermal, atmospheric plasma brush. Dent Mater. 2013. 29:871–80.
Article16.Yang YZ., Tian JM., Tian JT., Chen ZQ., Deng XJ., Zhang DH. Preparation of graded porous titanium coatings on titanium implant materials by plasma spraying. J Biomed Mater Res. 2000. 52:333–7.
Article17.Fischer H., Wirtz DC., Weber M., Neuss M., Niethard FU., Marx R. Improvement of the long-term adhesive strength between metal stem and polymethylmethacrylate bone cement by a silica/silane interlayer system. J Biomed Mater Res. 2001. 57:413–8.
Article18.Kim JH., Choe HC., Son MK. Evaluation of adhesion of reline resins to the thermoplastic denture base resin for non-metal clasp denture. Dent Mater J. 2014. 33:32–8.
Article19.Su N., Yue L., Liao Y., Liu W., Zhang H., Li X., Wang H., Shen J. The effect of various sandblasting conditions on surface changes of dental zirconia and shear bond strength between zirconia core and indirect composite resin. J Adv Prosthodont. 2015. 7:214–23.
Article20.Ozden N., Akaltan F., Suzer S., Akovali G. Time-related wettability characteristic of acrylic resin surfaces treated by glow discharge. J Prosthet Dent. 1999. 82:680–4.21.Jokinen V., Suvanto P., Franssila S. Oxygen and nitrogen plasma hydrophilization and hydrophobic recovery of polymers. Biomicro‡uidics. 2012. 6:16501–10.
Article22.Ozcan C., Zorlutuna P., Hasirci V., Hasirci N. In‡uence of oxygen plasma modification on surface free energy of PMMA fllms and cell attachment. Macromol Symp. 2008. 269:128–37.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A comparison study on shear bond strength of 3D printed resin and conventional heat-cured denture base resin to denture relining materials
- Comparison of shear bond strength between hard relining material and 3D-printing denture base resin containing silica micro-gel
- The Effects Of Thermocycling On The Bond Strength Between Cobalt-Chromium Alloy And Denture Base Resin
- A Study on the Bond Strength of Reline Resin to Pressure Injection Type Thermoplastic Denture Base Resin
- Effect of surface design on bond strength of relining denture resin