J Korean Soc Radiol.
2018 Aug;79(2):57-62. 10.3348/jksr.2018.79.2.57.
Comparison of CT Findings of Non-Tuberculous Mycobacterial Pulmonary Infection: Disease Stable versus Progressed Group
- Affiliations
-
- 1Department of Radiology, Kangwon National University Hospital, Chuncheon, Korea. hanheon@kangwon.ac.kr
- 2Department of Medicine, Hallym University Chuncheon Sacred Heart Hospital, Hallym University College of Medicine, Chuncheon, Korea.
- 3Department of Emergency Medicine, Kangwon National University Hospital, Chuncheon, Korea.
- KMID: 2416389
- DOI: http://doi.org/10.3348/jksr.2018.79.2.57
Abstract
- PURPOSE
To compare initial CT findings of non-tuberculous mycobacteria (NTM) pulmonary infection between stable and progressed groups and determine whether they could be used to predict disease prognosis and treatment response.
MATERIALS AND METHODS
From July 2006 to October 2013, 71 patients with NTM infection were retrospectively reviewed. Lung lesion pattern of CT finding, specific species, disease duration, and follow-up period were analyzed. These patients were classified into NTM stable (n = 46) and progressed (n = 25) groups.
RESULTS
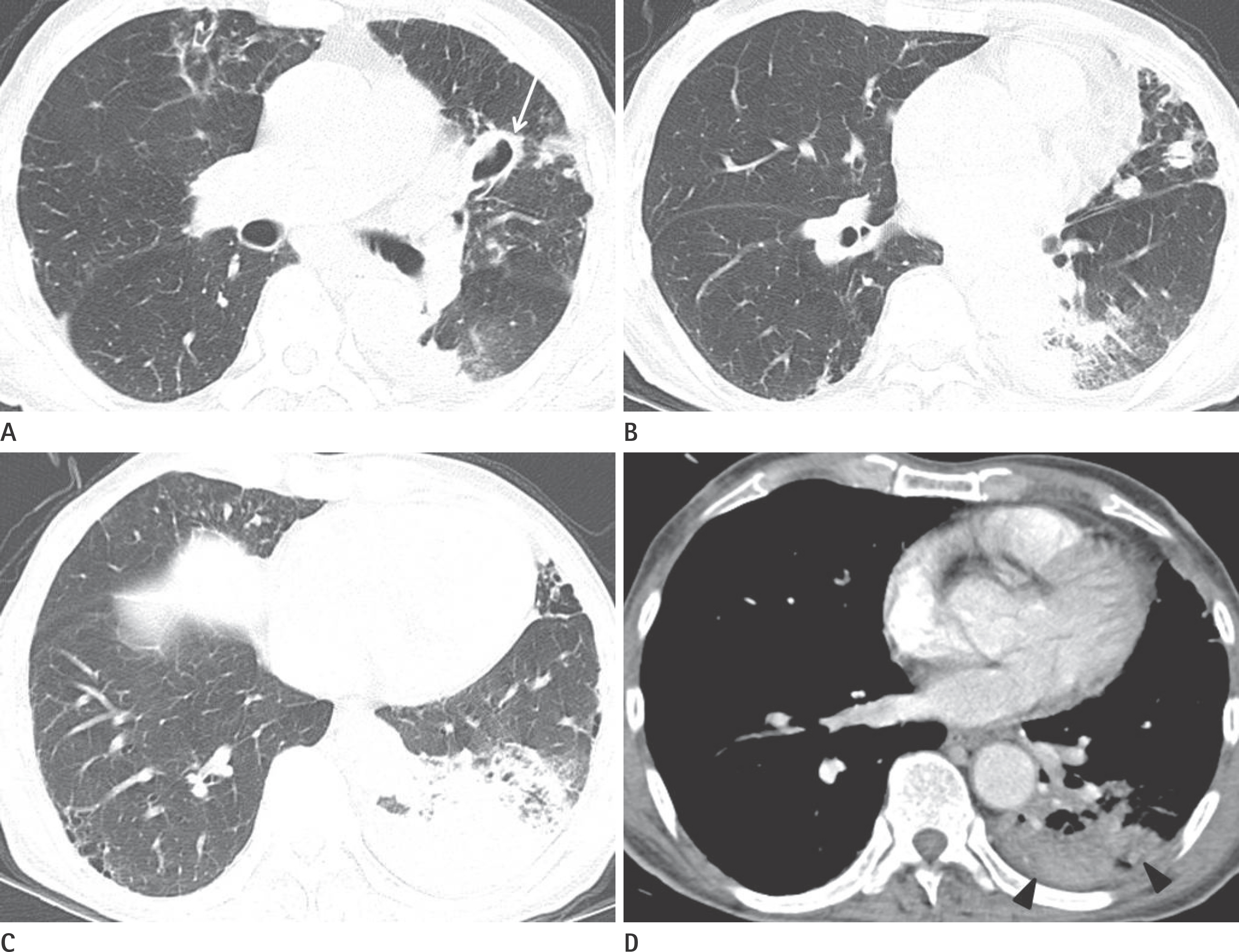
The most common CT findings of NTM infection were small nodules (n = 71, 100%) and bronchiectasis (n = 67, 94%). Large consolidation (> 2 cm, n = 34, 48%) and involvement of more than four lobes (n = 49, 69%) were also commonly observed. According to disease prognosis, large consolidation (n = 18, 72%, p = 0.003), cavitary lesion (n = 17, p = 0.002), and involvement of four or more lobes (n = 21, p = 0.044) on CT were significantly more frequent in disease progressed group than that in the stable group.
CONCLUSION
Among common CT findings of NTM disease, some CT findings such as large consolidation, cavitary lesion, and disease extent are good predictors of response to treatment in NTM pulmonary disease.
MeSH Terms
Figure
Reference
-
1.Glassroth J. Pulmonary disease due to nontuberculous mycobacteria. Chest. 2008. 133:243–251.
Article2.Gwak SH., Kim SJ., Cho BS., Jeon MH., Lee KM., Kim EY, et al. High resolution CT findings of nontuberculous mycobacterial pulmonary disease: comparison between the first treatment and the re-treatment group. J Korean Soc Radiol. 2012. 66:527–533.
Article3.O'Brien RJ., Geiter LJ., Snider DE Jr. The epidemiology of non-tuberculous mycobacterial diseases in the United States. Results from a national survey. Am Rev Respir Dis. 1987. 135:1007–1014.4.Koh WJ., Kwon OJ., Jeon K., Kim TS., Lee KS., Park YK, et al. Clinical significance of nontuberculous mycobacteria isolated from respiratory specimens in Korea. Chest. 2006. 129:341–348.
Article5.Jeong YJ., Lee KS., Koh WJ., Han J., Kim TS., Kwon OJ. Nontuberculous mycobacterial pulmonary infection in immunocompetent patients: comparison of thin-section CT and histopathologic findings. Radiology. 2004. 231:880–886.
Article6.Goo JM., Im JG. CT of tuberculosis and nontuberculous mycobacterial infections. Radiol Clin North Am. 2002. 40:73–87.
Article7.Griffith DE., Aksamit T., Brown-Elliott BA., Catanzaro A., Daley C., Gordin F, et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007. 175:367–416.
Article8.Han D., Lee KS., Koh WJ., Yi CA., Kim TS., Kwon OJ. Radiographic and CT findings of nontuberculous mycobacterial pulmonary infection caused by Mycobacterium abscessus. AJR Am J Roentgenol. 2003. 181:513–517.
Article9.Tanaka E., Kimoto T., Tsuyuguchi K., Watanabe I., Matsumoto H., Niimi A, et al. Effect of clarithromycin regimen for Mycobacterium avium complex pulmonary disease. Am J Respir Crit Care Med. 1999. 160:866–872.10.Kobashi Y., Matsushima T. The effect of combined therapy according to the guidelines for the treatment of Mycobacterium avium complex pulmonary disease. Intern Med. 2003. 42:670–675.
Article11.Kuroishi S., Nakamura Y., Hayakawa H., Shirai M., Nakano Y., Yasuda K, et al. Mycobacterium avium complex disease: prognostic implication of high-resolution computed tomography findings. Eur Respir J. 2008. 32:147–152.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Chronic Large Non Healing Ulcer: Non-Tuberculous Mycobacterial Infection of the Laryngopharynx
- A Case of Mediastinal Tuberculous Abscess and Lymphadenitis after Bone Marrow Transplantation
- Hepatic Tuberculous Abscess and Miliary Tuberculosis in A Hemodialysis Patient
- Radiologic Findings of Bronchiectasis: Tuberculous versus Non-Tuberculous
- Mycobacterium Szulgai Pulmonary Infection: Case Report of an Uncommon Pathogen in Korea