J Periodontal Implant Sci.
2018 Jun;48(3):164-173. 10.5051/jpis.2018.48.3.164.
Efficacy of an LED toothbrush on a Porphyromonas gingivalis biofilm on a sandblasted and acid-etched titanium surface: an in vitro study
- Affiliations
-
- 1Department of Periodontology and Research Institute of Oral Sciences, Gangneung-Wonju National University College of Dentistry, Gangneung, Korea. periojk@gwnu.ac.kr
- 2Department of Periodontology, Kyungpook National University School of Dentistry, Daegu, Korea.
- 3Department of Microbiology and Immunology and Research Institute of Oral Sciences, Gangneung-Wonju National University College of Dentistry, Gangneung, Korea.
- KMID: 2414929
- DOI: http://doi.org/10.5051/jpis.2018.48.3.164
Abstract
- PURPOSE
The aim of this study was to evaluate the antimicrobial effect of a newly devised toothbrush with light-emitting diodes (LEDs) on Porphyromonas gingivalis attached to sandblasted and acid-etched titanium surfaces.
METHODS
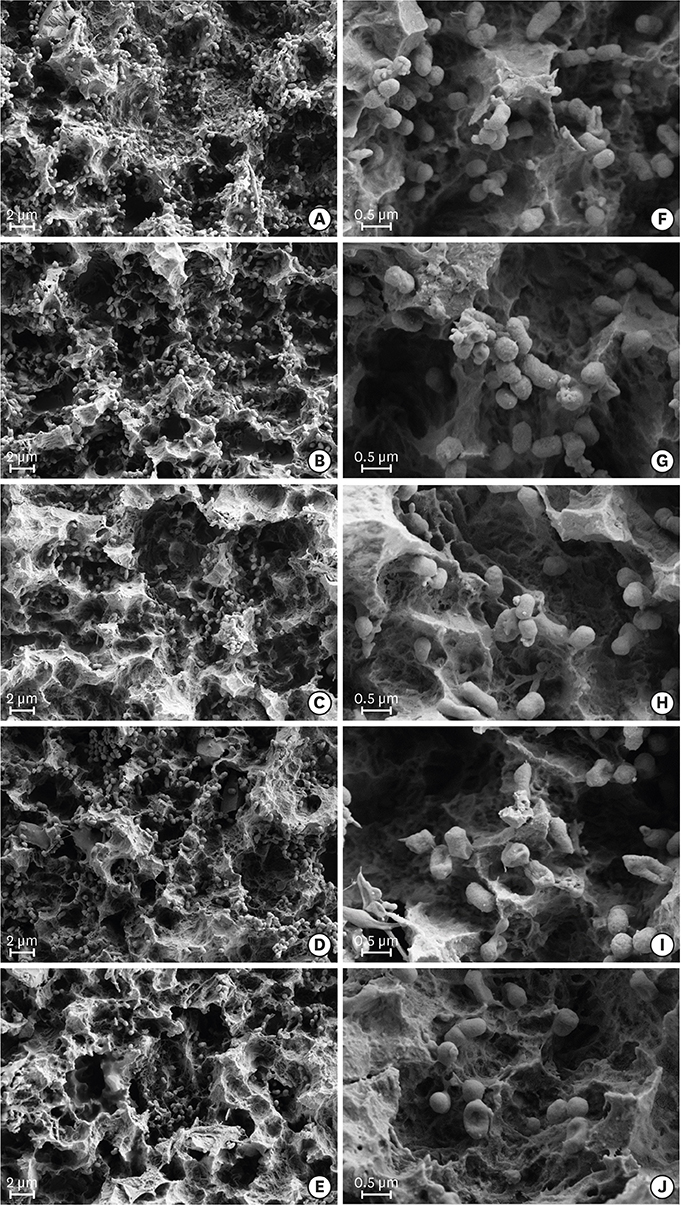
The study included a control group, a commercial photodynamic therapy (PDT) group, and 3 test groups (B, BL, and BLE). The disks in the PDT group were placed in methylene blue and then irradiated with a diode laser. The B disks were only brushed, the BL disks were brushed with an LED toothbrush, and the BLE disks were placed into erythrosine and then brushed with an LED toothbrush. After the different treatments, bacteria were detached from the disks and spread on selective agar. The number of viable bacteria and percentage of bacterial reduction were determined from colony counts. Scanning electron microscopy was performed to visualize bacterial alterations.
RESULTS
The number of viable bacteria in the BLE group was significantly lower than that in the other groups (P < 0.05). Scanning electron microscopy showed that bacterial cell walls were intact in the control and B groups, but changed after commercial PDT and LED exposure.
CONCLUSIONS
The findings suggest that an LED toothbrush with erythrosine treatment was more effective than a commercial PDT kit in reducing the number of P. gingivalis cells attached to surface-modified titanium in vitro.
MeSH Terms
Figure
Reference
-
1. Lindhe J, Meyle J; Group D of European Workshop on Periodontology. Peri-implant diseases: consensus report of the sixth European workshop on periodontology. J Clin Periodontol. 2008; 35:282–285.
Article2. Zitzmann NU, Berglundh T. Definition and prevalence of peri-implant diseases. J Clin Periodontol. 2008; 35:286–291.
Article3. Mombelli A, Müller N, Cionca N. The epidemiology of peri-implantitis. Clin Oral Implants Res. 2012; 23:Suppl 6. 67–76.
Article4. Figuero E, Graziani F, Sanz I, Herrera D, Sanz M. Management of peri-implant mucositis and peri-implantitis. Periodontol 2000. 2014; 66:255–273.
Article5. Mombelli A, Lang NP. The diagnosis and treatment of peri-implantitis. Periodontol 2000. 1998; 17:63–76.
Article6. Serino G, Ström C. Peri-implantitis in partially edentulous patients: association with inadequate plaque control. Clin Oral Implants Res. 2009; 20:169–174.
Article7. Sgolastra F, Petrucci A, Severino M, Gatto R, Monaco A. Periodontitis, implant loss and peri-implantitis. A meta-analysis. Clin Oral Implants Res. 2015; 26:e8–e16.
Article8. Dalago HR, Schuldt Filho G, Rodrigues MA, Renvert S, Bianchini MA. Risk indicators for Peri-implantitis. A cross-sectional study with 916 implants. Clin Oral Implants Res. 2017; 28:144–150.
Article9. Zhuang LF, Watt RM, Mattheos N, Si MS, Lai HC, Lang NP. Periodontal and peri-implant microbiota in patients with healthy and inflamed periodontal and peri-implant tissues. Clin Oral Implants Res. 2016; 27:13–21.
Article10. Socransky SS, Haffajee AD, Cugini MA, Smith C, Kent RL Jr. Microbial complexes in subgingival plaque. J Clin Periodontol. 1998; 25:134–144.
Article11. Pérez-Chaparro PJ, Duarte PM, Shibli JA, Montenegro S, Lacerda Heluy S, Figueiredo LC, et al. The Current Weight of Evidence of the Microbiologic Profile Associated With Peri-Implantitis: A Systematic Review. J Periodontol. 2016; 87:1295–1304.
Article12. Subramani K, Jung RE, Molenberg A, Hämmerle CH. Biofilm on dental implants: a review of the literature. Int J Oral Maxillofac Implants. 2009; 24:616–626.13. Kömerik N, Nakanishi H, MacRobert AJ, Henderson B, Speight P, Wilson M. In vivo killing of Porphyromonas gingivalis by toluidine blue-mediated photosensitization in an animal model. Antimicrob Agents Chemother. 2003; 47:932–940.
Article14. Wainwright M. Photodynamic antimicrobial chemotherapy (PACT). J Antimicrob Chemother. 1998; 42:13–28.
Article15. Alwaeli HA, Al-Khateeb SN, Al-Sadi A. Long-term clinical effect of adjunctive antimicrobial photodynamic therapy in periodontal treatment: a randomized clinical trial. Lasers Med Sci. 2015; 30:801–807.
Article16. Fukui M, Yoshioka M, Satomura K, Nakanishi H, Nagayama M. Specific-wavelength visible light irradiation inhibits bacterial growth of Porphyromonas gingivalis . J Periodontal Res. 2008; 43:174–178.
Article17. Feuerstein O, Persman N, Weiss EI. Phototoxic effect of visible light on Porphyromonas gingivalis and Fusobacterium nucleatum: an in vitro study. Photochem Photobiol. 2004; 80:412–415.
Article18. Song HH, Lee JK, Um HS, Chang BS, Lee SY, Lee MK. Phototoxic effect of blue light on the planktonic and biofilm state of anaerobic periodontal pathogens. J Periodontal Implant Sci. 2013; 43:72–78.
Article19. Teughels W, Van Assche N, Sliepen I, Quirynen M. Effect of material characteristics and/or surface topography on biofilm development. Clin Oral Implants Res. 2006; 17:Suppl 2. 68–81.
Article20. Bollen CM, Papaioanno W, Van Eldere J, Schepers E, Quirynen M, van Steenberghe D. The influence of abutment surface roughness on plaque accumulation and peri-implant mucositis. Clin Oral Implants Res. 1996; 7:201–211.
Article21. Berglundh T, Gotfredsen K, Zitzmann NU, Lang NP, Lindhe J. Spontaneous progression of ligature induced peri-implantitis at implants with different surface roughness: an experimental study in dogs. Clin Oral Implants Res. 2007; 18:655–661.
Article22. Louropoulou A, Slot DE, Van der Weijden F. The effects of mechanical instruments on contaminated titanium dental implant surfaces: a systematic review. Clin Oral Implants Res. 2014; 25:1149–1160.
Article23. Salvi GE, Ramseier CA. Efficacy of patient-administered mechanical and/or chemical plaque control protocols in the management of peri-implant mucositis. A systematic review. J Clin Periodontol. 2015; 42:Suppl 16. S187–S201.
Article24. Park JB, Koh M, Jang YJ, Choi BK, Kim KK, Ko Y. Removing bacteria from rough surface titanium discs with chlorhexidine and additional brushing with dentifrice. Gerodontology. 2016; 33:28–35.
Article25. Park JB, Kim N, Ko Y. Effects of ultrasonic scaler tips and toothbrush on titanium disc surfaces evaluated with confocal microscopy. J Craniofac Surg. 2012; 23:1552–1558.
Article26. Deppe H, Mücke T, Wagenpfeil S, Kesting M, Sculean A. Nonsurgical antimicrobial photodynamic therapy in moderate vs severe peri-implant defects: a clinical pilot study. Quintessence Int. 2013; 44:609–618.27. Okamoto K, Nakayama K, Kadowaki T, Abe N, Ratnayake DB, Yamamoto K. Involvement of a lysine-specific cysteine proteinase in hemoglobin adsorption and heme accumulation by Porphyromonas gingivalis . J Biol Chem. 1998; 273:21225–21231.
Article28. Smalley JW, Silver J, Marsh PJ, Birss AJ. The periodontopathogen Porphyromonas gingivalis binds iron protoporphyrin IX in the mu-oxo dimeric form: an oxidative buffer and possible pathogenic mechanism. Biochem J. 1998; 331:681–685.
Article29. Soukos NS, Som S, Abernethy AD, Ruggiero K, Dunham J, Lee C, et al. Phototargeting oral black-pigmented bacteria. Antimicrob Agents Chemother. 2005; 49:1391–1396.
Article30. Soukos NS, Stultz J, Abernethy AD, Goodson JM. Phototargeting human periodontal pathogens in vivo . Lasers Med Sci. 2015; 30:943–952.31. Habiboallah G, Mahdi Z, Mahbobeh NN, Mina ZJ, Sina F, Majid Z. Bactericidal effect of visible light in the presence of erythrosine on Porphyromonas gingivalis and Fusobacterium nucleatum compared with diode laser, an in vitro study. Laser Ther. 2014; 23:263–271.
Article32. Wang J, Liu Z, Liu J, Liu S, Shen W. Study on the interaction between fluoroquinolones and erythrosine by absorption, fluorescence and resonance Rayleigh scattering spectra and their application. Spectrochim Acta A Mol Biomol Spectrosc. 2008; 69:956–963.
Article33. Metcalf D, Robinson C, Devine D, Wood S. Enhancement of erythrosine-mediated photodynamic therapy of Streptococcus mutans biofilms by light fractionation. J Antimicrob Chemother. 2006; 58:190–192.
Article34. Fekrazad R, Mirmoezzi A, Kalhori KA, Arany P. The effect of red, green and blue lasers on healing of oral wounds in diabetic rats. J Photochem Photobiol B. 2015; 148:242–245.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The bactericidal effect of an atmospheric-pressure plasma jet on Porphyromonas gingivalis biofilms on sandblasted and acid-etched titanium discs
- Fusobacterium nucleatum modulates serum binding to Porphyromonas gingivalis biofilm
- The effect of pretreating resorbable blast media titanium discs with an ultrasonic scaler or toothbrush on the bacterial removal efficiency of brushing
- Perturbation of host responses by Porphyromonas gingivalis biofilm
- T lymphocyte response to periodontal complex bacterial biofilm