Ann Surg Treat Res.
2018 Jun;94(6):330-336. 10.4174/astr.2018.94.6.330.
Assessment of functional defecation disorders using anorectal manometry
- Affiliations
-
- 1Department of Surgery, Konkuk University School of Medicine, Seoul, Korea. recto@kuh.ac.kr
- KMID: 2412403
- DOI: http://doi.org/10.4174/astr.2018.94.6.330
Abstract
- PURPOSE
The aim was to evaluate the discriminating accuracy of anorectal manometry (ARM) between nonconstipated (NC) subjects and functionally constipated (FC) subjects, and between FC subjects with and without functional defecation disorder (FDD).
METHODS
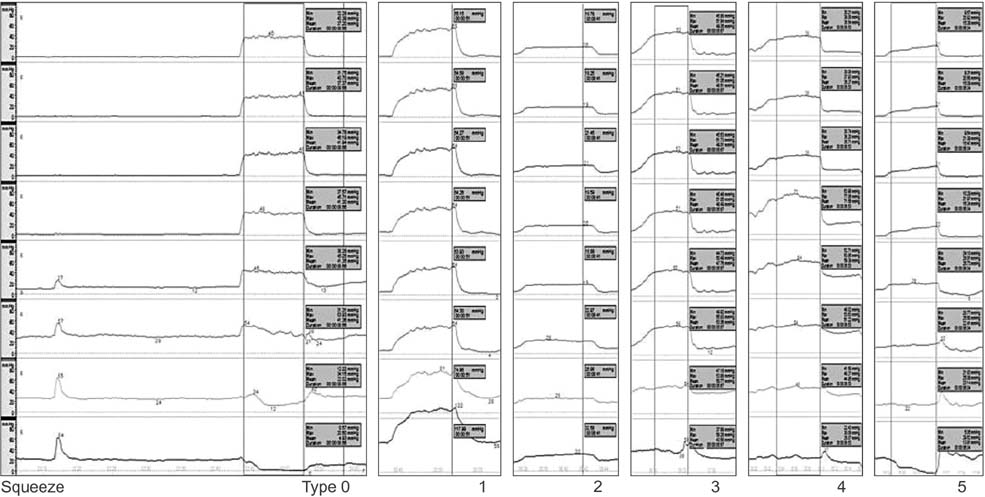
Among female patients who visited anorectal physiology unit, those who could be grouped to following categories were included; FC group with FDD (+FDD subgroup), or without FDD (−FDD subgroup) and NC group. ARM was performed and interpreted not only with absolute pressure values, but also pattern classification and quantification of pressure changes in the rectum and anus during attempted defecation.
RESULTS
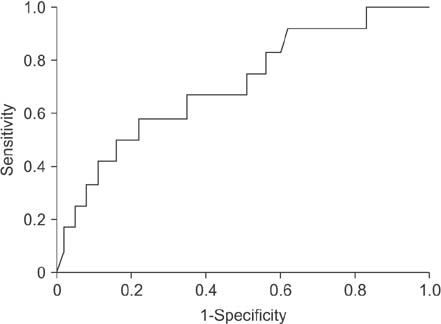
There were 76 subjects in NC group and 75 in FC group. Among FC group, 63 subjects were in −FDD subgroup and 12 in +FDD subgroup. In pattern classification of pressure changes, type 0, as "˜normal' response, was only slightly more prevalent in NC group than in FC group. When all "˜abnormal' types (types 1-5) were considered together as positive findings, the sensitivity and specificity of pattern classification in diagnosing FC among all subjects were 89.3% and 22.7%. Those values in diagnosing FDD among FC group were 91.7% and 11.1%. Manometric defecation index (MDI) as a quantification parameter was significantly different between −FDD and +FDD subgroups. Other conventional absolute pressures were mostly comparable between the groups.
CONCLUSION
Among all parameters of ARM, MDI was useful to diagnose FDD in FC patients. Other parameters including the pattern classification were questionable in their ability to diagnose FDD.
Keyword
MeSH Terms
Figure
Reference
-
1. Rome Foundation. Rome III disorders and criteria [Internet]. Raleigh (NC): Rome Foundation Inc.;c2015. cited 2015 May 10. Available from: http://www.romecriteria.org/criteria.2. Dixon T. Obstucted defecation: a pathophysiologic approach. In : Lindsey I, Nugent K, Dixon T, editors. Pelvic floor disorders. New York: Oxford University Press Inc.;2011. p. 57.3. Irvine EJ, Ferrazzi S, Pare P, Thompson WG, Rance L. Health-related quality of life in functional GI disorders: focus on constipation and resource utilization. Am J Gastroenterol. 2002; 97:1986–1993.
Article4. Heymen S, Scarlett Y, Jones K, Ringel Y, Drossman D, Whitehead WE. Randomized, controlled trial shows biofeedback to be superior to alternative treatments for patients with pelvic floor dyssynergia-type constipation. Dis Colon Rectum. 2007; 50:428–441.
Article5. Chiarioni G, Whitehead WE, Pezza V, Morelli A, Bassotti G. Biofeedback is superior to laxatives for normal transit constipation due to pelvic floor dyssynergia. Gastroenterology. 2006; 130:657–664.
Article6. Rao SS, Valestin J, Brown CK, Zimmerman B, Schulze K. Long-term efficacy of biofeedback therapy for dyssynergic defecation: randomized controlled trial. Am J Gastroenterol. 2010; 105:890–896.
Article7. American Gastroenterological Association. Bharucha AE, Dorn SD, Lembo A, Pressman A. American Gastroenterological Association medical position statement on constipation. Gastroenterology. 2013; 144:211–217.
Article8. Rao SS. Dyssynergic defecation. Gastroenterol Clin North Am. 2001; 30:97–114.
Article9. Rao SS. Dyssynergic defecation and biofeedback therapy. Gastroenterol Clin North Am. 2008; 37:569–586.
Article10. Noelting J, Ratuapli SK, Bharucha AE, Harvey DM, Ravi K, Zinsmeister AR. Normal values for high-resolution anorectal manometry in healthy women: effects of age and significance of rectoanal gradient. Am J Gastroenterol. 2012; 107:1530–1536.
Article11. Ratuapli SK, Bharucha AE, Noelting J, Harvey DM, Zinsmeister AR. Phenotypic identification and classification of functional defecatory disorders using high-resolution anorectal manometry. Gastroenterology. 2013; 144:314–322.e2.
Article12. Grossi U, Carrington EV, Bharucha AE, Horrocks EJ, Scott SM, Knowles CH. Diagnostic accuracy study of anorectal manometry for diagnosis of dyssynergic defecation. Gut. 2016; 65:447–455.
Article13. Rao SS, Welcher KD, Leistikow JS. Obstructive defecation: a failure of rectoanal coordination. Am J Gastroenterol. 1998; 93:1042–1050.
Article14. Seong MK, Kim TW. Significance of defecographic parameters in diagnosing pelvic floor dyssynergia. J Korean Surg Soc. 2013; 84:225–230.
Article15. Staller K. Role of Anorectal manometry in clinical practice. Curr Treat Options Gastroenterol. 2015; 13:418–431.
Article16. Rao SS, Mudipalli RS, Stessman M, Zimmerman B. Investigation of the utility of colorectal function tests and Rome II criteria in dyssynergic defecation (Anismus). Neurogastroenterol Motil. 2004; 16:589–596.
Article17. Bharucha AE, Wald A, Enck P, Rao S. Functional anorectal disorders. Gastroenterology. 2006; 130:1510–1518.
Article18. Bharucha AE, Fletcher JG, Seide B, Riederer SJ, Zinsmeister AR. Phenotypic variation in functional disorders of defecation. Gastroenterology. 2005; 128:1199–1210.
Article19. Videlock EJ, Lembo A, Cremonini F. Diagnostic testing for dyssynergic defecation in chronic constipation: meta-analysis. Neurogastroenterol Motil. 2013; 25:509–520.
Article20. Sauter M, Heinrich H, Fox M, Misselwitz B, Halama M, Schwizer W, et al. Toward more accurate measurements of anorectal motor and sensory function in routine clinical practice: validation of high-resolution anorectal manometry and Rapid Barostat Bag measurements of rectal function. Neurogastroenterol Motil. 2014; 26:685–695.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- High-resolution anorectal manometry in children
- Comparison of High-resolution Anorectal Manometry With Water-perfused Anorectal Manometry
- How to Interpret Conventional Anorectal Manometry
- Is High-resolution Anorectal Pressure Topography More Useful Than Wave Manometry in Dyssynergic Defecation?
- High-resolution Anorectal Manometry in the Diagnosis of Functional Defecation Disorder in Patients With Functional Constipation: A Retrospective Cohort Study