Clin Orthop Surg.
2017 Mar;9(1):63-70. 10.4055/cios.2017.9.1.63.
Radiological Parameters of Undegenerated Cervical Vertebral Segments in a Korean Population
- Affiliations
-
- 1Department of Orthopedic Surgery, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Yangsan, Korea.
- 2Elim Orthopedic Clinic, Anyang, Korea.
- 3Department of Orthopedic Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. dlee@amc.seoul.kr
- KMID: 2412305
- DOI: http://doi.org/10.4055/cios.2017.9.1.63
Abstract
- BACKGROUND
Several scoring systems for cervical disc and facet joint degeneration, using radiography or computed tomography, have been developed and tested for reliability. However, definitions of disc height and facet joint space narrowing vary. To our knowledge, no study has reported quantitative data for normal radiologic values of the cervical spine in the Korean population. The purpose of this study is to determine normal cervical disc height, disc height ratio, and facet joint space values, and investigate the correlation between demographic data and these values.
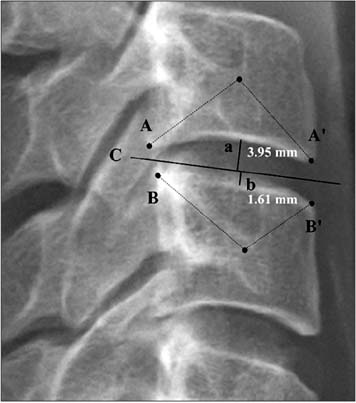
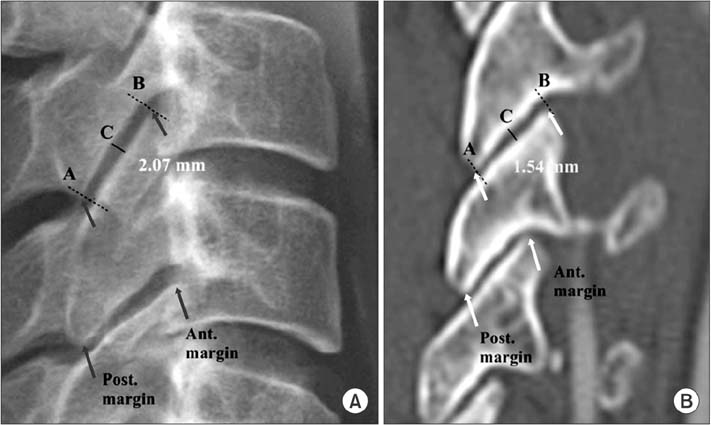
METHODS
We performed a retrospective study of patients who underwent artificial disc replacement of the cervical spine. Disc heights and facet joint spaces were measured using cervical neutral lateral radiographs and computed tomography. The means, standard deviations, and 95% confidence intervals of the values were determined.
RESULTS
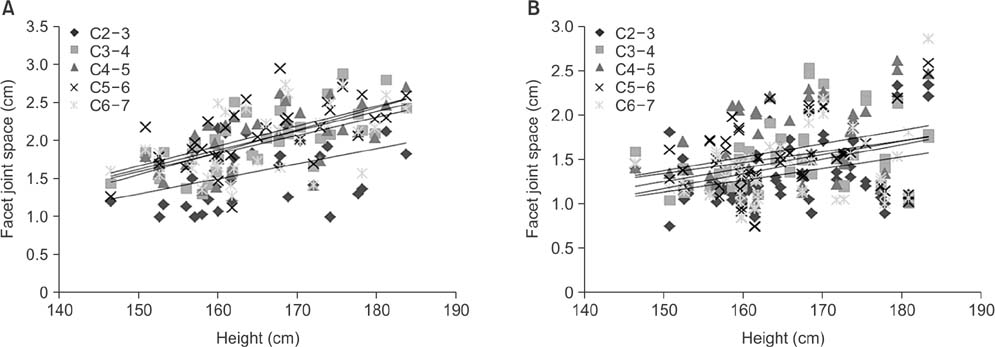
We measured 148 intervertebral discs and 352 posterior facet joints. The mean disc height measured by plain radiography and computed tomography was 5.57 ± 0.81 mm and 4.94 ± 0.94 mm, respectively. The mean facet joint space values measured by plain radiography and computed tomography were 1.94 ± 0.45 mm and 1.43 ± 0.39 mm, respectively. The disc heights and facet joint space values measured by plain radiography were greater than those measured by computed tomography. The lower limit of the 95% confidence interval of the disc height ratio calculated by plain radiography and computed tomography was greater than 0.94 at all levels except for C5-6. Patient height and disc height showed a tendency of positive correlation.
CONCLUSIONS
In a Korean population, the normal cervical disc height was about 5.0 mm and the normal facet joint space was 1.4 mm. Disc height ratio can reliably identify normal cervical disc height in patients with mild degeneration. Patient height was positively correlated with disc height and facet joint space. Thus, when selecting a cervical implant, surgeons should consider patient height as well as estimated normal disc height.
MeSH Terms
-
Adult
Body Height
Cervical Vertebrae/anatomy & histology/*diagnostic imaging
Female
Humans
Intervertebral Disc/anatomy & histology/*diagnostic imaging
Male
Middle Aged
Reference Standards
Republic of Korea
Retrospective Studies
Tomography, X-Ray Computed
Zygapophyseal Joint/anatomy & histology/*diagnostic imaging
Figure
Reference
-
1. Szpalski M, Gunzburg R, Mayer M. Spine arthroplasty: a historical review. Eur Spine J. 2002; 11:Suppl 2. S65–S84.
Article2. Cote P, Cassidy JD, Yong-Hing K, Sibley J, Loewy J. Apophysial joint degeneration, disc degeneration, and sagittal curve of the cervical spine: can they be measured reliably on radiographs? Spine (Phila Pa 1976). 1997; 22(8):859–864.3. Kellgren JH, Jeffrey MR, Ball J. The epidemiology of chronic rheumatism: atlas of standard radiographs of arthritis. Oxford: Blackwell Scientific;1963.4. Walraevens J, Liu B, Meersschaert J, et al. Qualitative and quantitative assessment of degeneration of cervical intervertebral discs and facet joints. Eur Spine J. 2009; 18(3):358–369.
Article5. Kettler A, Wilke HJ. Review of existing grading systems for cervical or lumbar disc and facet joint degeneration. Eur Spine J. 2006; 15(6):705–718.
Article6. Kettler A, Rohlmann F, Neidlinger-Wilke C, Werner K, Claes L, Wilke HJ. Validity and interobserver agreement of a new radiographic grading system for intervertebral disc degeneration: part II. cervical spine. Eur Spine J. 2006; 15(6):732–741.
Article7. Shigematsu H, Koizumi M, Yoneda M, Iida J, Oshima T, Tanaka Y. Magnification error in digital radiographs of the cervical spine against magnetic resonance imaging measurements. Asian Spine J. 2013; 7(4):267–272.
Article8. Frobin W, Leivseth G, Biggemann M, Brinckmann P. Vertebral height, disc height, posteroanterior displacement and dens-atlas gap in the cervical spine: precision measurement protocol and normal data. Clin Biomech (Bristol, Avon). 2002; 17(6):423–431.
Article9. Christe A, Laubli R, Guzman R, et al. Degeneration of the cervical disc: histology compared with radiography and magnetic resonance imaging. Neuroradiology. 2005; 47(10):721–729.
Article10. Lehto IJ, Tertti MO, Komu ME, Paajanen HE, Tuominen J, Kormano MJ. Age-related MRI changes at 0.1 T in cervical discs in asymptomatic subjects. Neuroradiology. 1994; 36(1):49–53.
Article11. Kolstad F, Myhr G, Kvistad KA, Nygaard OP, Leivseth G. Degeneration and height of cervical discs classified from MRI compared with precise height measurements from radiographs. Eur J Radiol. 2005; 55(3):415–420.
Article12. Viikari-Juntura E, Raininko R, Videman T, Porkka L. Evaluation of cervical disc degeneration with ultralow field MRI and discography: an experimental study on cadavers. Spine (Phila Pa 1976). 1989; 14(6):616–619.
Article13. Miyazaki M, Hong SW, Yoon SH, Morishita Y, Wang JC. Reliability of a magnetic resonance imaging-based grading system for cervical intervertebral disc degeneration. J Spinal Disord Tech. 2008; 21(4):288–292.
Article14. Mimura M, Panjabi MM, Oxland TR, Crisco JJ, Yamamoto I, Vasavada A. Disc degeneration affects the multidirectional flexibility of the lumbar spine. Spine (Phila Pa 1976). 1994; 19(12):1371–1380.
Article15. Rampersaud R, Fehlings M, Harrop J, et al. Validation of digital radiology measurement tools for quantitative spinal imaging. Top Spinal Cord Inj Rehabil. 2006; 12(1):11–21.
Article16. Yukawa Y, Kato F, Suda K, Yamagata M, Ueta T. Age-related changes in osseous anatomy, alignment, and range of motion of the cervical spine: part I. radiographic data from over 1,200 asymptomatic subjects. Eur Spine J. 2012; 21(8):1492–1498.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Vertebral Spreading Segments of Cervical Epidural Injection: a Comparative Study with 5 ml and 10 ml of Injected Volume
- Review of Radiological Parameters, Imaging Characteristics, and Their Effect on Optimal Treatment Approaches and Surgical Outcomes for Cervical Ossification of the Posterior Longitudinal Ligament
- Radiologic Changes of Operated and Adjacent Segments after Anterior Cervical Microforaminotomy
- Morphometric Relationship between the Cervicothoracic Cord Segments and Vertebral Bodies
- Comparative Analysis of Three Different Cervical Lateral Mass Screw Fixation Techniques by Complications and Bicortical Purchase : Cadaveric Study