Clin Orthop Surg.
2017 Sep;9(3):280-285. 10.4055/cios.2017.9.3.280.
Tibial Base Plate for Total Knee Arthroplasty: Symmetric or Asymmetric?
- Affiliations
-
- 1Department of Orthopedics and Traumatology, Yildirim Beyazit University Faculty of Medicine, Ankara, Turkey. nmbozkurt@gmail.com
- 2Department of Orthopaedics and Traumatology, Yenimahalle Training and Research Hospital, Yildirim Beyazit University, Ankara, Turkey.
- 3Department of Orthopedics and Traumatology, Izmir Atatürk Training and Research Hospital, Katip Celebi University, Izmir, Turkey.
- KMID: 2412263
- DOI: http://doi.org/10.4055/cios.2017.9.3.280
Abstract
- BACKGROUND
Ideal positioning and best coverage of the tibial base plate are essential in total knee arthroplasty. There are 2 types of tibial base plates: symmetric and asymmetric. The superiority of one to the other is still controversial. The aim of this study was to compare symmetric and asymmetric tibial base plates for total knee arthroplasty in terms of rotational alignment and coverage.
METHODS
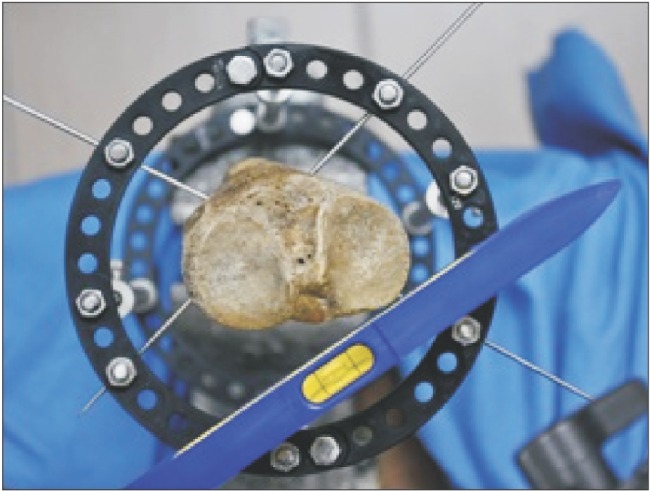
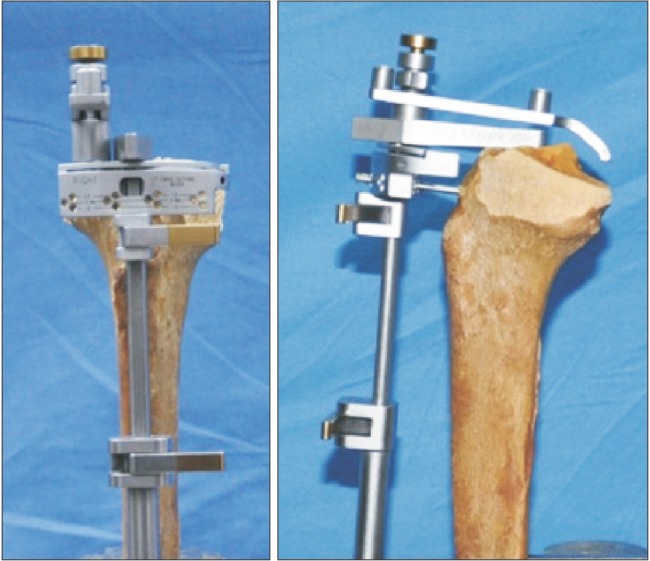
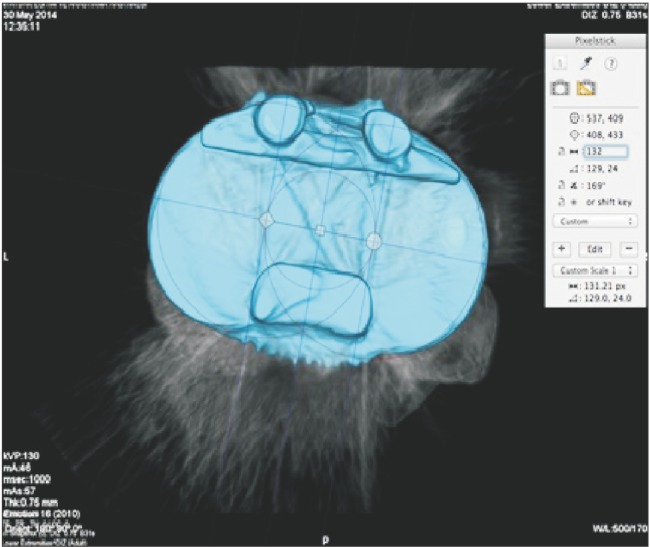
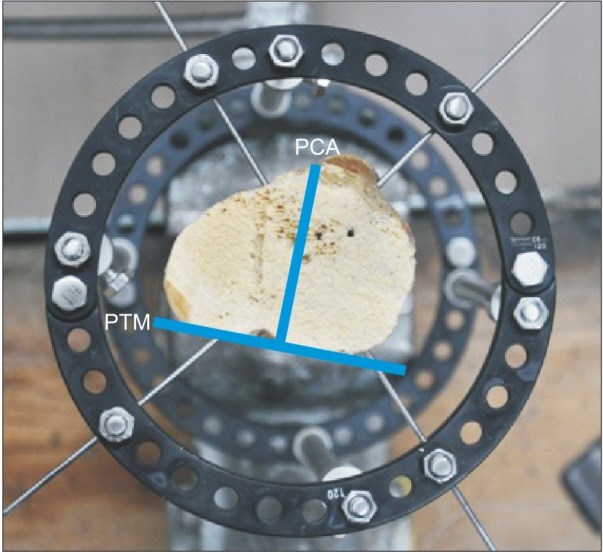
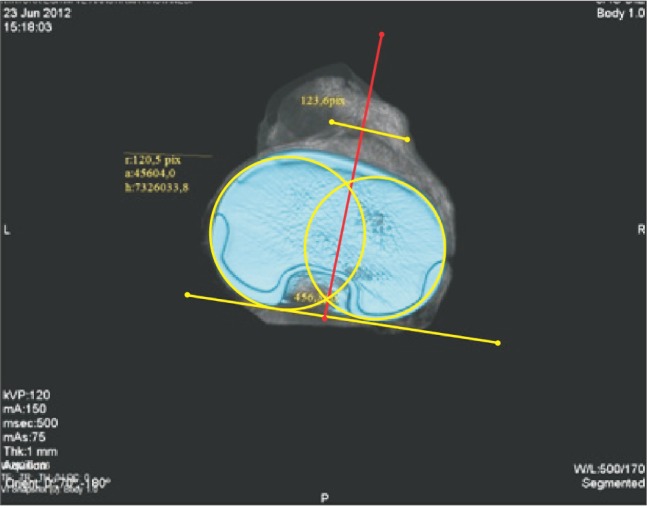
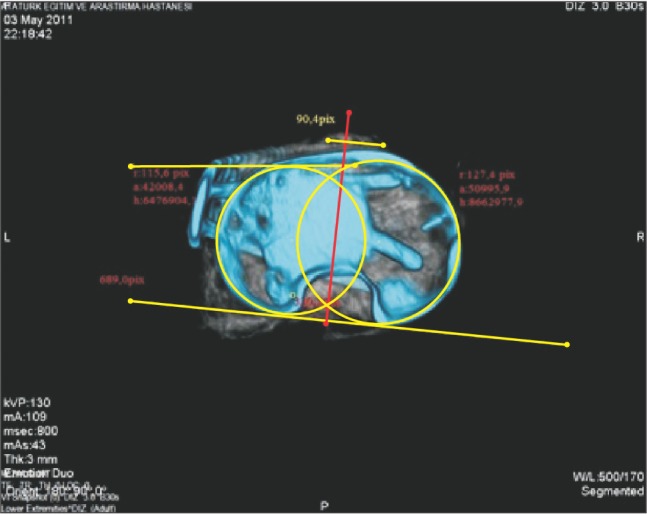
The study was conducted on a total of 80 cadaveric tibial bones. Two surgeons were asked to place 20 symmetric (group 1) and 20 asymmetric (group 2) tibial base plates taking care to ensure the best coverage that they were able to determine. Afterwards, the rotational errors and coverage were assessed with reference to the posterior tibial margin and posterior condylar axis on the three-dimensional computed tomography (3D CT) scan. In the second part of the study, the surgeons were asked to place 20 symmetric (group 3) and 20 asymmetric (group 4) base plates taking care to ensure the best rotational alignment. The rotational errors and the areas uncovered or overstuffed after the application were measured on the 3D CT scan.
RESULTS
On the comparison of rotational errors, while there was no significant difference between group 1 and group 2 in terms of coverage (p = 0.624), the mean external rotation error was significantly greater in group 2 (p = 0.034). On the comparison of coverage, while there was no significant difference between group 3 and group 4 in terms of rotation (p = 0.36), the mean ratios of the uncovered tibial surface to the total tibial surface (p = 0.041) and also the overstuffed area to the total base plate surface (p = 0.029) were significantly greater in group 4.
CONCLUSIONS
The determination of correct size and rotation of the tibial component is essential for favorable outcomes of total knee arthroplasty. In this study, the symmetric tibial base plate design was more effective than the asymmetric design in providing the ideal tibial rotation and coverage.
Keyword
MeSH Terms
Figure
Reference
-
1. Abram SG, Marsh AG, Brydone AS, Nicol F, Mohammed A, Spencer SJ. The effect of tibial component sizing on patient reported outcome measures following uncemented total knee replacement. Knee. 2014; 21(5):955–959. PMID: 25017484.
Article2. Clary C, Aram L, Deffenbaugh D, Heldreth M. Tibial base design and patient morphology affecting tibial coverage and rotational alignment after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2014; 22(12):3012–3018. PMID: 25358691.
Article3. Bell SW, Young P, Drury C, et al. Component rotational alignment in unexplained painful primary total knee arthroplasty. Knee. 2014; 21(1):272–277. PMID: 23140906.
Article4. Watanabe S, Sato T, Omori G, Koga Y, Endo N. Change in tibiofemoral rotational alignment during total knee arthroplasty. J Orthop Sci. 2014; 19(4):571–578. PMID: 24817492.
Article5. Kwak DS, Surendran S, Pengatteeri YH, et al. Morphometry of the proximal tibia to design the tibial component of total knee arthroplasty for the Korean population. Knee. 2007; 14(4):295–300. PMID: 17600719.
Article6. Bonnin MP, Saffarini M, Mercier PE, Laurent JR, Carrillon Y. Is the anterior tibial tuberosity a reliable rotational landmark for the tibial component in total knee arthroplasty? J Arthroplasty. 2011; 26(2):260–267. 267.e1–267.e2. PMID: 20452177.7. Greenberg RL, Kenna RV, Hungerford DS, Krackow KA. Instrumentation for total knee arthroplasty. In : Hungerford DS, Krackow KA, Kenna RV, editors. Total knee arthroplasty: a comprehensive approach. Baltimore, MD: Williams & Wilkins;1984. p. 35–70.8. Dai Y, Scuderi GR, Bischoff JE, Bertin K, Tarabichi S, Rajgopal A. Anatomic tibial component design can increase tibial coverage and rotational alignment accuracy: a comparison of six contemporary designs. Knee Surg Sports Traumatol Arthrosc. 2014; 22(12):2911–2923. PMID: 25217314.
Article9. Martin S, Saurez A, Ismaily S, Ashfaq K, Noble P, Incavo SJ. Maximizing tibial coverage is detrimental to proper rotational alignment. Clin Orthop Relat Res. 2014; 472(1):121–125. PMID: 23653101.
Article10. Mahoney OM, Kinsey T. Overhang of the femoral component in total knee arthroplasty: risk factors and clinical consequences. J Bone Joint Surg Am. 2010; 92(5):1115–1121. PMID: 20439656.
Article11. Petersen W, Rembitzki IV, Bruggemann GP, et al. Anterior knee pain after total knee arthroplasty: a narrative review. Int Orthop. 2014; 38(2):319–328. PMID: 24057656.
Article12. Mandalia V, Eyres K, Schranz P, Toms AD. Evaluation of patients with a painful total knee replacement. J Bone Joint Surg Br. 2008; 90(3):265–271. PMID: 18310744.
Article13. Bonnin MP, Saffarini M, Shepherd D, Bossard N, Dantony E. Oversizing the tibial component in TKAs: incidence, consequences and risk factors. Knee Surg Sports Traumatol Arthrosc. 2016; 24(8):2532–2540. PMID: 25605560.
Article14. Hartel MJ, Loosli Y, Delfosse D, et al. The influence of tibial morphology on the design of an anatomical tibial baseplate for TKA. Knee. 2014; 21(2):415–419. PMID: 24503228.
Article15. Akagi M, Mori S, Nishimura S, Nishimura A, Asano T, Hamanishi C. Variability of extraarticular tibial rotation references for total knee arthroplasty. Clin Orthop Relat Res. 2005; (436):172–176. PMID: 15995437.
Article16. Berhouet J, Beaufils P, Boisrenoult P, Frasca D, Pujol N. Rotational positioning of the tibial tray in total knee arthroplasty: a CT evaluation. Orthop Traumatol Surg Res. 2011; 97(7):699–704. PMID: 21993150.
Article17. Ikeuchi M, Yamanaka N, Okanoue Y, Ueta E, Tani T. Determining the rotational alignment of the tibial component at total knee replacement: a comparison of two techniques. J Bone Joint Surg Br. 2007; 89(1):45–49. PMID: 17259415.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Fracture of Tibial Base Plate Following Total Knee Arthroplasty: Report of a Case
- Combined Rotational Alignment Change after Total Knee Arthroplasty in Different Tibial Component Designs: Implications for Optimal Tibial Component Rotational Alignment
- Osteotomy of the Tibial Tubercle in difficult Total Knee Arthroplasty
- Analysis of Proximal Tibial Resection Surface Dimention with Korean Total Knee Arthroplasty Specimens
- Breakage of the Implant after Total Knee Replacement: Cases Report