J Korean Orthop Assoc.
2018 Apr;53(2):136-142. 10.4055/jkoa.2018.53.2.136.
The Relationship between Body Mass Index and Diabetic Foot Ulcer, Sensory, Blood Circulation of Foot on Type II Diabetes Mellitus Patients
- Affiliations
-
- 1Department of Orthopaedic Surgery, Chosun University School of Medicine, Gwangju, Korea. leejy88@chosun.ac.kr
- KMID: 2410061
- DOI: http://doi.org/10.4055/jkoa.2018.53.2.136
Abstract
- PURPOSE
Excessive weight bearing from obesity may induce pains in the lower extremity and resulting functional abnormality. Here we aimed to identify the relationship, it is intended to identity relationship obesity has with diabetic foot ulcer, sensory function, and blood circulation in diabetic patients.
MATERIALS AND METHODS
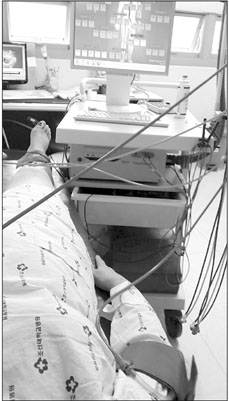
We included patients who hospitalized or visited the department of orthopedic surgery for the treatment of diabetic foot ulcer, between January 2010 and December 2015. Among them, those aged over 30 years, diagnosed with diabetes with a progression of more than one year, and an HbA1c level of less than 7.5% were included for final analysis. For obesity, body mass index (BMI) was used, those with a BMI of over 18.5 kg/m2 were included. Using the Asian cut point of World Health Organization, patients were classified into normal, overweight, or obese. For foot ulcers, patients were classified using the Wagner ulcer classification. For sensory function, it was measured by scoring it with Semmes-Weinstein monofilament of International Working Group on the Diabetic Foot (IWGDF). Moreover for blood circulation, ankle-brachial index (ABI) was measured.
RESULTS
For the sensory function, it was found that the overweight group obtained the highest score and the obesity group obtained the lowest score. For ABI, the overweight group scored the highest and the normal group scored the lowest. Moreover diabetic foot ulcer was the highest in the obesity group and the lowest in the normal group. From these results, it was considered that BMI had no relationship with sensory or blood circulation of the feet. However, the relationship between the diabetic foot ulcer and BMI showed statistical significance; according to the result of regression analysis, BMI of diabetic patients had a positive correlation with diabetic foot ulcer.
CONCLUSION
This study showed that the sensory function and blood circulation of the feet had no relationship with diabetic foot ulcer; however, BMI appears to have a positive correlation with diabetic foot ulcer. Moreover, it seems to be a good index for determining the risk of diabetic foot ulcer.
Keyword
MeSH Terms
Figure
Reference
-
1. Statiscics Korea [Internet]. Deajeon: Statistics Korea;2014. Available from: kostat.go.kr/portal/eng/pressReleases/11/4/index.board.2. Brown WV, Fujioka K, Wilson PW, Woodworth KA. Obesity: why be concerned? Am J Med. 2009; 122:S4–S11.
Article3. Gray N, Picone G, Sloan F, Yashkin A. Relation between BMI and diabetes mellitus and its complications among US older adults. South Med J. 2015; 108:29–36.
Article4. Boyko EJ, Ahroni JH, Stensel V, Forsberg RC, Davignon DR, Smith DG. A prospective study of risk factors for diabetic foot ulcer. The Seattle Diabetic Foot Study. Diabetes Care. 1999; 22:1036–1042.
Article5. Park SA, Ko SH, Lee SH, et al. Incidence of diabetic foot and associated risk factors in type 2 diabetic patients: a five-year observational study. Korean Diabetes J. 2009; 33:315–323.
Article6. Tsuritani I, Honda R, Noborisaka Y, Ishida M, Ishizaki M, Yamada Y. Impact of obesity on musculoskeletal pain and difficulty of daily movements in Japanese middle-aged women. Maturitas. 2002; 42:23–30.
Article7. Moulik PK, Mtonga R, Gill GV. Amputation and mortality in new-onset diabetic foot ulcers stratified by etiology. Diabetes Care. 2003; 26:491–494.
Article8. Sohn MW, Budiman-Mak E, Lee TA, Oh E, Stuck RM. Significant J-shaped association between body mass index (BMI) and diabetic foot ulcers. Diabetes Metab Res Rev. 2011; 27:402–409.
Article9. Nosadini R, Tonolo G. Relationship between blood glucose control, pathogenesis and progression of diabetic nephropathy. J Am Soc Nephrol. 2004; 15:Suppl 1. S1–S5.
Article10. Lee JM. Antihyperglycemic agent combination therapy for patients with type 2 diabetes mellitus. J Korean Med Assoc. 2014; 57:435–443.
Article11. American Diabetes Association. Diabetes Care. 2010; 33:Suppl 1. S62–S69.12. Seo DK, Lee HS. Management of diabetic foot ulcer. J Korean Foot Ankle Soc. 2014; 18:1–7.
Article13. Hills AP, Hennig EM, Byrne NM, Steele JR. The biomechanics of adiposity: structural and functional limitations of obesity and implications for movement. Obes Rev. 2002; 3:35–43.14. Singh N, Armstrong DG, Lipsky BA. Preventing foot ulcers in patients with diabetes. JAMA. 2005; 293:217–228.
Article15. Hooi JD, Stoffers HE, Kester AD, van RJ, Knottnerus JA. Peripheral arterial occlusive disease: prognostic value of signs, symptoms, and the ankle-brachial pressure index. Med Decis Making. 2002; 22:99–107.
Article16. Lavery LA, Peters EJ, Armstrong DG. What are the most effective interventions in preventing diabetic foot ulcers? Int Wound J. 2008; 5:425–433.
Article17. Bays RA, Healy DA, Atnip RG, Neumyer M, Thiele BL. Validation of air plethysmography, photoplethysmography, and duplex ultrasonography in the evaluation of severe venous stasis. J Vasc Surg. 1994; 20:721–727.
Article18. Watanabe Y, Masaki H, Yunoki Y, et al. Ankle-brachial index, toe-brachial index, and pulse volume recording in healthy young adults. Ann Vasc Dis. 2015; 8:227–235.
Article19. Koh BR, Kim YK, Ahn SM, et al. Relationship between diabetic peripheral vascular disease and ankle-brachial index. J Korean Endocr Soc. 2006; 21:382–388.
Article20. Lee HS. Prevention and management of the diabetic foot. J Korean Med Assoc. 2013; 56:220–228.
Article21. Huang ES, Laiteerapong N, Liu JY, John PM, Moffet HH, Karter AJ. Rates of complications and mortality in older patients with diabetes mellitus: the diabetes and aging study. JAMA Intern Med. 2014; 174:251–258.22. Karki DB, Yadava SK, Pant S, Thusa N, Dangol E, Ghimire S. Prevalence of sensory neuropathy in type 2 diabetes mellitus and its correlation with duration of disease. Kathmandu Univ Med J (KUMJ). 2016; 14:120–124.