Yonsei Med J.
2018 May;59(3):438-444. 10.3349/ymj.2018.59.3.438.
Radiographic and Clinical Outcomes of Robot-Assisted Posterior Pedicle Screw Fixation: Two-Year Results from a Randomized Controlled Trial
- Affiliations
-
- 1Spine Center and Department of Orthopaedic Surgery, Seoul National University College of Medicine, Seoul National University Bundang Hospital, Seongnam, Korea. highcervical@gmail.com
- 2Department of Orthopaedic Surgery, Seoul National University College of Medicine, Seoul National University Hospital, Seoul, Korea.
- KMID: 2407868
- DOI: http://doi.org/10.3349/ymj.2018.59.3.438
Abstract
- PURPOSE
We prospectively assessed the early radiographic and clinical outcomes (minimum follow-up of 2 years) of robot-assisted pedicle screw fixation (Robot-PSF) and conventional freehand pedicle screw fixation (Conv-PSF).
MATERIALS AND METHODS
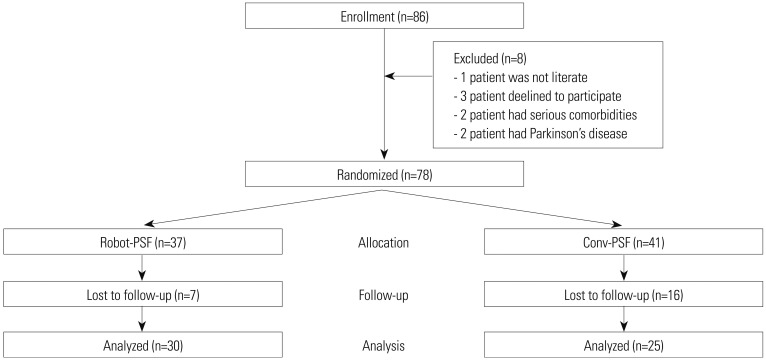
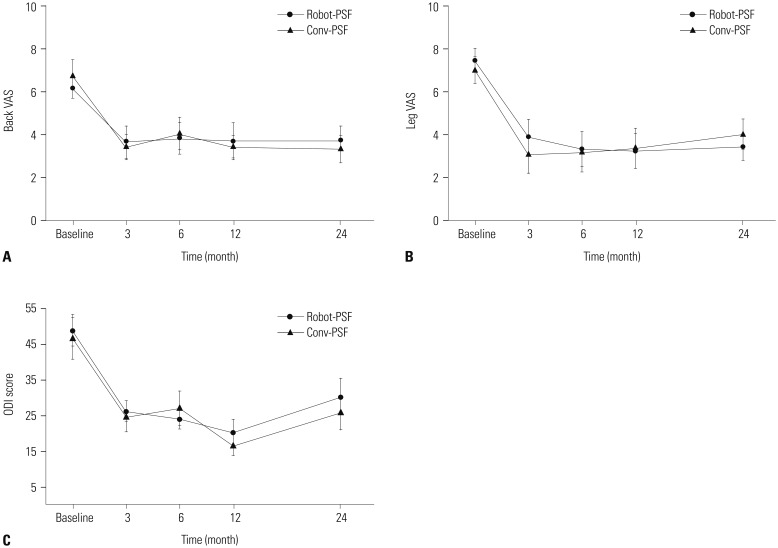
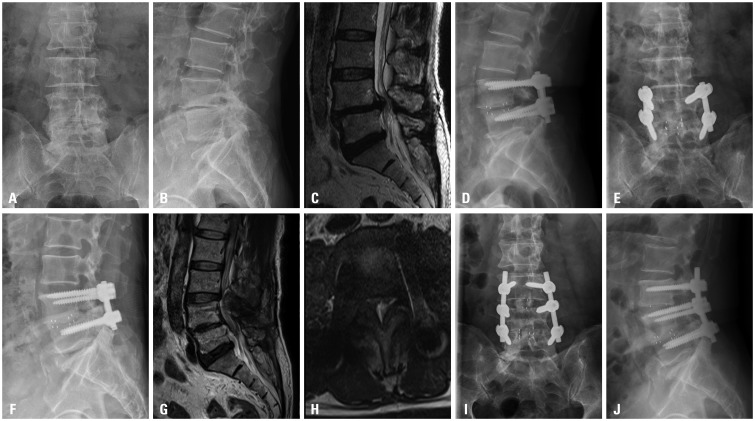
Patients were randomly assigned to Robot-PSF (37 patients) or Conv-PSF (41 patients) for posterior interbody fusion surgery. The Robot-PSF group underwent minimally invasive pedicle screw fixation using a pre-planned robot-guided screw trajectory. The Conv-PSF underwent screw fixation using the freehand technique. Radiographic adjacent segment degeneration (ASD) was measured on plain radiographs, and clinical outcomes were measured using visual analogue scale (VAS) and Oswestry disability index (ODI) scores regularly after surgery.
RESULTS
The two groups had similar values for radiographic ASD, including University California at Los Angeles grade, vertebral translation, angular motion, and loss of disc height (p=0.320). At final follow-up, both groups had experienced significant improvements in back VAS, leg VAS, and ODI scores after surgery (p < 0.001), although inter-group differences were not significant for back VAS (p=0.876), leg VAS (p=0.429), and ODI scores (p=0.952). In the Conv-PSF group, revision surgery was required for two of the 25 patients (8%), compared to no patients in the Robot-PSF group.
CONCLUSION
There were no significant differences in radiographic ASD and clinical outcomes between Robot-PSF and Conv-PSF. Thus, the advantages of robot-assisted surgery (accurate pedicle screw insertion and minimal facet joint violation) do not appear to be clinically significant.
Keyword
MeSH Terms
Figure
Reference
-
1. Molliqaj G, Schatlo B, Alaid A, Solomiichuk V, Rohde V, Schaller K, et al. Accuracy of robot-guided versus freehand fluoroscopy-assisted pedicle screw insertion in thoracolumbar spinal surgery. Neurosurg Focus. 2017; 42:E14.
Article2. Lonjon N, Chan-Seng E, Costalat V, Bonnafoux B, Vassal M, Boetto J. Robot-assisted spine surgery: feasibility study through a prospective case-matched analysis. Eur Spine J. 2016; 25:947–955. PMID: 25575857.
Article3. Kuo KL, Su YF, Wu CH, Tsai CY, Chang CH, Lin CL, et al. Assessing the intraoperative accuracy of pedicle screw placement by using a bone-mounted miniature robot system through secondary registration. PLoS One. 2016; 11:e0153235. PMID: 27054360.
Article4. Schatlo B, Molliqaj G, Cuvinciuc V, Kotowski M, Schaller K, Tessitore E. Safety and accuracy of robot-assisted versus fluoroscopy-guided pedicle screw insertion for degenerative diseases of the lumbar spine: a matched cohort comparison. J Neurosurg Spine. 2014; 20:636–643. PMID: 24725180.
Article5. Hu X, Ohnmeiss DD, Lieberman IH. Robotic-assisted pedicle screw placement: lessons learned from the first 102 patients. Eur Spine J. 2013; 22:661–666. PMID: 22975723.
Article6. Devito DP, Kaplan L, Dietl R, Pfeiffer M, Horne D, Silberstein B, et al. Clinical acceptance and accuracy assessment of spinal implants guided with SpineAssist surgical robot: retrospective study. Spine (Phila Pa 1976). 2010; 35:2109–2115. PMID: 21079498.7. Ringel F, Stüer C, Reinke A, Preuss A, Behr M, Auer F, et al. Accuracy of robot-assisted placement of lumbar and sacral pedicle screws: a prospective randomized comparison to conventional freehand screw implantation. Spine (Phila Pa 1976. 2012; 37:E496–E501. PMID: 22310097.8. Liu H, Chen W, Wang Z, Lin J, Meng B, Yang H. Comparison of the accuracy between robot-assisted and conventional freehand pedicle screw placement: a systematic review and meta-analysis. Int J Comput Assist Radiol Surg. 2016; 11:2273–2281. PMID: 27334134.
Article9. Kim HJ, Jung WI, Chang BS, Lee CK, Kang KT, Yeom JS. A prospective, randomized, controlled trial of robot-assisted vs freehand pedicle screw fixation in spine surgery. Int J Med Robot. 2017; 13:e1779.
Article10. Kim HJ, Kang KT, Park SC, Kwon OH, Son J, Chang BS, et al. Biomechanical advantages of robot-assisted pedicle screw fixation in posterior lumbar interbody fusion compared with freehand technique in a prospective randomized controlled trial-perspective for patient-specific finite element analysis. Spine J. 2017; 17:671–680. PMID: 27867080.
Article11. Holly LT, Schwender JD, Rouben DP, Foley KT. Minimally invasive transforaminal lumbar interbody fusion: indications, technique, and complications. Neurosurg Focus. 2006; 20:E6.
Article12. Kim HJ, Lee SH, Chang BS, Lee CK, Lim TO, Hoo LP, et al. Monitoring the quality of robot-assisted pedicle screw fixation in the lumbar spine by using a cumulative summation test. Spine (Phila Pa 1976). 2015; 40:87–94. PMID: 25575085.
Article13. Weinstein JN, Rydevik BL, Rauschning W. Anatomic and technical considerations of pedicle screw fixation. Clin Orthop Relat Res. 1992; (284):34–46.
Article14. Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976). 2001; 26:1873–1878. PMID: 11568697.
Article15. Ghiselli G, Wang JC, Bhatia NN, Hsu WK, Dawson EG. Adjacent segment degeneration in the lumbar spine. J Bone Joint Surg Am. 2004; 86-A:1497–1503. PMID: 15252099.
Article16. Ghiselli G, Wang JC, Hsu WK, Dawson EG. L5-S1 segment survivorship and clinical outcome analysis after L4-L5 isolated fusion. Spine (Phila Pa 1976). 2003; 28:1275–1280. PMID: 12811271.
Article17. Miyakoshi N, Abe E, Shimada Y, Hongo M, Chiba M, Sato K. Anterior decompression with single segmental spinal interbody fusion for lumbar burst fracture. Spine (Phila Pa 1976). 1999; 24:67–73. PMID: 9921594.
Article18. Lee DY, Jung TG, Lee SH. Single-level instrumented mini-open transforaminal lumbar interbody fusion in elderly patients. J Neurosurg Spine. 2008; 9:137–144. PMID: 18764745.
Article19. Cheh G, Bridwell KH, Lenke LG, Buchowski JM, Daubs MD, Kim Y, et al. Adjacent segment disease following lumbar/thoracolumbar fusion with pedicle screw instrumentation: a minimum 5-year follow-up. Spine (Phila Pa 1976). 2007; 32:2253–2257. PMID: 17873819.20. Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine (Phila Pa 1976). 2000; 25:2940–2952. PMID: 11074683.
Article21. Babu R, Park JG, Mehta AI, Shan T, Grossi PM, Brown CR, et al. Comparison of superior-level facet joint violations during open and percutaneous pedicle screw placement. Neurosurgery. 2012; 71:962–970. PMID: 22843132.
Article22. Park Y, Ha JW, Lee YT, Sung NY. Cranial facet joint violations by percutaneously placed pedicle screws adjacent to a minimally invasive lumbar spinal fusion. Spine J. 2011; 11:295–302. PMID: 21474080.
Article23. Radcliff KE, Kepler CK, Maaieh M, Anderson DG, Rihn J, Albert T, et al. What is the rate of lumbar adjacent segment disease after percutaneous versus open fusion? Orthop Surg. 2014; 6:118–120. PMID: 24890293.
Article24. Kanamori M, Yasuda T, Hori T, Suzuki K, Kawaguchi Y. Minimum 10-year follow-up study of anterior lumbar interbody fusion for degenerative spondylolisthesis: progressive pattern of the adjacent disc degeneration. Asian Spine J. 2012; 6:105–114. PMID: 22708014.
Article25. Soh J, Lee JC, Shin BJ. Analysis of risk factors for adjacent segment degeneration occurring more than 5 years after fusion with pedicle screw fixation for degenerative lumbar spine. Asian Spine J. 2013; 7:273–281. PMID: 24353843.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Risk Factors of Unsatisfactory Robot-Assisted Pedicle Screw Placement: A Case-Control Study
- Short Segment versus Long Segment Pedicle Screws Fixation in Management of Thoracolumbar Burst Fractures: Meta-Analysis
- Commentary on “A Propensity Score-Matched Cohort Study Comparing 3 Different Spine Pedicle Screw Fixation Methods: Freehand, Fluoroscopy-Guided, and Robot-Assisted Techniques”
- Cotrel - Dubousset Pedicle Screw Fixation After Posterior Decompression of Lumbar Spinal Stenosis
- Change of Kyphotic Angle in Posterior Pedicle Screw Fixation for Thoracic and Lumbar Burst Fractures: Comparison Study by the Screw Fixation Level