Clin Exp Otorhinolaryngol.
2018 Mar;11(1):40-45. 10.21053/ceo.2017.00332.
Bacterial Ball as an Unusual Finding in Patients With Chronic Rhinosinusitis
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Chuncheon Sacred Heart Hospital and Nano-Bio Regenerative Medical Institute, Hallym University College of Medicine, Chuncheon, Korea.
- 2Department of Pathology, Hanyang University College of Medicine, Seoul, Korea.
- 3Department of Otorhinolaryngology-Head and Neck Surgery, Hanyang University College of Medicine, Seoul, Korea. shcho@hanyang.ac.kr
- KMID: 2407791
- DOI: http://doi.org/10.21053/ceo.2017.00332
Abstract
OBJECTIVES
Pathophysiology of chronic rhinosinusitis (CRS) is very complex and has not yet been clearly understood. To date, various factors have been researched to have relations with the pathogenesis of CRS, such as superantigens and biofilms. Recently, we found an unusual pathological finding in patients with CRS, and we called this new entity as bacteria ball (or bioball). In this study, we analyze the clinical characteristics of bacteria ball occurred in CRS.
METHODS
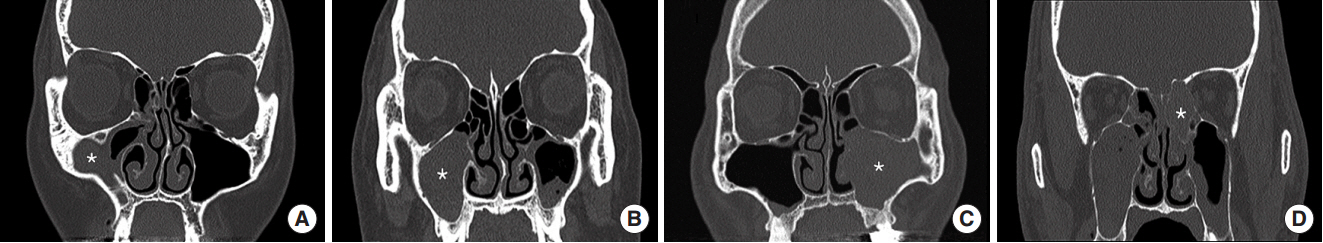
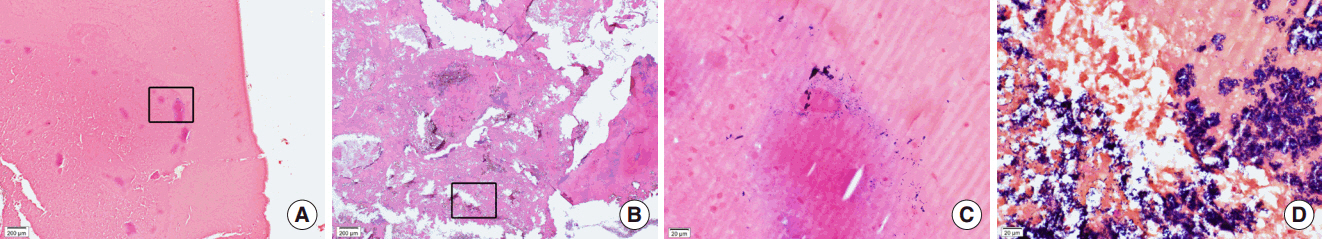
This study enrolled consecutive 247 patients with CRS who underwent functional endoscopic sinus surgery from January 2015 to August 2016. The diagnosis of bacterial ball was made when negative in Gomori-methenamine-silver stain and positive in Gram stain. Histologically, bacterial ball was defined as acellular mucous materials with bacterial colonies and inflammatory cell infiltrates. We compared clinical data and computed tomography (CT) findings between fungal and bacterial balls.
RESULTS
Six cases (2.4%) of CRS were confirmed histologically as bacterial ball. Most of them were found in the maxillary sinus of CRS without nasal polyposis (66.7%). Bacterial ball was green or brown colored materials similar to fungal ball which was harder and tightly adherent to the antral mucosa. Compared to fungal ball, patients with bacterial ball showed significantly less peripheral eosinophils (P=0.011) and calcification in CT scans (P=0.003).
CONCLUSION
Bacterial ball is unusual findings occurred in patient with CRS which is different from fungal ball and biofilm. For diagnosis of bacterial ball, Gram stain is essentially required to identify bacterial colonies. Bacterial ball might appear to be evidence of a new strategy for living in the paranasal sinuses.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Unveiling the Diverse Spectrum of Fungal Rhinosinusitis
Seok Hyun Cho
Clin Exp Otorhinolaryngol. 2020;13(2):89-90. doi: 10.21053/ceo.2019.02026.Bacterial Ball in Concha Bullosa: Report of a Case With Unusual Location
Su-Jong Kim, Jee Won Moon, Yongmin Cho, Heung-Man Lee
Korean J Otorhinolaryngol-Head Neck Surg. 2023;66(5):335-339. doi: 10.3342/kjorl-hns.2021.01067.
Reference
-
1. Fokkens WJ, Lund VJ, Mullol J, Bachert C, Alobid I, Baroody F, et al. EPOS 2012: European position paper on rhinosinusitis and nasal polyps 2012: a summary for otorhinolaryngologists. Rhinology. 2012; Mar. 50(1):1–12.
Article2. Adams PF, Lucas JW, Barnes PM. Summary health statistics for the U.S. population: National Health Interview Survey, 2006. Vital Health Stat 10. 2008; Jan. (236):1–104.3. Jarvis D, Newson R, Lotvall J, Hastan D, Tomassen P, Keil T, et al. Asthma in adults and its association with chronic rhinosinusitis: the GA2LEN survey in Europe. Allergy. 2012; Jan. 67(1):91–8.
Article4. Kim DH, Han K, Kim SW. Effect of chronic rhinosinusitis with or without nasal polyp on quality of life in South Korea: 5th Korea National Health and Nutrition Examination Survey Korean. Clin Exp Otorhinolaryngol. 2016; Jun. 9(2):150–6.
Article5. Brandsted R, Sindwani R. Impact of depression on disease-specific symptoms and quality of life in patients with chronic rhinosinusitis. Am J Rhinol. 2007; Jan-Feb. 21(1):50–4.
Article6. Stevens WW, Lee RJ, Schleimer RP, Cohen NA. Chronic rhinosinusitis pathogenesis. J Allergy Clin Immunol. 2015; Dec. 136(6):1442–53.
Article7. Hulse KE, Stevens WW, Tan BK, Schleimer RP. Pathogenesis of nasal polyposis. Clin Exp Allergy. 2015; Feb. 45(2):328–46.
Article8. Kennedy JL, Borish L. Chronic rhinosinusitis and antibiotics: the good, the bad, and the ugly. Am J Rhinol Allergy. 2013; Nov-Dec. 27(6):467–72.
Article9. Bachert C, Hamilos DL. Are antibiotics useful for chronic rhinosinusitis? J Allergy Clin Immunol Pract. 2016; Jul-Aug. 4(4):629–38.
Article10. Head K, Chong LY, Piromchai P, Hopkins C, Philpott C, Schilder AG, et al. Systemic and topical antibiotics for chronic rhinosinusitis. Cochrane Database Syst Rev. 2016; Apr. 4:CD011994.
Article11. Kim HD, Lee DW, Pyo JY, Oh YH, Cho SH. Bioballs causing asymptomatic or recurrent acute rhinosinusitis: two cases. J Rhinol. 2016; May. 23(1):55–9.
Article12. Van Crombruggen K, Zhang N, Gevaert P, Tomassen P, Bachert C. Pathogenesis of chronic rhinosinusitis: inflammation. J Allergy Clin Immunol. 2011; Oct. 128(4):728–32.
Article13. Kilty SJ, Desrosiers MY. The role of bacterial biofilms and the pathophysiology of chronic rhinosinusitis. Curr Allergy Asthma Rep. 2008; May. 8(3):227–33.
Article14. Bernstein JM, Ballow M, Schlievert PM, Rich G, Allen C, Dryja D. A superantigen hypothesis for the pathogenesis of chronic hyperplastic sinusitis with massive nasal polyposis. Am J Rhinol. 2003; Nov-Dec. 17(6):321–6.
Article15. Schubert MS. A superantigen hypothesis for the pathogenesis of chronic hypertrophic rhinosinusitis, allergic fungal sinusitis, and related disorders. Ann Allergy Asthma Immunol. 2001; Sep. 87(3):181–8.16. Choi EB, Hong SW, Kim DK, Jeon SG, Kim KR, Cho SH, et al. Decreased diversity of nasal microbiota and their secreted extracellular vesicles in patients with chronic rhinosinusitis based on a metagenomic analysis. Allergy. 2014; Apr. 69(4):517–26.
Article17. Al-Mutairi D, Kilty SJ. Bacterial biofilms and the pathophysiology of chronic rhinosinusitis. Curr Opin Allergy Clin Immunol. 2011; Feb. 11(1):18–23.
Article18. Perloff JR, Palmer JN. Evidence of bacterial biofilms on frontal recess stents in patients with chronic rhinosinusitis. Am J Rhinol. 2004; Nov-Dec. 18(6):377–80.
Article19. Prince AA, Steiger JD, Khalid AN, Dogrhamji L, Reger C, Eau Claire S, et al. Prevalence of biofilm-forming bacteria in chronic rhinosinusitis. Am J Rhinol. 2008; May-Jun. 22(3):239–45.
Article20. Foreman A, Jervis-Bardy J, Wormald PJ. Do biofilms contribute to the initiation and recalcitrance of chronic rhinosinusitis? Laryngoscope. 2011; May. 121(5):1085–91.
Article21. Hekiert AM, Kofonow JM, Doghramji L, Kennedy DW, Chiu AG, Palmer JN, et al. Biofilms correlate with TH1 inflammation in the sinonasal tissue of patients with chronic rhinosinusitis. Otolaryngol Head Neck Surg. 2009; Oct. 141(4):448–53.22. Sanclement JA, Webster P, Thomas J, Ramadan HH. Bacterial biofilms in surgical specimens of patients with chronic rhinosinusitis. Laryngoscope. 2005; Apr. 115(4):578–82.
Article23. Foreman A, Singhal D, Psaltis AJ, Wormald PJ. Targeted imaging modality selection for bacterial biofilms in chronic rhinosinusitis. Laryngoscope. 2010; Feb. 120(2):427–31.
Article