Infect Chemother.
2010 Apr;42(2):82-86.
Laboratory Confirmatory Rate of Pandemic Influenza (H1N1 2009) Virus in Korean Households with Index Case
- Affiliations
-
- 1Armed Forces Seoul Hospital, Seoul, Korea.
- 2Department of Infectious Diseases, Chonnam National University Medical School, Gwangju, Korea. medkid@dreamwiz.com
Abstract
- BACKGROUND
Influenza transmission in households a subject of renewed interest especially in pandemic situation. We performed this study to investigate the laboratory-confirmatory rate in household contacts with index cases of pandemic influenza (H1N1 2009).
MATERIALS AND METHODS
For three months from 1 September and 29 November 2009, people who had a history of close contact with confirmed cases of pandemic influenza (index case) were recruited. The information on the study participants was collected using a standardized questionnaire. Presence of the pandemic influenza (H1N1 2009) infection was confirmed by real-time reverse-transcription polymerase chain reaction (RT-PCR).
RESULTS
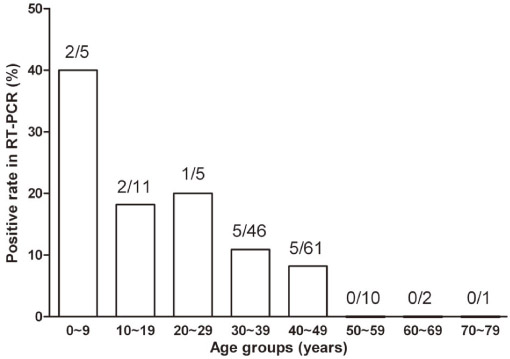
A total of 113 index cases and 141 household contacts were investigated. One hundred and four index cases (92.0%) were younger than 20 years. The median age of household contacts was 40 years. Twenty eight household contacts (19.8%) had acute respiratory illness (ARI). Overall, 10.6% of enrolled household contacts were positive in RT-PCR for pandemic influenza (H1N1 2009). The positive rate of household contacts with ARI was 25.0% and it was 7.1% in household contacts without ARI. The positive rate was significantly higher in children and young adults under 30 years (28.3%) compared with that in household contacts older than 30 years (8.3%).
CONCLUSIONS
This results showed a significant role of mild symptomatic or asymptomatic pandemic influenza (H1N1 2009) patients as a virus carriers in households.
Keyword
MeSH Terms
Figure
Reference
-
1. Santibañez S, Fiore AE, Merlin TL, Redd S. A primer on strategies for prevention and control of seasonal and pandemic influenza. Am J Public Health. 2009. 99:Suppl 2. S216–S224.
Article2. Longini IM Jr, Koopman JS, Monto AS, Fox JP. Estimating household and community transmission parameters for influenza. Am J Epidemiol. 1982. 115:736–751.
Article3. Health Protection Agency. Health Protection Scotland. National Public Health Service for Wales. HPA Northern Ireland Swine influenza investigation teams. Epidemiology of new influenza A (H1N1) virus infection, United Kingdom, April-June 2009. Euro Surveill. 2009. 14:pii: 19232.4. Cauchemez S, Donnelly CA, Reed C, Ghani AC, Fraser C, Kent CK, Finelli L, Ferguson NM. Household transmission of 2009 pandemic influenza A (H1N1) virus in the United States. N Engl J Med. 2009. 361:2619–2627.
Article5. Yang Y, Sugimoto JD, Halloran ME, Basta NE, Chao DL, Matrajt L, Potter G, Kenah E, Longini IM Jr. The transmissibility and control of pandemic influenza A (H1N1) virus. Science. 2009. 326:729–733.
Article6. Odaira F, Takahashi H, Toyokawa T, Tsuchihashi Y, Kodama T, Yahata Y, Sunagawa T, Taniguchi K, Okabe N. Assessment of secondary attack rate and effectiveness of antiviral prophylaxis among household contacts in an influenza A(H1N1) outbreak in Kobe, Japan, May-June 2009. Euro Surveill. 2009. 14:pii: 19320.7. Kelly H, Carville K, Grant K, Jacoby P, Tran T, Barr I. Estimation of influenza vaccine effectiveness from routine surveillance data. PLoS One. 2009. 4:e5079.
Article8. Calatayud L, Kurkela S, Neave PE, Brock A, Perkins S, Zuckerman M, Sudhanva M, Bermingham A, Ellis J, Pebody R, Catchpole M, Heathcock R, Maguire H. Pandemic (H1N1) 2009 virus outbreak in a school in London, April-May 2009: an observational study. Epidemiol Infect. 2010. 138:183–191.
Article9. Foy HM, Cooney MK, Allan ID, Albrecht JK. Influenza B in households: virus shedding without symptoms or antibody response. Am J Epidemiol. 1987. 126:506–515.
Article10. Winther B, Alper CM, Mandel EM, Doyle WJ, Hendley JO. Temporal relationships between colds, upper respiratory viruses detected by polymerase chain reaction, and otitis media in young children followed through a typical cold season. Pediatrics. 2007. 119:1069–1075.
Article11. Winther B, Hayden FG, Hendley JO. Picornavirus infections in children diagnosed by RT-PCR during longitudinal surveillance with weekly sampling: Association with symptomatic illness and effect of season. J Med Virol. 2006. 78:644–650.
Article12. Carrat F, Vergu E, Ferguson NM, Lemaitre M, Cauchemez S, Leach S, Valleron AJ. Time lines of infection and disease in human influenza: a review of volunteer challenge studies. Am J Epidemiol. 2008. 167:775–785.
Article13. Ng S, Cowling BJ, Fang VJ, Chan KH, Ip DK, Cheng CK, Uyeki TM, Houck PM, Malik Peiris JS, Leung GM. Effects of oseltamivir treatment on duration of clinical illness and viral shedding and household transmission of influenza virus. Clin Infect Dis. 2010. 50:707–714.
Article14. Mermel LA. Swine-origin influenza virus in young age groups. Lancet. 2009. 373:2108–2109.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The 2009 H1N1 Pandemic Influenza in Korea
- Influenza Associated Pneumonia
- A Case of Oseltamivir-Resistant Pandemic Influenza (H1N1 2009)
- Three Reinfection Cases of the Pandemic Influenza (H1N1 2009)
- A Case of Pseudomembranous Tracheobronchitis Complicated by Coinfection of 2009 Pandemic Influenza A/H1N1 and Staphylococcus aureus