Infect Chemother.
2011 Oct;43(5):425-428. 10.3947/ic.2011.43.5.425.
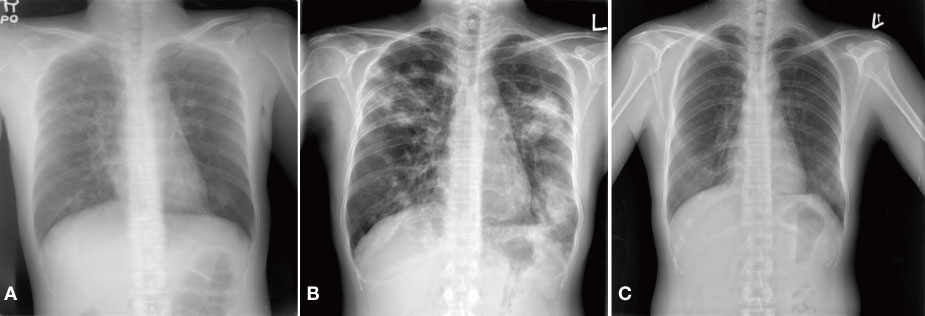
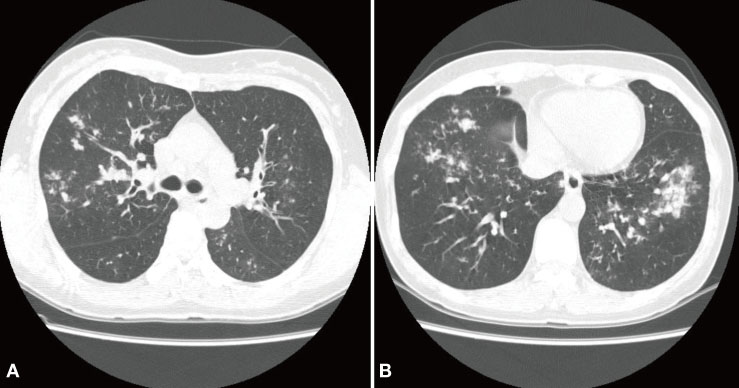
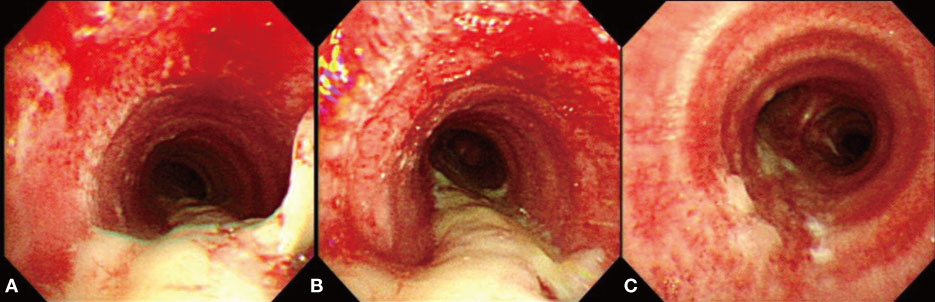
A Case of Pseudomembranous Tracheobronchitis Complicated by Coinfection of 2009 Pandemic Influenza A/H1N1 and Staphylococcus aureus
- Affiliations
-
- 1Department of Internal Medicine, Gangneung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea. jbh@gnah.co.kr
- 2Department of Radiology, Gangneung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea.
- KMID: 2285017
- DOI: http://doi.org/10.3947/ic.2011.43.5.425
Abstract
- An influenza pandemic due to a novel influenza A/H1N1 virus occurred after April 2009. This virus has some characteristics that differentiate it from the seasonal influenza virus. The 2009 pandemic influenza A/H1N1 virus can frequently infect the lower respiratory tract, and it might cause acute tracheobronchitis as well as pneumonia. Viral-bacterial interaction is well known as an important mechanism of the pathogenesis of respiratory complications of influenza. Herein, we report on a case that presented with pseudomembranous tracheobronchitis complicated by coinfection with 2009 pandemic influenza A/H1N1 and Staphylococcus aureus. We also review the relevent literature.
Keyword
MeSH Terms
Figure
Reference
-
1. World Health Organization (WHO). New influenza A (H1N1) virus: global epidemiological situation, June 2009. Weekly Epidl Rec. 2009. 84:249–257.2. Brundage JF. Interactions between influenza and bacterial respiratory pathogens: implications for pandemic preparedness. Lancet Infect Dis. 2006. 6:303–312.
Article3. McCullers JA. Insights into the interaction between influenza virus and pneumococcus. Clin Microbiol Rev. 2006. 19:571–582.
Article4. Smith CB, Kanner RE, Golden CA, Klauber MR, Renzetti AD Jr. Effect of viral infections on pulmonary function in patients with chronic obstructive pulmonary diseases. J Infect Dis. 1980. 141:271–280.
Article5. Boots RJ, Paterson DL, Allworth AM, Faoagali JL. Successful treatment of post-influenza pseudomembranous necrotising bronchial aspergillosis with liposomal amphotericin, inhaled amphotericin B, gamma interferon and GM-CSF. Thorax. 1999. 54:1047–1049.
Article6. Herrmann RE, Ogura GI, Johnson ES, Toll HW Jr, White WC. Respiratory deaths associated with Asian influenza epidemic; report of twenty-three cases. J Am Med Assoc. 1958. 166:467–471.7. Enserink M. Pandemic influenza. Ferrets shed light on new virus's severity and spread. Science. 2009. 325:17.
Article8. Childs RA, Palma AS, Wharton S, Matrosovich T, Liu Y, Chai W, Campanero-Rhodes MA, Zhang Y, Eickmann M, Kiso M, Hay A, Matrosovich M, Feizi T. Receptor-binding specificity of pandemic influenza A(H1N1) 2009 virus determined by carbohydrate microarray. Nat Biotechnol. 2009. 27:797–799.
Article9. Chen J, Lee KH, Steinhauer DA, Stevens DJ, Skehel JJ, Wiley DC. Structure of the hemagglutinin precursor cleavage site, a determinant of influenza pathogenicity and the origin of the labile conformation. Cell. 1998. 95:409–417.
Article10. Tashiro M, Ciborowski P, Klenk HD, Pulverer G, Rott R. Role of Staphylococcus protease in the development of influenza pneumonia. Nature. 1987. 325:536–537.
Article11. Tashiro M, Ciborowski P, Reinacher M, Pulverer G, Klenk HD, Rott R. Synergistic role of staphylococcal proteases in the induction of influenza virus pathogenicity. Virology. 1987. 157:421–430.
Article12. Louria DB, Blumenfeld HL, Ellis JT, Kilbourne ED, Rogers DE. Studies on influenza in the pandemic of 1957-1958. II. Pulmonary complications of influenza. J Clin Invest. 1959. 38:213–265.
Article13. Centers for Disease Control and Prevention (CDC). Intensive-care patients with severe novel influenza A (H1N1) virus infection - Michigan, June 2009. MMWR Morb Mortal Wkly Rep. 2009. 58:749–752.14. Rello J, Rodríguez A, Ibañez P, Socias L, Cebrian J, Marques A, Guerrero J, Ruiz-Santana S, Marquez E, Del Nogal-Saez F, Alvarez-Lerma F, Martínez S, Ferrer M, Avellanas M, Granada R, Maraví-Poma E, Albert P, Sierra R, Vidaur L, Ortiz P, Prieto del Portillo I, Galván B, León-Gil C. H1N1 SEMICYUC Working Group. Intensive care adult patients with severe respiratory failure caused by Influenza A (H1N1) in Spain. Crit Care. 2009. 13:R148.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Severe Pseudomembranous Tracheobronchitis Complicated by Co-infection of Influenza A (H1N1) and Staphylococcus aureus in an Immunocompetent Patient
- A Case of Coinfection with Pandemic (H1N1) 2009 Influenza and Scrub Typhus with Abnormal Liver Function Test
- Pandemic Influenza (H1N1) and Mycobacterium tuberculosis Co-infection
- The 2009 H1N1 Pandemic Influenza in Korea
- Epidemiology, clinical manifestations, and management of pandemic novel Influenza A (H1N1)