Ann Surg Treat Res.
2018 Jan;94(1):36-43. 10.4174/astr.2018.94.1.36.
Anatomical distribution and detection rate of colorectal neoplasms according to age in the colonoscopic screening of a Korean population
- Affiliations
-
- 1Divisions of Oncology/Hematology, Department of Internal Medicine, Korea University College of Medicine, Seoul, Korea.
- 2Korea Medical Institute, Seoul, Korea.
- 3Department of Surgery, Korea University College of Medicine, Seoul, Korea. silee@korea.ac.kr
- KMID: 2405337
- DOI: http://doi.org/10.4174/astr.2018.94.1.36
Abstract
- PURPOSE
Because data as a basis for the determination of proper age and modality for screening of colorectal neoplasms is lacking, we evaluated detection rates and anatomical distribution of colorectal neoplasms according to age in healthy individuals who underwent total colonoscopy for health checkup.
METHODS
A total of 16,100 cases that had received the colonoscopic examination from January to December in 2014 were analyzed. The total number of individuals who received total colonoscopy were divided by the number of individuals harboring colorectal adenoma to calculate the detection rate of colorectal adenoma. Individuals ≤50 years old were classified as young-age group and aged >50 were old-age group. Differences in anatomical locations of colorectal neoplasms were analyzed in the 2 age groups by chi-square test. Risk factors for colorectal adenoma in each age group were analyzed using univariate and multivariate logistic regression analyses.
RESULTS
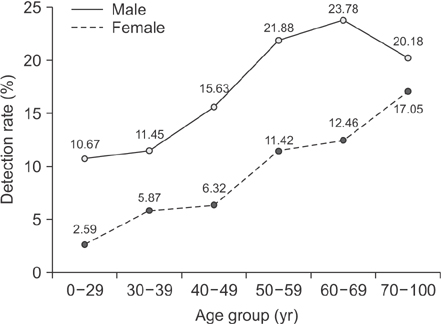
Detection rates of colorectal adenoma were 13.7% in all cases and 12.8% for those in their 40"²s. The main anatomical location of colorectal adenoma was proximal colon in both age groups (P < 0.001). Hyperplastic polyp was mainly distributed to the distal colon in both age groups (P < 0.001). Distal colon was the major site for colorectal cancer in the old-age group (P = 0.001). Proximal location of neoplasms was a risk factor for colorectal adenoma in both age groups with multivariate analysis.
CONCLUSION
These data could be the bases for earlier initiation of screening for colorectal neoplasms with total colonoscopy to detect clinically significant colorectal polyps.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Prevalence and risk factors of colorectal cancer in Asia
Martin CS Wong, Hanyue Ding, Jingxuan Wang, Paul SF Chan, Junjie Huang
Intest Res. 2019;17(3):317-329. doi: 10.5217/ir.2019.00021.
Reference
-
1. Oh CM, Won YJ, Jung KW, Kong HJ, Cho H, Lee JK, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2013. Cancer Res Treat. 2016; 48:436–450.
Article2. Nishihara R, Wu K, Lochhead P, Morikawa T, Liao X, Qian ZR, et al. Long-term colorectal-cancer incidence and mortality after lower endoscopy. N Engl J Med. 2013; 369:1095–1105.
Article3. U.S. Preventive Services Task Force. Screening for colorectal cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2008; 149:627–637.4. Levin B, Lieberman DA, McFarland B, Smith RA, Brooks D, Andrews KS, et al. Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. CA Cancer J Clin. 2008; 58:130–160.
Article5. International Agency for Research on Cancer. Lansdorp-Vogelaar I, von Karsa L. European guidelines for quality assurance in colorectal cancer screening and diagnosis. First Edition--Introduction. Endoscopy. 2012; 44:Suppl 3. SE15–SE30.6. Lee BI, Hong SP, Kim SE, Kim SH, Kim HS, Hong SN, et al. Korean guidelines for colorectal cancer screening and polyp detection. Clin Endosc. 2012; 45:25–43.
Article7. Inra JA, Syngal S. Colorectal cancer in young adults. Dig Dis Sci. 2015; 60:722–733.
Article8. Centers for Disease Control and Prevention (CDC). Vital signs: colorectal cancer screening, incidence, and mortality: United States, 2002-2010. MMWR Morb Mortal Wkly Rep. 2011; 60:884–889.9. Bailey CE, Hu CY, You YN, Bednarski BK, Rodriguez-Bigas MA, Skibber JM, et al. Increasing disparities in the age-related incidences of colon and rectal cancers in the United States, 1975-2010. JAMA Surg. 2015; 150:17–22.
Article10. Siegel RL, Miller KD, Fedewa SA, Ahnen DJ, Meester RGS, Barzi A, et al. Colorectal cancer statistics, 2017. CA Cancer J Clin. 2017; 67:177–193.
Article11. Siegel RL, Fedewa SA, Anderson WF, Miller KD, Ma J, Rosenberg PS, et al. Colorectal cancer incidence patterns in the United States, 1974-2013. J Natl Cancer Inst. 2017; 109:DOI: 10.1093/jnci/djw322.
Article12. Chung SJ, Kim YS, Yang SY, Song JH, Park MJ, Kim JS, et al. Prevalence and risk of colorectal adenoma in asymptomatic Koreans aged 40-49 years undergoing screening colonoscopy. J Gastroenterol Hepatol. 2010; 25:519–525.13. Bae T, Ha Y, Kim C, Lee J, Ha K, Shin S, et al. Distribution of the colonoscopic adenoma detection rate according to age: is recommending colonoscopy screening for koreans over the age of 50 safe? Ann Coloproctol. 2015; 31:46–51.
Article14. Kwak JY, Kim KM, Yang HJ, Yu KJ, Lee JG, Jeong YO, et al. Prevalence of colorectal adenomas in asymptomatic young adults: a window to early intervention? Scand J Gastroenterol. 2016; 51:731–738.
Article15. Lee SE, Jo HB, Kwack WG, Jeong YJ, Yoon YJ, Kang HW. Characteristics of and risk factors for colorectal neoplasms in young adults in a screening population. World J Gastroenterol. 2016; 22:2981–2992.
Article16. Loberg M, Kalager M, Holme O, Hoff G, Adami HO, Bretthauer M. Long-term colorectal-cancer mortality after adenoma removal. N Engl J Med. 2014; 371:799–807.
Article17. Risio M. The natural history of adenomas. Best Pract Res Clin Gastroenterol. 2010; 24:271–280.
Article18. Kim JY, Jung YS, Park JH, Kim HJ, Cho YK, Sohn CI, et al. Different risk factors for advanced colorectal neoplasm in young adults. World J Gastroenterol. 2016; 22:3611–3620.
Article19. Atkin WS, Edwards R, Kralj-Hans I, Wooldrage K, Hart AR, Northover JM, et al. Once-only flexible sigmoidoscopy screening in prevention of colorectal cancer: a multicentre randomised controlled trial. Lancet. 2010; 375:1624–1633.
Article20. Segnan N, Armaroli P, Bonelli L, Risio M, Sciallero S, Zappa M, et al. Once-only sigmoidoscopy in colorectal cancer screening: follow-up findings of the Italian Randomized Controlled Trial--SCORE. J Natl Cancer Inst. 2011; 103:1310–1322.
Article21. Holme O, Loberg M, Kalager M, Bretthauer M, Hernan MA, Aas E, et al. Effect of flexible sigmoidoscopy screening on colorectal cancer incidence and mortality: a randomized clinical trial. JAMA. 2014; 312:606–615.22. Brenner H, Stock C, Hoffmeister M. Effect of screening sigmoidoscopy and screening colonoscopy on colorectal cancer incidence and mortality: systematic review and meta-analysis of randomised controlled trials and observational studies. BMJ. 2014; 348:g2467.
Article23. Schoen RE, Pinsky PF, Weissfeld JL, Yokochi LA, Church T, Laiyemo AO, et al. Colorectal-cancer incidence and mortality with screening flexible sigmoidoscopy. N Engl J Med. 2012; 366:2345–2357.24. Wang YR, Cangemi JR, Loftus EV Jr, Picco MF. Risk of colorectal cancer after colonoscopy compared with flexible sigmoidoscopy or no lower endoscopy among older patients in the United States, 1998-2005. Mayo Clin Proc. 2013; 88:464–470.
Article25. Painter J, Saunders DB, Bell GD, Williams CB, Pitt R, Bladen J. Depth of insertion at flexible sigmoidoscopy: implications for colorectal cancer screening and instrument design. Endoscopy. 1999; 31:227–231.
Article26. Taghavi S, Jayarajan SN, Powers BD, Davey A, Willis AI. Examining rectal carcinoids in the era of screening colonoscopy: a surveillance, epidemiology, and end results analysis. Dis Colon Rectum. 2013; 56:952–959.27. Joosten E, Meeuwissen J, Vandewinckele H, Hiele M. Iron status and colorectal cancer in symptomatic elderly patients. Am J Med. 2008; 121:1072–1077.
Article28. Sawhney MS, Lipato T, Nelson DB, Lederle FA, Rector TS, Bond JH. Should patients with anemia and low normal or normal serum ferritin undergo colonoscopy? Am J Gastroenterol. 2007; 102:82–88.
Article29. Kishida T, Shinozawa I, Tanaka S, Hoshino T, Tatsuguchi A, Feng L, et al. Significance of serum iron and ferritin in patients with colorectal adenomas. Scand J Gastroenterol. 1997; 32:233–237.
Article30. Bird CL, Witte JS, Swendseid ME, Shikany JM, Hunt IF, Frankl HD, et al. Plasma ferritin, iron intake, and the risk of colorectal polyps. Am J Epidemiol. 1996; 144:34–41.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Early Detection of Pancreatic Cancer: Whom and How?
- Korean National Recommendation Guidelines on Screening and Surveillance for Early Detection of Colorectal Cancers
- Cost-Effectiveness Analysis of Colon Cancer Screening by Colonosopic Examination in Korea
- Colon Cancer Screening—Is It Necessary to Start under the Age of 50?
- Results of Colorectal Cancer Screening of the National Cancer Screening Program in Korea, 2008