Ann Surg Treat Res.
2018 Mar;94(3):154-158. 10.4174/astr.2018.94.3.154.
Bacterial infection monitoring in the early period after liver transplantation
- Affiliations
-
- 1Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. yjongman21@gmail.com
- 2Department of Surgery, Kyung Hee University Hospital at Gangdong, Kyung Hee University School of Medicine,Seoul, Korea.
- 3Critical Care Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 4Division of Infectious Diseases, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2405328
- DOI: http://doi.org/10.4174/astr.2018.94.3.154
Abstract
- PURPOSE
Infection remains the main cause of morbidity and mortality in liver transplantation (LT) recipients; however infection is notoriously difficult to diagnose because its usual signs and symptoms of infection may be masked or absent. This study comprises an analysis of bacterial infections in the early period after LT.
METHODS
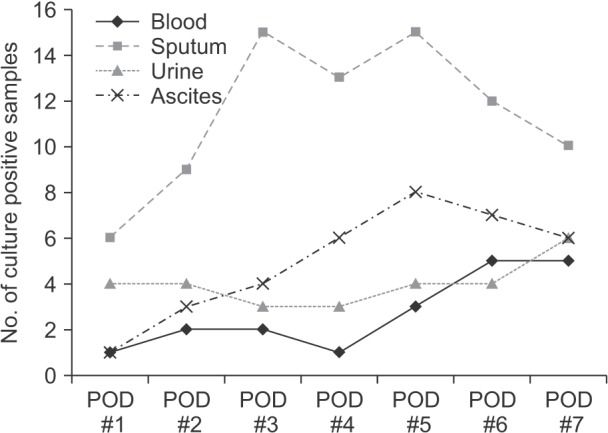
This is a study of 129 adults who underwent LT from January 2013 to December 2013, and it includes patients who were followed daily from the day of transplantation to 1-week posttransplantation using bacteriological cultures of blood, urine, sputum, and drained ascites.
RESULTS
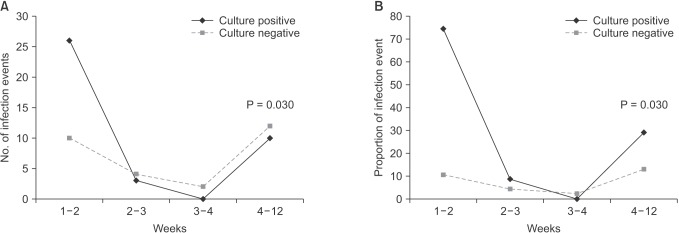
The following factors were significantly different between the positive and negative culture groups: living donor LT vs. deceased donor LT (odds ratio [OR], 3.269; P = 0.003), model for end-stage liver disease score (OR, 4.364; P < 0.001), and Child-Pugh classification (P = 0.007). Neither positive culture nor negative culture was associated with infection within 4 weeks of surgery (P = 0.03), and most events were due to surgical complications (75%).
CONCLUSION
Since the full effect of immunosuppression is not yet present during the first month after LT, we suggest that the number of bacterial culture test could be reduced such that they are performed every other day depending on patient's situation.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Clinical outcome of 1,000 consecutive cases of liver transplantation: a single center experience
Bong Jun Kwak, Dong Goo Kim, Jae Hyun Han, Ho Joong Choi, Si Hyun Bae, Young Kyoung You, Jong Young Choi, Seung Kew Yoon
Ann Surg Treat Res. 2018;95(5):267-277. doi: 10.4174/astr.2018.95.5.267.
Reference
-
1. Fishman JA. Infection in solid-organ transplant recipients. N Engl J Med. 2007; 357:2601–2614. PMID: 18094380.
Article2. Barkholt L, Ericzon BG, Tollemar J, Malmborg AS, Ehrnst A, Wilczek H, et al. Infections in human liver recipients: different patterns early and late after transplantation. Transpl Int. 1993; 6:77–84. PMID: 8447929.
Article3. Nicholson V, Johnson PC. Infectious complications in solid organ transplant recipients. Surg Clin North Am. 1994; 74:1223–1245. PMID: 7940071.
Article4. Snydman DR. Infection in solid organ transplantation. Transpl Infect Dis. 1999; 1:21–28. PMID: 11428968.
Article5. Lumbreras C, Lizasoain M, Moreno E, Aguado JM, Gomez R, Garcia I, et al. Major bacterial infections following liver transplantation: a prospective study. Hepatogastroenterology. 1992; 39:362–365. PMID: 1427585.6. Swoboda-Kopec E, Kawecki D, Wroblewska M, Krawczyk M, Luczak M. Epidemiology and susceptibility to antifungal agents of fungi isolated from clinical specimens from patients hospitalized in the Department of General and Liver Surgery of the Medical University of Warsaw. Transplant Proc. 2003; 35:2298–2303. PMID: 14529921.
Article7. Kim YJ, Kim SI, Jun YH, Choi JY, Yoon SK, You YK, et al. Clinical significance of surveillance culture in liver transplant recipients. Transplant Proc. 2014; 46:828–831. PMID: 24767358.
Article8. Kawecki D, Chmura A, Pacholczyk M, Lagiewska B, Adadynski L, Wasiak D, et al. Bacterial infections in the early period after liver transplantation: etiological agents and their susceptibility. Med Sci Monit. 2009; 15:CR628–CR637. PMID: 19946234.9. Kim JM, Kwon CH, Joh JW, Ha YE, Sinn DH, Choi GS, et al. Oral valganciclovir as a preemptive treatment for cytomegalovirus (CMV) infection in CMV-seropositive liver transplant recipients. PLoS One. 2015; 10:e0123554. PMID: 25942443.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Necrotizing Fasciitis following Liver Transplantation
- Simple Auxiliary Liver Transplantation without Bile Duct Reconstruction in the Rat
- Comparison of bacterial infection rate between patients with alcoholic liver cirrhosis and viral liver cirrhosis
- Early complication of liver transplantation in the intensive care unit
- Management of Hepatitis C Viral Infection Pre- and Post-liver Transplantation