Allergy Asthma Immunol Res.
2018 Mar;10(2):131-136. 10.4168/aair.2018.10.2.131.
Dyspnea Perception During Induced Bronchoconstriction Is Complicated by the Inhaled Methacholine in Children With Clinical Asthma
- Affiliations
-
- 1Department of Pediatrics, Yonsei University College of Medicine, Seoul, Korea.
- 2Department of Pediatrics, Seoul National University Hospital, Seoul, Korea. dongins0@snu.ac.kr
- 3Department of Pediatrics, Severance Children's Hospital, Seoul, Korea.
- KMID: 2402972
- DOI: http://doi.org/10.4168/aair.2018.10.2.131
Abstract
- PURPOSE
Dyspnea is not widely utilized as an indicator of asthma provocation despite its universal presentation. We hypothesized that dyspnea severity was proportionate with the lung function decline, methacholine dose-step, and the degree of bronchial hyperresponsiveness (BHR).
METHODS
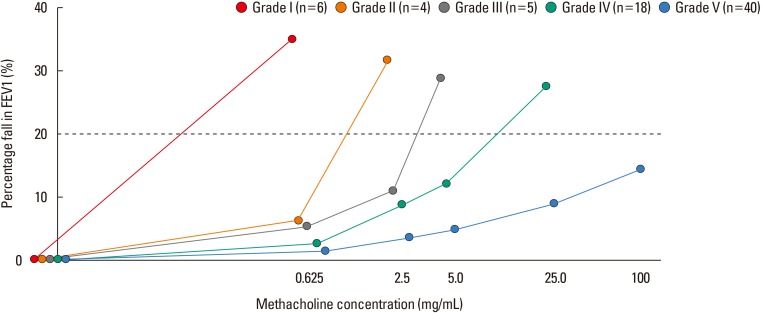
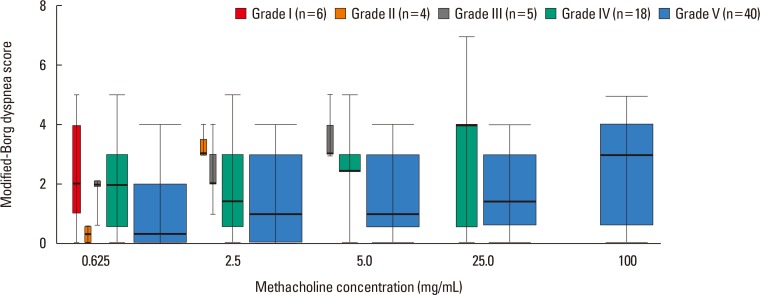
We retrospectively analyzed 73 children's bronchial provocation test data with an assessment of dyspnea at every dose-step. Dyspnea severity was scored using a modified Borg (mBorg) scale. A linear mixed effect analysis was performed to evaluate the relationship between the mBorg scale, the percentage fall in the forced expiratory volume in 1 second (FEV1) (ΔFEV1%), the methacholine dose-step, and the degree of BHR (BHR grade).
RESULTS
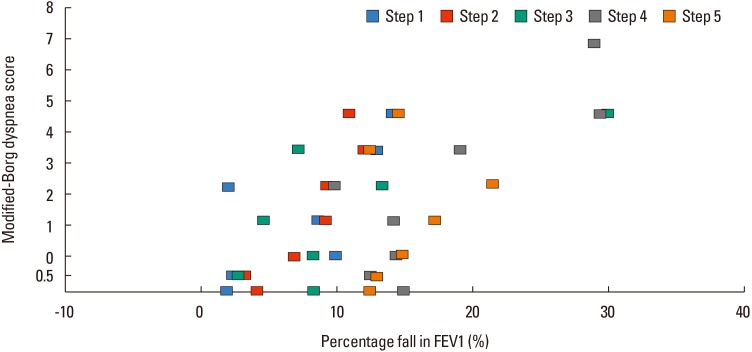
Subjects were divided into 5 BHR groups based on their last methacholine dose-steps. The mBorg scores did not differ significantly among BHR groups (P=0.596, Kruskal-Wallis test). The linear mixed effect analysis showed that ΔFEV1% was affected by the methacholine dose-step (P < 0.001) and BHR grade (P < 0.001). The mBorg score was affected by the dose-step (P < 0.001) and BHR grade (P=0.019). We developed a model to predict the mBorg score and found that it was affected by the methacholine dose-step and ΔFEV1%, elevating it by a score of 0.039 (χ² [1]=21.06, P < 0.001) and 0.327 (χ² [1]=47.45, P < 0.001), respectively. A significant interaction was observed between the methacholine dose-step and ΔFEV1% (χ² [1]=16.20, P < 0.001).
CONCLUSIONS
In asthmatic children, inhaled methacholine, as well as the degree of BHR and lung function decline, may affect dyspnea perception during the bronchial provocation test. If we wish to draw meaningful information from dyspnea perception, we have to consider various complicating factors underlying it.
Keyword
MeSH Terms
Figure
Reference
-
1. Banzett RB, Mulnier HE, Murphy K, Rosen SD, Wise RJ, Adams L. Breathlessness in humans activates insular cortex. Neuroreport. 2000; 11:2117–2120. PMID: 10923655.
Article2. Fitzgerald JM, Hargreave FE. Acute asthma: emergency department management and prospective evaluation of outcome. CMAJ. 1990; 142:591–595. PMID: 1968778.3. Parente AA, March MF, Evangelista LA, Cunha AL. Perception of dyspnea in childhood asthma crisis by the patients and those in charge of them. J Pediatr (Rio J). 2011; 87:541–546. PMID: 22170258.
Article4. Boushey HA, Holtzman MJ, Sheller JR, Nadel JA. Bronchial hyperreactivity. Am Rev Respir Dis. 1980; 121:389–413. PMID: 6987924.5. Rosenthal RR, Norman PS, Summer WR, Permutt S. Role of the parasympathetic system in antigen-induced bronchospasm. J Appl Physiol Respir Environ Exerc Physiol. 1977; 42:600–606. PMID: 863822.
Article6. Crapo RO, Casaburi R, Coates AL, Enright PL, Hankinson JL, Irvin CG, et al. Guidelines for methacholine and exercise challenge testing-1999. This official statement of the American Thoracic Society was adopted by the ATS Board of Directors, July 1999. Am J Respir Crit Care Med. 2000; 161:309–329. PMID: 10619836.7. Baker RR, Mishoe SC, Zaitoun FH, Arant CB, Lucas J, Rupp NT. Poor perception of airway obstruction in children with asthma. J Asthma. 2000; 37:613–624. PMID: 11059529.
Article8. Motomura C, Odajima H, Tezuka J, Harada J, Okada K, Nishima S. Perception of dyspnea during acetylcholine-induced bronchoconstriction in asthmatic children. Ann Allergy Asthma Immunol. 2009; 102:121–124. PMID: 19230462.
Article9. Panditi S, Silverman M. Perception of exercise induced asthma by children and their parents. Arch Dis Child. 2003; 88:807–811. PMID: 12937106.
Article10. Kim YS, Shin JM, Choi YJ, Suh DI, Koh YY. Comparison on the profiles of the two dyspnea score during an induced bronchoconstriction in children with clinical asthma. Allergy Asthma Respir Dis. 2017; 5:262–269.11. Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardisation of spirometry. Eur Respir J. 2005; 26:319–338. PMID: 16055882.12. Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982; 14:377–381. PMID: 7154893.
Article13. Khan FI, Reddy RC, Baptist AP. Pediatric Dyspnea Scale for use in hospitalized patients with asthma. J Allergy Clin Immunol. 2009; 123:660–664. PMID: 19181371.
Article14. Lunneborg CE. Jonckheere–Terpstra test. In : . Hoboken (NJ): John Wiley & Sons;2014.15. Bates D, Mächler M, Bolker BM, Walker SC. Fitting linear mixed-effects models using lme4. J Stat Softw. 2015; 67:1–48.16. Avital A, Bar-Yishay E, Springer C, Godfrey S. Bronchial provocation tests in young children using tracheal auscultation. J Pediatr. 1988; 112:591–594. PMID: 3280772.
Article17. Lansing RW, Gracely RH, Banzett RB. The multiple dimensions of dyspnea: review and hypotheses. Respir Physiol Neurobiol. 2009; 167:53–60. PMID: 18706531.
Article18. Tosca MA, Silvestri M, Olcese R, Pistorio A, Rossi GA, Ciprandi G. Breathlessness perception assessed by visual analogue scale and lung function in children with asthma: a real-life study. Pediatr Allergy Immunol. 2012; 23:537–542. PMID: 22625869.
Article19. Ciprandi G, Schiavetti I, Sorbello V, Ricciardolo FL. Perception of asthma symptoms as assessed on the visual analog scale in subjects with asthma: a real-life study. Respir Care. 2016; 61:23–29. PMID: 26420899.
Article20. Burdon JG, Juniper EF, Killian KJ, Hargreave FE, Campbell EJ. The perception of breathlessness in asthma. Am Rev Respir Dis. 1982; 126:825–828. PMID: 7149447.21. Chetta A, Castagnaro A, Foresi A, Del Donno M, Pisi G, Malorgio R, et al. Assessment of breathlessness perception by Borg scale in asthmatic patients: reproducibility and applicability to different stimuli. J Asthma. 2003; 40:323–329. PMID: 12807177.
Article22. Cato Study Group. Nuijsink M, Hop WC, Jongste JC, Sterk PJ, Duiverman AE. Perception of bronchoconstriction: a complementary disease marker in children with asthma. J Asthma. 2013; 50:560–564. PMID: 23672570.
Article23. Boulet LP, Leblanc P, Turcotte H. Perception scoring of induced bronchoconstriction as an index of awareness of asthma symptoms. Chest. 1994; 105:1430–1433. PMID: 8181331.
Article24. Turcotte H, Corbeil F, Boulet LP. Perception of breathlessness during bronchoconstriction induced by antigen, exercise, and histamine challenges. Thorax. 1990; 45:914–918. PMID: 2281422.
Article25. van Gent R, van Essen-Zandvliet LE, Rovers MM, Kimpen JL, de Meer G, van der Ent CK. Poor perception of dyspnoea in children with undiagnosed asthma. Eur Respir J. 2007; 30:887–891. PMID: 17652315.
Article26. Yoos HL, McMullen A. Symptom perception and evaluation in childhood asthma. Nurs Res. 1999; 48:2–8. PMID: 10029396.
Article27. Fritz GK, McQuaid EL, Spirito A, Klein RB. Symptom perception in pediatric asthma: relationship to functional morbidity and psychological factors. J Am Acad Child Adolesc Psychiatry. 1996; 35:1033–1041. PMID: 8755800.
Article28. Won YK, Hwang TH, Roh EJ, Chung EH. Seasonal patterns of asthma in children and adolescents presenting at emergency departments in Korea. Allergy Asthma Immunol Res. 2016; 8:223–229. PMID: 26922932.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Comparative Study between External Resistive Loads to Breathing and Induced Bronchoconstriction on Dyspnea Perception in Asthma
- A Comparative Study between External Resistive Loads to Breathing and Induced Bronchoconstriction on Dyspnea Perception in Asthma
- The effect of deep inspiration on methacholine induced bronchoconstriction
- Differences of Ventilatory Function Measurements between Natural and Methacholine or Histamine-induced Bronchoconstriction in Asthma
- Exercise induced delayed bronchoconstriction in children with asthma