Ann Rehabil Med.
2017 Dec;41(6):1082-1087. 10.5535/arm.2017.41.6.1082.
Bulbar Myasthenia Gravis Superimposed in a Medullary Infarction Diagnosed by a Fiberoptic Endoscopic Evaluation of Swallowing With Simultaneous Tensilon Application
- Affiliations
-
- 1Department of Rehabilitation Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea. lafolia@catholic.ac.kr
- KMID: 2400294
- DOI: http://doi.org/10.5535/arm.2017.41.6.1082
Abstract
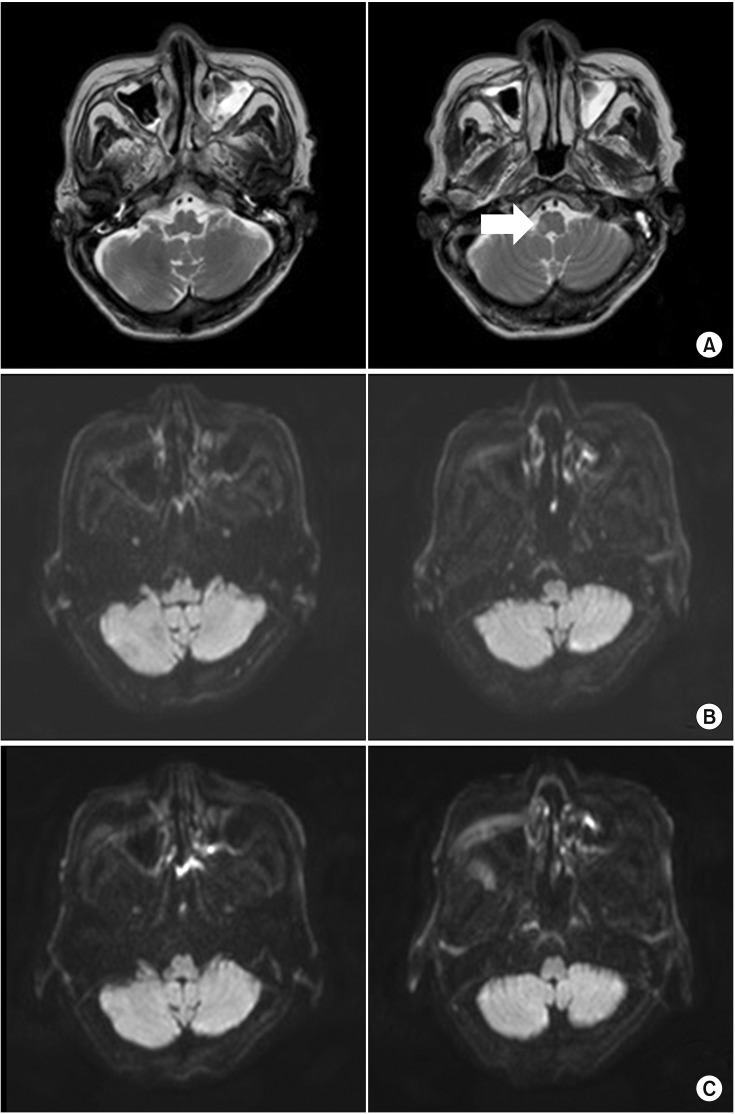
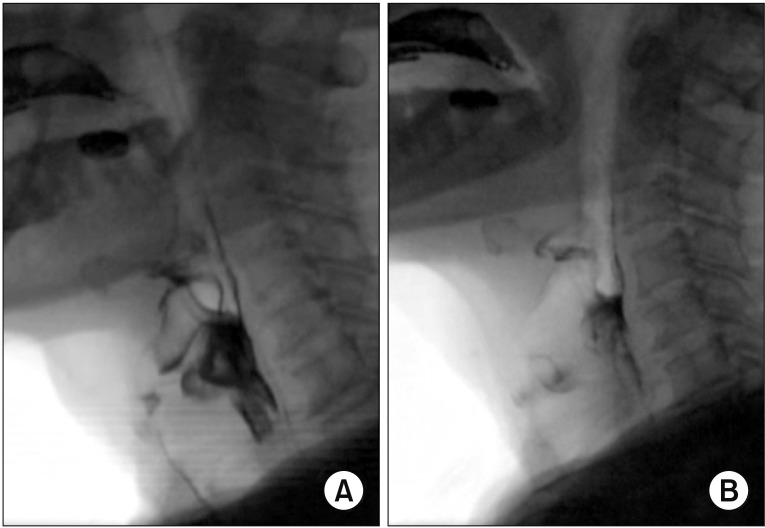
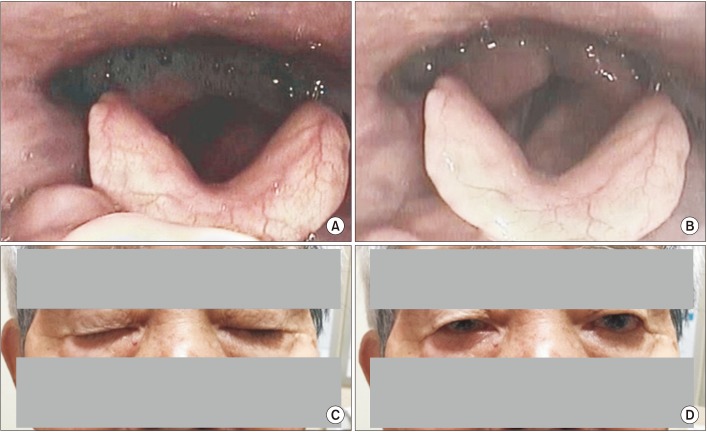
- In the elderly, myasthenia gravis (MG) can present with bulbar symptoms, which can be clinically difficult to diagnose from other neurological comorbid conditions. We describe a case of a 75-year-old man who had been previously diagnosed with dysphagia associated with medullary infarction but exhibited aggravation of the dysphagia later on due to a superimposed development of bulbar MG. After recovering from his initial swallowing difficulties, the patient suddenly developed ptosis, drooling, and generalized weakness with aggravated dysphagia. Two follow-up brain magnetic resonance imaging (MRI) scans displayed no new brain lesions. Antibodies to acetylcholine receptor and muscle-specific kinase were negative. Subsequent electrodiagnosis with repetitive nerve stimulation tests revealed unremarkable findings. A diagnosis of bulbar MG could only be established after fiberoptic endoscopic evaluation of swallowing (FEES) with simultaneous Tensilon application. After application of intravenous pyridostigmine, significant improvement in dysphagia and ptosis were observed both clinically and according to the FEES.
Keyword
MeSH Terms
-
Acetylcholine
Aged
Antibodies
Brain
Deglutition Disorders
Deglutition*
Diagnosis
Edrophonium*
Electrodiagnosis
Fees and Charges
Follow-Up Studies
Humans
Infarction*
Magnetic Resonance Imaging
Myasthenia Gravis*
Phosphotransferases
Pyridostigmine Bromide
Sialorrhea
Stroke
Acetylcholine
Antibodies
Edrophonium
Phosphotransferases
Pyridostigmine Bromide
Figure
Reference
-
1. Vincent A, Clover L, Buckley C, Grimley Evans J, Rothwell PM. UK Myasthenia Gravis Survey. Evidence of underdiagnosis of myasthenia gravis in older people. J Neurol Neurosurg Psychiatry. 2003; 74:1105–1108. PMID: 12876244.
Article2. Sathasivam C. Diagnosis and management of myasthenia gravis. Prog Neurol Psychiatry. 2014; 18:6–14.
Article3. Warnecke T, Teismann I, Zimmermann J, Oelenberg S, Ringelstein EB, Dziewas R. Fiberoptic endoscopic evaluation of swallowing with simultaneous Tensilon application in diagnosis and therapy of myasthenia gravis. J Neurol. 2008; 255:224–230. PMID: 18217186.
Article4. Basiri K, Ansari B, Okhovat AA. Life-threatening misdiagnosis of bulbar onset myasthenia gravis as a motor neuron disease: How much can one rely on exaggerated deep tendon reflexes. Adv Biomed Res. 2015; 4:58. PMID: 25802827.
Article5. Vincent A, McConville J, Farrugia ME, Newsom-Davis J. Seronegative myasthenia gravis. Semin Neurol. 2004; 24:125–133. PMID: 15229799.
Article6. Kleiner-Fisman G, Kott HS. Myasthenia gravis mimicking stroke in elderly patients. Mayo Clin Proc. 1998; 73:1077–1078. PMID: 9818042.7. Libman R, Benson R, Einberg K. Myasthenia mimicking vertebrobasilar stroke. J Neurol. 2002; 249:1512–1514. PMID: 12420089.
Article8. Aarli JA. Myasthenia gravis in the elderly: is it different? Ann N Y Acad Sci. 2008; 1132:238–243. PMID: 18567874.9. O'Riordan J, Javed M, Doherty C, Hutchinson M. Worsening of myasthenia gravis on treatment with imipenem/cilastatin. J Neurol Neurosurg Psychiatry. 1994; 57:383.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Response to Low Rate Stimulation of Repetitive Nerve Stimulation Test after Intravenous Tensilon Injection on Patients With Myasthenia Gravis
- Fecal Incontinence as a Symptom of Myasthenia Gravis
- Pathological Findings of Tumors at Thymus and Myasthenia Gravis
- Tensilon Tonometry in Diagnosis of Myasthenia Gravis
- Myasthenia Gravis, Schizophrenia, and Colorectal Cancer in A Patient: Long-Term Follow-Up with Medication Complexity