Ann Dermatol.
2018 Feb;30(1):41-46. 10.5021/ad.2018.30.1.41.
Terminal Deoxynucleotidyl Transferase-Mediated Deoxyuridine Triphosphate Nick End Labeling (TUNEL) Assay to Characterize Histopathologic Changes Following Thermal Injury
- Affiliations
-
- 1Department of Dermatology, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea. kumcihk@korea.ac.kr
- KMID: 2399753
- DOI: http://doi.org/10.5021/ad.2018.30.1.41
Abstract
- BACKGROUND
Despite the wide application of lasers and radiofrequency (RF) surgery in dermatology, it is difficult to find studies showing the extent of damage dependent on cell death.
OBJECTIVE
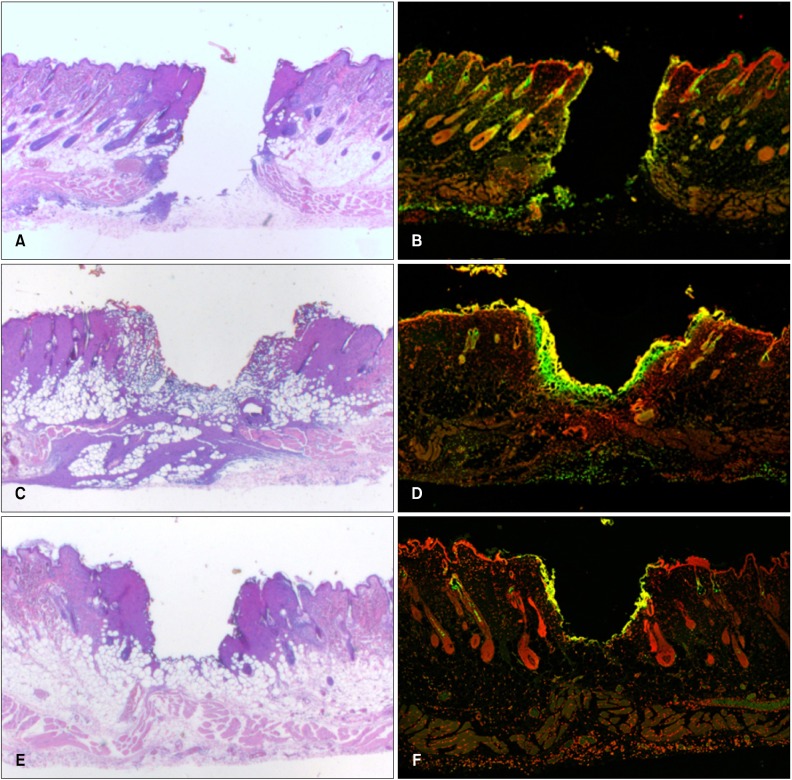
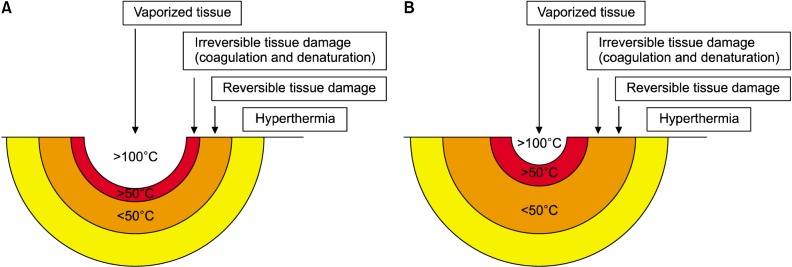
We evaluated histopathologic changes following in vivo thermal damage generated by CO2 laser, 1,444 nm long-pulsed neodymium:yttrium-aluminum-garnet (LP Nd:YAG) laser and RF emitting electrosurgical unit.
METHODS
Thermal damage was induced by the above instruments on ventral skin of rat. Specimens were stained with hematoxylin and eosin, along with a terminal deoxynucleotidyl transferase-mediated deoxyuridine triphosphate nick end labeling (TUNEL) assay, to highlight the degree of irreversible cellular injury.
RESULTS
The volume of vaporization was largest with the CO2 laser. Area of cell death area identified by TUNEL assay, when arranged from widest to narrowest, was 1,444 nm LP Nd:YAG laser, CO2 laser, and RF emitting electrosurgical unit.
CONCLUSION
This histopathologic evaluation of the acute characterization of injury across devices may be advantageous for attaining better treatment outcomes.
Keyword
MeSH Terms
Figure
Reference
-
1. Schoinohoriti OK, Chrysomali E, Tzerbos F, Iatrou I. Comparison of lateral thermal injury and healing of porcine skin incisions performed by CO2-laser, monopolar electrosurgery and radiosurgery: a preliminary study based on histological and immunohistochemical results. Int J Dermatol. 2012; 51:979–986. PMID: 22788819.
Article2. Gavrieli Y, Sherman Y, Ben-Sasson SA. Identification of programmed cell death in situ via specific labeling of nuclear DNA fragmentation. J Cell Biol. 1992; 119:493–501. PMID: 1400587.
Article3. Ansari B, Coates PJ, Greenstein BD, Hall PA. In situ end-labelling detects DNA strand breaks in apoptosis and other physiological and pathological states. J Pathol. 1993; 170:1–8. PMID: 8326456.
Article4. Schemmel M, Haefner HK, Selvaggi SM, Warren JS, Termin CS, Hurd WW. Comparison of the ultrasonic scalpel to CO2 laser and electrosurgery in terms of tissue injury and adhesion formation in a rabbit model. Fertil Steril. 1997; 67:382–386. PMID: 9022618.
Article5. Courey MS, Fomin D, Smith T, Huang S, Sanders D, Reinisch L. Histologic and physiologic effects of electrocautery, CO2 laser, and radiofrequency injury in the porcine soft palate. Laryngoscope. 1999; 109:1316–1319. PMID: 10443841.6. Sinha UK, Gallagher LA. Effects of steel scalpel, ultrasonic scalpel, CO2 laser, and monopolar and bipolar electrosurgery on wound healing in guinea pig oral mucosa. Laryngoscope. 2003; 113:228–236. PMID: 12567074.
Article7. Basterra J, Zapater E, Moreno R, Hernández R. Electrosurgical endoscopic cordectomy with microdissection electrodes: a comparative study with CO2 laser. J Laryngol Otol. 2006; 120:661–664. PMID: 16719953.
Article8. Silverman EB, Read RW, Boyle CR, Cooper R, Miller WW, McLaughlin RM. Histologic comparison of canine skin biopsies collected using monopolar electrosurgery, CO2 laser, radiowave radiosurgery, skin biopsy punch, and scalpel. Vet Surg. 2007; 36:50–56. PMID: 17214820.9. Zapater E, Frías S, Pérez A, Basterra J. Comparative study on chronic tissue damage after cordectomies using either CO2 laser or microdissection electrodes. Head Neck. 2009; 31:1477–1481. PMID: 19378326.10. Stelter K, de la Chaux R, Patscheider M, Olzowy B. Double-blind, randomised, controlled study of post-operative pain in children undergoing radiofrequency tonsillotomy versus laser tonsillotomy. J Laryngol Otol. 2010; 124:880–885. PMID: 20380764.
Article11. Schoinohoriti OK, Chrysomali E, Iatrou I, Perrea D. Evaluation of lateral thermal damage and reepithelialization of incisional wounds created by CO2-laser, monopolar electrosurgery, and radiosurgery: a pilot study on porcine oral mucosa. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012; 113:741–747. PMID: 22677020.
Article12. Kelly KJ, Sandoval RM, Dunn KW, Molitoris BA, Dagher PC. A novel method to determine specificity and sensitivity of the TUNEL reaction in the quantitation of apoptosis. Am J Physiol Cell Physiol. 2003; 284:C1309–C1318. PMID: 12676658.13. Taheri A, Mansoori P, Sandoval LF, Feldman SR, Pearce D, Williford PM. Electrosurgery: part II. Technology, applications, and safety of electrosurgical devices. J Am Acad Dermatol. 2014; 70:607.e1–607.e12. quiz 619-620. PMID: 24629362.14. Tark KC, Jung JE, Song SY. Superior lipolytic effect of the 1,444 nm Nd:YAG laser: comparison with the 1,064 nm Nd:YAG laser. Lasers Surg Med. 2009; 41:721–727. PMID: 20014250.15. Jung SK, Jang HW, Kim HJ, Lee SG, Lee KG, Kim SY, et al. A prospective, long-term follow-Up study of 1,444 nm Nd:YAG laser: a new modality for treating axillary bromhidrosis. Ann Dermatol. 2014; 26:184–188. PMID: 24882972.
Article16. Lee KG, Kim SA, Yi SM, Kim JH, Kim IH. Subdermal coagulation treatment of axillary bromhidrosis by 1,444 nm Nd:YAG laser: a comparison with surgical treatment. Ann Dermatol. 2014; 26:99–102. PMID: 24648694.
Article17. Min KH, Kim JH, Park HJ, Chung HS, Heo CY. The skin-tightening effects of 1,444-nm Nd:YAG laser on human skin: an in vivo study. Aesthetic Plast Surg. 2014; 38:585–591. PMID: 24788857.
Article18. Lee SH, Roh MR, Jung JY, Jee H, Nam KA, Chung KY. Effect of subdermal 1,444-nm pulsed neodymium-doped yttrium aluminum garnet laser on the nasolabial folds and cheek laxity. Dermatol Surg. 2013; 39:1067–1078. PMID: 23815313.
Article19. Lee SH, Jung JY, Roh MR, Chung KY. Treatment of lipomas using a subdermal 1,444-nm micropulsed neodymiumdoped yttrium aluminum garnet laser. Dermatol Surg. 2011; 37:1375–1376. PMID: 22988996.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Placental Apoptosis in Preeclampsia
- Apoptosis of Alveolar Cells in Pneumocystis Carinii Pneumonia: Application of Electron Microscopic Terminal Deoxynucleotidyl Transferase-Mediated dUTP-Biotin Nick End Labeling Method
- Placental apoptosis in preeclampsia
- Study on the Apoptosis and its Mediators in the Placentas of Preclampsia using cDNA Expression Array
- Trophoblast Apoptosis and BRCA1 Expression in Fetal Growth Restriction Pregnancy